Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
Mohmmed Al-Zuidi , Kenni Lotter Mrtin Mrshll ,Mikhil Lozinskiy
a Department of Urology, Royal Perth Hospital, Perth, Australia
b Department of Radiology, Royal Perth Hospital, Perth, Australia
KEYWORDS Radiofrequency ablation;Small renal tumour;Hydrodissection;Renal cell carcinoma
Abstract Objective: This study aimed to evaluate the safety and efficacy outcomes of percutaneous radiofrequency ablation (RFA) for localised renal cell carcinoma (RCC) in a tertiary hospital patient who remained unfit for surgical intervention.Methods: We retrospectively analysed survival outcomes for patients with biopsy proven RCC treated by RFA at Royal Perth Hospital between September 2009 and May 2018.Complication data were gathered for all patients that underwent renal RFA along with 2- and 5-year recurrence-free survival (RFS) rate and compared the outcomes with data from previous studies.Results: A total of 69 patients (73 procedures) were eligible for the study, and those patients had biopsy-proven RCC with a minimum of 2-year follow-up.The complication rate was 8.2% (6/73) and local recurrence rate 9.6% (7/73).Two-year RFS is 95.7% and 5-year RFS is 78.8% on a median 3.82-year follow-up (interquartile range 1.90—5.75 years).Conclusion: RFA performed at our centre was found to be safe and effective with low complication rates and durable RFS in line with expectations from existing research.Our study demonstrated that RFA is an alternative modality of treatment for small renal tumours in patients unfit for surgical approach.
1.Introduction
Small renal masses are being detected more regularly,owing partly to increased use of computed tomography(CT)scanning as well as lifestyle associated factors such as obesity[1].The management of these has been an evolving field of contemporary medicine, including surveillance,surgical resection, and thermal ablation.
Renal cancer was the seventh most commonly diagnosed cancer in Australia in 2016 [2] with an age-standardised incidence rate of 13 cases per 100 000 persons [2].In 2018, the age-standardised mortality rate was 2.9 deaths per 100 000 persons; however, from 2012 to 2016 5-year survival increased from 51% to 79% [2] owing to advance in detection and management.For many years, radical nephrectomy was considered the “gold standard” of treatment for localised renal cell carcinoma (RCC).However, it has been reported that a significant number of patients who are rendered with a single kidney after radical nephrectomy are under increased risk of developing chronic kidney disease [3,4].Recent advances in surgical techniques have brought the use of a nephron sparing surgery which includes an open, laparoscopic, and robot-assisted laparoscopic partial nephrectomy as radical nephrectomy was considered as overtreating small renal tumours.However, some patients are unfit for surgery from comorbidity point of view or patients request no surgical approach for small renal tumours.Therefore, advancements into ablative modalities in treating small renal tumours have expanded considerably with the use of cryoablation, radiofrequency ablation (RFA), high-intensity focused ultrasound, and microwave thermotherapy.
RFA is a novel minimally invasive treatment approach to the management of small renal tumours.International studies have shown that RFA is a safe[5—8]nephron sparing treatment [6] for small (<4 cm) [9] RCC.Due to lack of long-term follow-up, there has been some hesitancy to use RFA as first-line management.However, more recent comparative studies have identified that in appropriately selected populations RFA has comparable recurrence rates during interval follow-up compared to partial nephrectomy[7];this is of particular interest for patients who may not be a suitable candidate to undergo surgical management.There has been a lack of data regarding RFA within Australian populations and certain age and comorbid subgroups.
This cohort aimed to compare safety and efficacy outcomes of percutaneous RFA for localised RCC performed in outpatient setting at Royal Perth Hospital with available data in patients who remained unfit for surgical intervention or requested to have RFA of the renal tumour.
Herein, we report our centre’s experience with RFAs of small renal tumours in the management of 69 patients over a follow-up time of at least 2 years.
2.Methods
This cohort has been approved by Western Australia Health Governance, Evidence, Knowledge and Outcome (GEKO)committee (approval number QA35804) to retrospectively study 69 patients (73 procedures) treated with percutaneous RFA from September 2009 to May 2018 at Royal Perth Hospital.The study excluded non-eligible patients who did not have preprocedure biopsy,lost follow-up prior to 2 years or patients who underwent the procedure out of Royal Perth Hospital, as pathologic confirmation would provide an accurate treatment and follow-up plan,reduce over-estimation of the treatment effectiveness,and minimize unnecessary follow-up [10].All the patients were followed up for at least 2 years following the RFA procedures and all had pre-procedural imaging and biopsy to confirm RCC.Each patient was reviewed by a urologist, and all methods have been carried out in accordance with relevant guidelines and regulations.Ethical approval body has approved data collection and publishing.Informed consents were obtained from individuals and from the committee as this research involves human participants.
All the procedures were performed under general anaesthesia in either prone position (mostly), supine, left lateral, or right lateral positions based on tumour site.The procedures were CT-guided with a percutaneous approach with occasional use of hydrodissection with dextrose 5% in water to displace bowel or adjacent structures to approach the tumour precisely with no major technical difficulties.The centre’s recommended follow-up was at 6 months post procedure,then at 12 months,and then yearly at least for 2 years for all patient to meet European Association of Urology guidelines [11].
