Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
Akif Memmedoglu Bairov
Department of Urology, Azerbaijan Medical University, Azerbaijan, Baku, Azerbaijan
KEYWORDS Hydronephrosis;Hydroureteronephrosis;Ureteropelvic obstruction;Dismembered pyeloplasty;Ureterovesical obstruction;Subadventitial resection of the ureter
Abstract Objective: The aim of our study was to examine results of pyeloplasty using the new method—subadventitial resection of the ureter with preservation of the ureteral artery proposed by us and the possibility of using this method in one-stage surgery with ureteropelvic junction (UPJ) and ureterovesical junction (UVJ) obstructions or vesicoureteral reflux.Methods: A retrospective analysis of 108 patients with hydronephrosis (including two patients with hydroureteronephrosis) who received treatment from March 1998 to March 2020 was carried out,with an average follow-up period of 36 months.Dismembered pyeloplasty using a subadventitial technique with preservation of ureteral blood supply was performed in 108 patients(including bilateral in two cases).In one patient with UPJ and UVJ obstructions and in one patient with UPJ obstruction and vesicoureteral reflux subadventitial resection of the ureter were performed in both segments.Results: All patients managed to preserve the integrity of the ureteral artery during dismembered pyeloplasty, and two patients simultaneously underwent ureterocystostomy by subadventitial resection of the ureter.The method of pyeloureteroplasty with subadventitial resection of the ureter makes it possible to improve long-term results in patients with hydronephrosis, including those with lesions of the UPJ and UVJ segments.In all cases, it was feasible to achieve a decrease in the degree of hydronephrosis.Postoperative complications were observed in five cases(4.6%),in none of which there were complications associated with the surgical technique, and were eliminated without loss of renal function.Conclusion: Our 22 years of experience shows that the technique of subadventitial resection of the ureter allows us to preserve the ureteral blood circulation during dismembered pyeloplasty and thus creates conditions for prevention of restenosis of UPJ and for single-stage ureteroplasty on the upper and lower ureteral segments.
1.Introduction
Among the causes of chronic kidney failure, obstructive nephro-uropathy is one of the leading congenital pathologies.Epidemiologically,obstructive uropathy accounts for 10% of the causes of acute renal failure and 4% of the causes of chronic end stage renal insufficiency [1].
Ureteropelvic junction (UPJ) obstruction is the most common cause of hydronephrosis and anomalies of the uretero-vesical junction such as obstruction and vesicoureteral reflux are the most common causes of the hydroureteronephrosis.It is not rare the coexistence of obstructions at the proximal and the distal ends of the ureter.McGrath et al.[2]followed up 225 patients with UPJ obstruction and identified 14(6.2%) cases of ureterovesical junction (UVJ) obstruction in this group.
Pitts and Muecke [3] reviewed 80 patients with megaureter and there were 20% of adult and 25% of children patients with UPJ and UVJ obstructions.In patients with high-grade vesico-ureteral reflux, UPJ obstruction was detected in up to 20% of cases [4].
Open or laparoscopic dismembered Anderson-Hynes pyeloplasty is an excellent procedure for treatment of UPJ obstruction and produces long-term improvement in function and drainage in most patients [5].Advantages of the dismembered pyeloplasty are widely applicable, including preservation of accessory vessels, possibility of pathologic UPJ excision,and appropriate repositioning[6].
We have proposed and applied a new method of dismembered pyeloplasty—subadventitial resection of UPJ to prevent vascular damage of the distal part of the pelvis and proximal part of the ureter.The preservation of blood supply in this area must improve regeneration of anastomosis and prevent fibrotic changes for long-term, simultaneously providing better condition for recovery of the kinetic ability of the ureter.
Surgical correction of hydroureteronephrosis with UPJ and UVJ obstructions together, is usually performed in two stages; pyeloureteroplasty is performed as the first stage;also sometimes ureterocystostomy is chosen as the initial stage of surgical treatment.Notably, simultaneous surgery is rarely used [7].If ureteral reimplantation is contemplated in future, for pyeloplasty, a V-shaped or Y-shaped Foley repair should be chosen, which has advantage of interfering with less ureteral blood supply [8].However, it is known that dismembered pyeloplasty by method of Anderson-Hynes is the gold standard for treatment of UPJ obstruction [5].