No renal function included in this study,as no significant renal dysfunction noted in comparison to the preprocedural baseline.
The statistical analysis and calculation were performed using standard definition.
3.Results
RFA was performed at 73 sessions in 69 patients, with a procedural success in 67 out of 73(91.8%)and no immediate complications.Mean age of patients at the time of RFA procedure was 68 years (range 47—89 years).Males accounted for 59.4% (41 patients) and female for 40.6%(28 patients).Median tumour size, which was ablated, was 3.2 cm (range 1.2—5.2 cm).Majority of tumours (n=69)were less than or equal to 4 cm and only four tumours of more than 4 cm in size were ablated (those were done at earlier stages prior to the latest recommendations [5]).
Table 1 and Table 2 demonstrate patients’demographics and tumour details.Clinical indications for RFA for patients included in this audit include coexisting comorbidities,solitary kidney, and patient preference (Table 3).

Table 3 Indications for choosing percutaneous radio-frequency ablation over surgical approach.
Tumour location was classified as upper, interpolar, or lower pole in either left or right side.One patient had the tumour in his solitary pelvic tumour.Left kidney tumours accounted for 56.2% (n=41) and right kidney tumours for 42.5% (n=31) of cases.Upper, interpolar, and lower tumours were 17.8%,45.2%,and 37.0%of cases,respectively.Median ablation time was 14 min (range: 4—24 min) and majority of ablations were done by either single burn(n=37) or two burns (n=29).
Complications occurred after procedural completion were documented in six out of 73 RFA procedures (8.2%),included perirenal or retroperitoneal hematoma, contrast extravasation, and pneumothorax (Table 4).
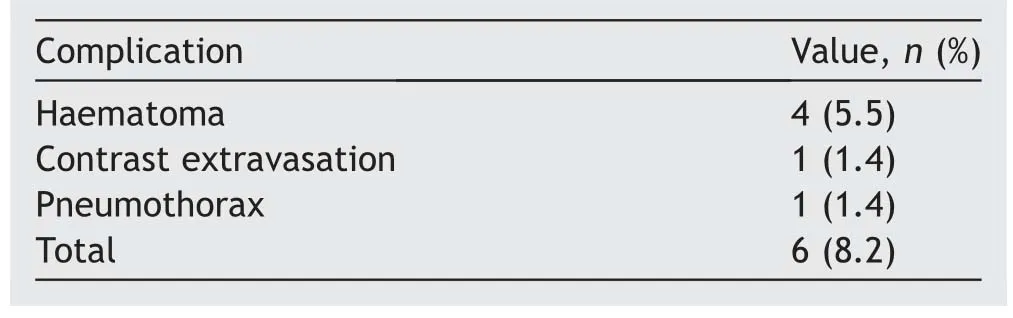
Table 4 Radiofrequency ablation complication in our cohort.
All 69 patients underwent pre-RFA renal tumour biopsy to confirm RCC prior as part of the inclusion criteria.RCC subtypes were mainly clear cell RCC (79.7%), while papillary RCC comprised 19.0% and chromophobe RCC 1.3%.
This study demonstrated that technical success was achieved in 67 of 73 procedures (91.8%), as we had seven local recurrences during surveillance;four patients of them had local recurrences during the first 2 years of surveillance, and they were treated with re-RFA of the same lesion with no further recurrences.Other three patients with local recurrences at 6,13,and 36 months were treated with either partial or radical nephrectomy (Table 5).Only one patient developed distant metastasis to para-aortic lymph nodes and lungs at 4 months follow-up CT scan who was referred to medical oncology.
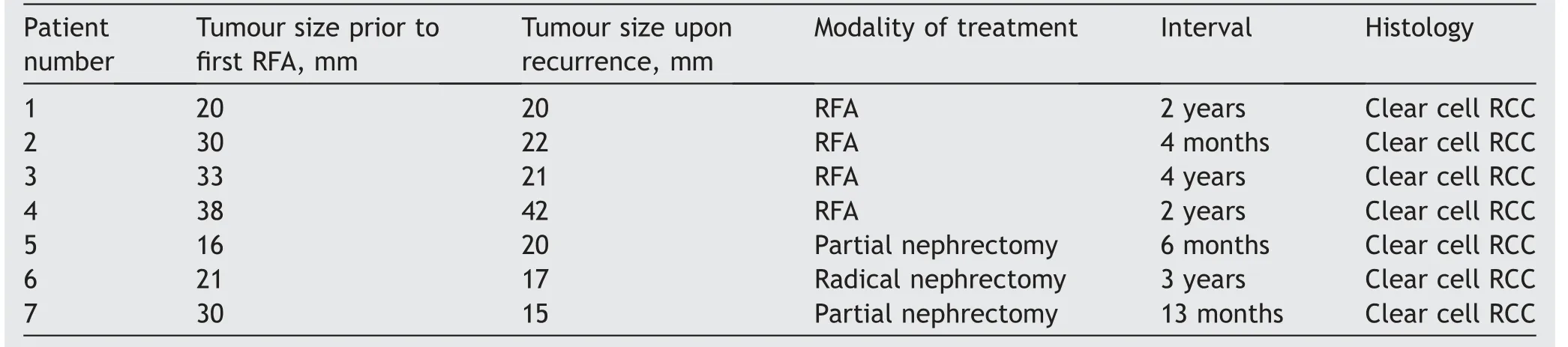
Table 5 Recurrent renal tumour after the first ablation details.