The method, subadventitial resection of the ureter,proposed and performed by us, allows to preserve ureteral branch of the pelvic artery during resection of UPJ and ureteral branch of the superior vesical artery during resection of UVJ, and reimplantation of the ureter.
The aim of this study was to improve the result of dismembered pyeloplasty with better preservation of blood circulation in the distal part of the pelvis and in the proximal part of the ureter during UPJ resection.At the same time,we set ourselves the task of determining the possibility of performing dismembered pyeloplasty and ureterocystostomy in one stage using subadventitial method of resection of the ureter.
2.Patients and methods
The study was conducted according to the principles of medical ethics.Informed consents of patients and their relatives were obtained for each operation, which were confirmed at the preoperative discussion in the medical council.The Ethics Committee of the Azerbaijan Medical University approved our scientific research (approved No.22) and compliance with ethical standards was confirmed.From March 1998 to March 2020, 110 consecutive open pyeloplasties were performed in 108 patients with application of the new surgical technique—subadventitial resection of the UPJ(bilateral in two cases:one stage in one case,two stages in the other case).Patients were observed from 12 months to 10 years (on average 36 months).
We briefly describe the technique of subadventitial resection of the ureter according to our proposed method.After dissection of the UPJ, the ureteral artery, located in medial side, was visualized (Fig.1), which is a continuation of the pelvic artery branched from the renal artery;parallel to it, an incision was made with a scalpel No.15 on the adventitial layer on both sides approximately 2 mm from the artery.Dissection of the adventitious layer of the ureter was completed using curved mosquito forceps.When the adventitial layer was dissected after two parallel incisions to the artery, approximately half of this layer remained above the ureter, and the other half remained together with the ureteral artery (Fig.2).
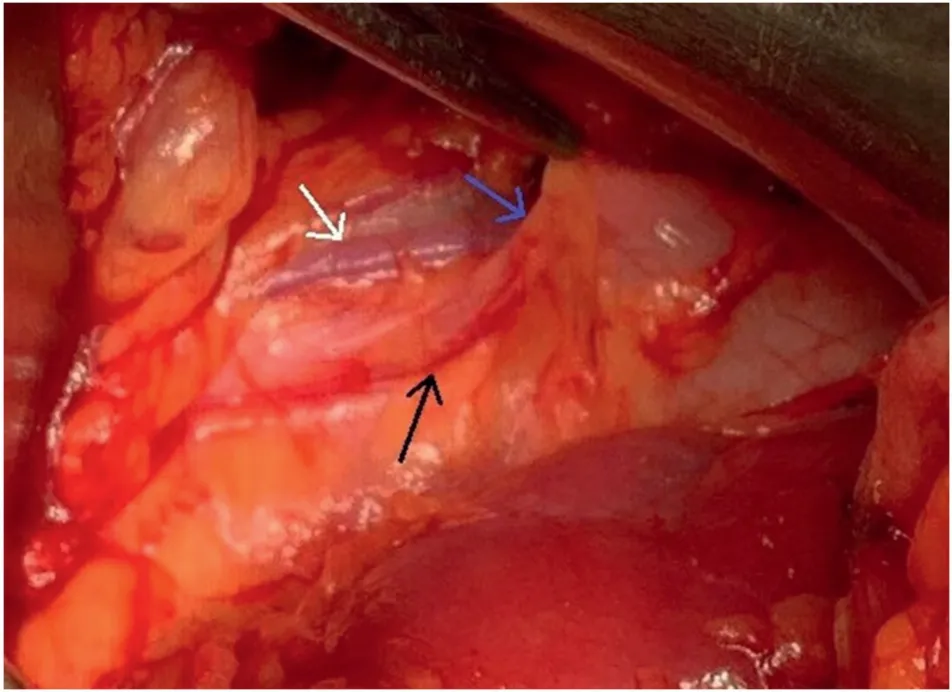
Figure 1 Ureteropelvic junction area in open dismembered ureteropyeloplasty.White arrow shows testicular vein; blue arrow shows ureter; black arrow shows ureteral artery.
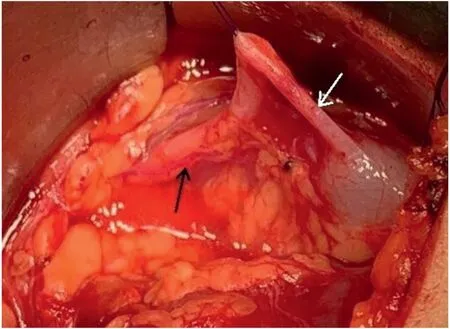
Figure 2 Incision and dissection adventitious layer of the ureter.White arrow shows ureter; black arrow shows ureteral artery.

Figure 4 Retrograde ureteropyelography.(A)Stenosis of the right ureteropelvic junction and Grade III hydronephrosis; (B)Stenosis of right ureterovesical junction and megaureter.
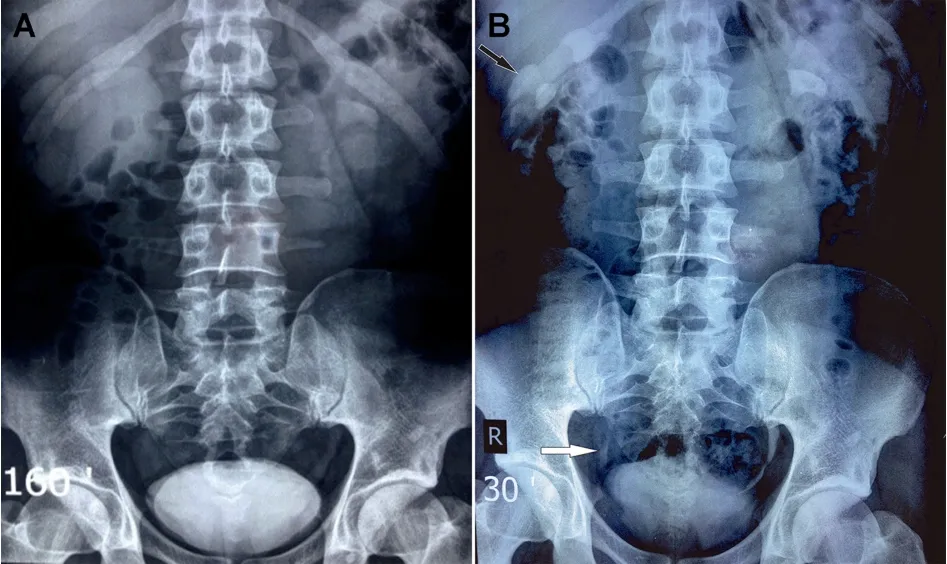
Figure 5 Preoperative and postoperative excretory urography.(A)Preoperative excretory urography.At 160 min on the left, the function was normal; on the right, only the contours of the kidney were determined.(B) Postoperative excretory urography (1 month after surgery).At 30 min, the functional ability of the right kidney improved;hydronephrosis decreased to Grade II(black arrow).The distal ureter was contrasted and the diameter was normal (white arrow).

Figure 6 Preoperative and postoperative excretory urography of a patient using ureteropyeloplasty with subadventitial resection of the ureter.(A) Preoperative excretory urography.At 120 min, left-sided Grade III hydronephrosis and right-sided pyelectasis (Grade I hydronephrosis) were detected.(B) Postoperative excretory urography (after 1 month of surgery).At 30 min, it was determined that the ureteropelvic junction had normal patency and a decrease in hydronephrosis to Grade II.
Dissection of the adventitial layer was performed approximately 3 cm above the ureter and 1.5 cm above the pelvis: In the presence of an accessory artery to the lower pole of kidney and the need for an antevasal anastomosis,the dissection length was increased by 1 cm to prevent compression of the ureteral artery from the accessory renal artery.After dissection of the adventitial layer of the ureter, together with the artery, a subadventitial resection of the ureter and pelvis was performed.On the medial side of the ureter,where the adventitial layer has been dissected,a 1.2—1.4 cm ureter incision was made.After placing the double-J ureteral stent, a running 6/0 suture was applied with synthetic absorbable monofilament suture material(Fig.3).
Preoperative renal function was studied using excretory urography in all patients.Diuretic renal scan was applied in cases on suspicion to nonobstructed pyelocaliectasis.In the postoperative period, follow-up was carried out on the basis of serum creatinine levels, urine analysis, and ultrasound examination.Excretory urography or computed tomography urography was used if restenosis was suspected.