Median follow-up time was 3.82 years(interquartile range 1.90—5.75 years).Two-year recurrence-free survival rate was 95.7% (in 66 patients), while 5-year recurrence-free survival rate was 78.8%(in 26 out of 33 patients who reached the 5-year follow-up)compared to disease-free survival rate of 91.7% in robotic-assisted partial nephrectomy over 84 months of surveillance [12].
4.Discussion
Prior to the advancement of radiological interventions for a long list of indications,radical nephrectomy was considered to be the gold standard treatment for RCC confined to the kidney and it was considered to be the only curative option.As there is a reasonable proportion of patients who are unfit for surgery due to coexisting medical conditions, extensive surgical background, or patients who refuse to have surgeries, there should be a modality of treatment which can be offered to those patients to improve outcome and achieve an alternative curable measure or at least offer the best nephron sparing approach in patient with renal insufficiency.Since Zlotta et al.[13] initially described the clinical application of RFA in human RCC in 1997, many authors have been reporting favourable experiences on RFA for small renal tumours.
A successful RFA outcome has been associated with multiple factors including tumour size,location,impedance of tissue,and ablation time as well as the amount of energy delivered and surface area of the electrodes [10].Mylona et al.[14] reported a complete response of 85.7% for tumours less than 3 cm after the first RFA session but reported a noticeably lower response rate with tumours greater than 5 cm in size.Tumours greater than 3 cm were technically challenging to completely ablate on the initial attempt and required multiple overlapping ablation techniques.Therefore, smaller renal tumours are ideal candidates to obtain complete responses for the first RFA session.
Tumour location is another factor that may influence ablative outcome.It is reported that tumours adjacent to large vessels will suffer a “heat sink”, in which a regional vascular flow reduces the extent of the thermally induced coagulation [14,15].By contrast, the ablative effect of exophytic tumours is higher,as they are easy to target with an RFA probe and because the insulating effect of surrounding perirenal fat allows for higher temperatures during RFA [15,16].At our centre, we used hydrodissection with 5% dextrose in water to dissect the colon away from the kidney to protect it prior to targeting the tumours.
This retrospective cohort demonstrated that technical success was within the range of previously reported technical success rate of initial RFA (90%—100%) [17].Similarly, the local recurrence rate is comparable with existing data (0%—11.1%) [15,18,19].All recurrences, in our study,were diagnosed radiologically without repeating biopsy as the lesion increased in size or enhancement was suggestive of residual tumour or recurrence.Re-biopsy post RFA is not recommended as early post-ablative biopsy is not reliable in the absence of radiological evidence of recurrence [20].
We had a low complication profile (six of 73 procedures,8.2%) [19,21].Four patients developed bleeding or haematoma; one patient developed contrast extravasation; and one patient had pneumothorax.All patients were treated conservatively (Clavien-Dindo Grade I or II only) [22,23].
By comparison with existing literature, we can confirm that RFA for T1 renal tumours performed at Royal Perth Hospital over the past decade has been a safe and well tolerated procedure with curative outcome and a complication rate that is expected when compared to benchmark outcome data.
The data are limited by the available follow-up data and variable follow-up intervals.Only 33 of 69 patients completed the 5-year follow-up which contributes to 47.8%of patients.However, 66 of 69 patients (95.7%) completed the 2-year surveillance.
Despite this limitation, the RFA has shown its therapeutic potentiality for T1 renal tumours at Royal Perth Hospital as a treatment option for patients who have comorbidities with high risk for surgery or anaesthesia or for patients who prefer non-surgical approach.
5.Conclusion
There is evidence from the literature that RFA of renal tumours is a valuable option for treatment of renal cancers especially for patients who are unfit for surgery or those who refuse to have a radical surgical intervention.This audit of local practice at Royal Perth Hospital demonstrates that RFA has a low recurrence rate and a low complication rate which is consistent with expectations based on available data.This indicates that, as offered at Royal Perth Hospital, the procedure is a safe and effective treatment measure for small renal tumours and should be considered as an option upon discussion with patients.
Author contributions
Study concept and design: Mohammed Al-Zubaidi.
Data acquisition: Mohammed Al-Zubaidi.
Data analysis: Mohammed Al-Zubaidi, Kennia Lotter.
Drafting of manuscript: Mohammed Al-Zubaidi, Kennia Lotter.Critical revision of manuscript: Mikhail Lozinskiy, Martin Marshall.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Antioxidant status in patients with bladder cancer regarding cancer stage and grade
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Analysis of the effect of holmium laser flexible ureteroscopic intrapelvic drainage in the treatment of parapelvic renal cysts
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