On ultrasonography, we studied anteroposterior pelvic diameter and parenchymal thickness (mm) comparatively before surgery and 3 months after surgery.Complete success was defined as the absence of any clinical symptoms(pain scale: 0 for signs of no pain), combined with a significant reduction of hydronephrosis (reduction as a minimum one grade according to Society for Fetal Urology hydronephrosis grading system) based on ultrasonography or intravenous urography (IVU).
Multiple data analyses were performed, including patient age, grade of hydronephrosis, and presence of crossing vessels, operative time, and length of hospital stay.All statistical analyses were performed using the routines of the Statistical Package for Social Sciences,Version 12.0 for Windows (SPSS Inc, Chicago, IL, USA).
3.Results
There were 77 men and 31 women out of 108 patients.The median age of patients was 20.4 years(range:1—63 years).Left-sided hydronephrosis was diagnosed in 70 patients(14 patients with Grade II and 56 with Grade III),right-sided in 36 patients (nine patients with Grade II and 27 with Grade III), and bilateral Grade III hydronephrosis in two patients.
During surgery, fibromuscular stenosis of the UPJ was revealed in 58 patients;accessory vessels were the cause of hydronephrosis in 47 cases; and ureteral valves were found in three cases.When there were accessory vessels to the lower pole of the kidney, an antevasal anastomosis was performed, while the dissected adventitious layer of the ureter with the ureteral artery remained behind the accessory artery.
Congenital anomaly was revealed in five patients: a single kidney in one case; renal hypoplasia in two cases; a horseshoe kidney in two cases, complicated by Grade III hydronephrosis.In two cases, hydronephrosis were complicated by secondary nephrolithiasis, and pyeloplasty were combined by pyelolithotomy.In one case, Grade III nephroptosis was determined, in which additionally Rivoir nephropexy was performed simultaneously.
In a patient aged 22 years with stenosis of both segments complicated by Grade III hydronephrosis and severe renal impairment,we used subadventitial method of resection on UPJ with pyeloplasty by Anderson-Hynes, and UVJ by extravesical reimplantation of the ureter with antireflux mechanism (Figs.4 and 5A).One month after the surgery,IVU revealed decreased stage of hydronephrosis (from Grade III to Grade II) and improvement of the kidney function (Fig.5B).
In addition, a 1-year-old child with Grade III hydroureteronephrosis of the left kidney, who was diagnosed with UPJ obstruction and fourth grade vesicoureteral reflux, underwent subadventitial dismembered pyeloplasty and ureterocystostomy according to the Politano-Ledbetter method with the use of subadventitial resection of the intramural part of the ureter.One year after surgery,hydroureteronephrosis regressed(from Grade III to Grade I)and there was no left-sided vesicoureteral reflux.
The median operative time for pyeloplasty was 102 min(range: 78—130 min) and for UPJ and UVJ surgery was 230 min (range: 205—245 min).The median hospital stay after pyeloplasty was 3.7 days and after UPJ and UVJ correction 4.5 days.The overall success rates were 98.1%in UPJ group and 100% in two patients with ureteral repair of UPJ and UVJ segments.
As an indicator of preoperative total renal function,blood creatinine level was above normal only in one patient with bilateral Grade III hydronephrosis(2.76 mg/dL)and returned to normal after bilateral ureteral stent placement.Postoperative serum creatinine level was short-term slightly elevated (1.42 mg/dL) only in one case with urosepsis.
Postoperative follow-up revealed improved renal function and the disappearance of hydronephrosis(especially in children)or a decrease in hydronephrosis by at least in one grade (in adult patients) in all cases.In suspected cases,there is not any sign of obstruction on IVU (Fig.6) and/or diuretic renography.
Clinical manifestations as periodic pains in the lumbar region were observed in more than half of the patients(57 patients); in one patient (a 63-year-old woman), the examination was conducted for nephrogenic hypertension;hydronephrosis was found in two infants during prenatal examination; in other cases, ultrasound examination was not associated with this pathology.In the long-term postoperative period, resolution of clinical manifestations was achieved in all patients (including two re-operated patients).
Postoperative complications were observed in five patients (Table 1).On the basis of Clavien-Dindo classification, one case (bacteriuria) corresponds to Grade I, two cases (urine leak and urosepsis) Grade II, and two cases(restenosis and incorrect location of double-J stent)Grade III.
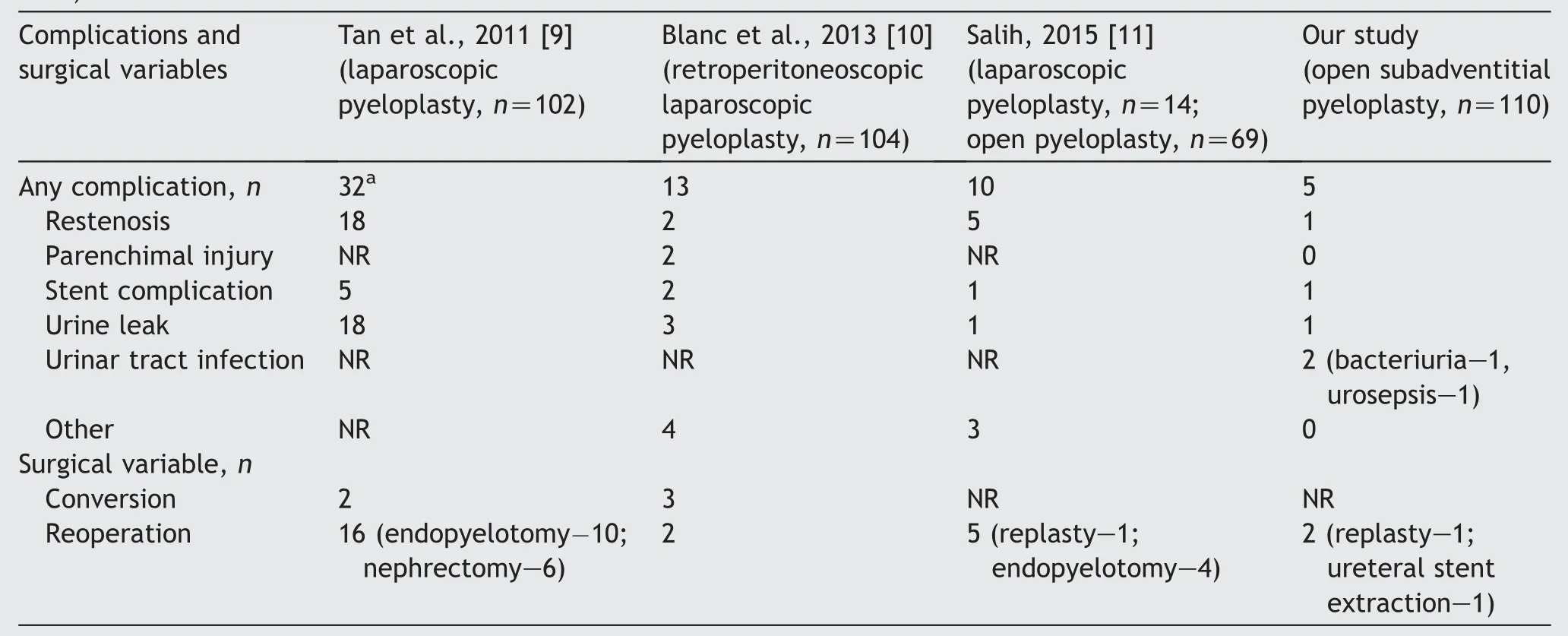
Table 1 Laparoscopic and open pyeloplasty complications and surgical variables (our results in comparison with literature data).
In case with restenosis (a 30-year-old man), the patient had a concomitant disease—type 2 diabetes mellitus.Subadventitial pyeloplasty was performed without double-J stent.In the postoperative period, urinary leakage was observed.After installation and removal of a double-J ureteral stent, UPJ restenosis was revealed.After 3 months, repyeloureteroplasty was performed with a satisfactory result—improved kidney function and regression of hydronephrosis from Grade III to Grade I.
In a 7-year-old patient in the postoperative period, an incorrect location of the ureteral stent in the ureter,established by the antegrade method, was revealed.The attempt of endoscopic removal of the stent was not successful due to the small diameter of the ureter and therefore, the stent was removed by open surgery and double-J ureteral stent was set in endoscopic way.After correction of the ureteral stent, the postoperative period was uneventful and hydronephrosis regressed from the Grade III to Grade II.
It should be noted that the two complications observed by us were not related to the procedure of plastic surgery and were caused by the absence or incorrect location of the ureteral stent.After reoperation, satisfactory functional and morphological results were achieved in all patients.
No complications were observed in the postoperative period in two patients who underwent simultaneous subadventitial dismembered pyeloplasty and ureterocystostomy with subadventitial resection of the ureter.
4.Discussion
Open dismembered pyeloplasty by Anderson-Hynes considered the gold standard of care for the treatment of UPJ stenosis with relatively high success rate[12].In the last quarter century, laparoscopic or retroperitoneoscopic dismembered pyeloplasty has been successfully introduced into clinical practice.The advantages of laparoscopic pyeloplasty over open surgery are the possibility magnified vision, low morbidity regarding the postoperative analgesia, shorter hospital stay,and minimal incision site scar.However,it is still a lengthier procedure with higher re-treatment rate (up to 17%)as compared to open dismembered pyeloplasty[9].
Our experience shows that a new technique for the preservation of ureteral blood circulation, the use of atraumatic surgical techniques, miniaturization of the incision, and the use of subcutaneous sutures can improve the postoperative period: reduce hospital days and the need for analgesics, and provide a cosmetic effect.
Despite the advancing of surgical technique with open and laparoscopic pyeloplasty, a relapse of the disease is observed in 6%—17% of cases, which is a consequence of restenosis in the anastomosis [9,11].With dismembered pyeloplasty, resection of the ureter inevitably is accompanied by a discontinuity of the ureteral artery.The main reason for the development of stenosis in the anastomotic area during dismembered pyeloureteroplasty can be considered insufficient blood circulation and the development of ischemia of the proximal ureter can be considered as the main reason for the development of stenosis in the anastomotic area during dismembered pyeloureteroplasty [8].
The method, subadventititial dismembered pyeloplasty that we have proposed, allows us to remove the fibromuscular-dysplastic-stenotic changed UPJ, preserve the integrity of ureteral artery located in subadventitial layer, and preserve ureteral blood circulation.An analysis of the results of subadventitial pyeloplasty in 108 patients(110 surgeries) proves the effectiveness of the proposed technique in the prevention of restenosis in the area of anastomosis.
In our practice, restenosis was observed only in one case, which was, in our opinion, a consequence of inadequate drainage of the kidney, when pyeloplasty without stent placement in the ureter was chosen.The second reoperation was carried out by us regarding the incorrect location of the double-J stent.The other two serious complications (urinoma and sepsis) occurred in a group of patients without the use of ureteral stents.In this aspect,our data correspond to the literature, which indicate the same complications in the group of patients without ureteral stenting [13].
Surgical correction of ureterohydronephrosis with UPJ and UVJ stenosis together creates certain difficulties in choosing a surgical tactic and usually performs in two stages: pyeloplasty should be performed 3 months before reimplantation of the ureter to vesical bladder.When reimplantation of the ureter is expected in the future,V-shaped or Y-shaped Foley repair should be chosen for pyeloplasty, which has the advantage of having less effect on the blood supply to the ureter.It is known that,dismembered pyeloplasty by method Anderson-Hynes is gold standard for treatment of UPJ stenosis, however, this method is unacceptable when ureterocystostomy is necessary in the second stage due to the interruption of the ureteral blood circulation supplied by the ureteral artery extending from the branches of the renal artery[7,8].
Subadventitial resection of the ureter allows us to preserve the ureteral branch of the pelvic artery for UPJ resection and ureteral branch of the superior vesical artery for UVJ resection,and ureteral reimplantation.Our clinical experience with successful results in two patients, with dismembered ureteroplasty in the ureteropelvic and vesicoureteral segments, creates the prerequisites for looking with hope at the problem of solving the issue of simultaneous surgical treatment of UPJ and UVJ stenosis.
5.Conclusion
Our experience in the treatment of patients with hydronephrosis who underwent open dismembered Anderson-Hynes pyeloplasty using our proposed new method of subadventitial resection of the ureter shows that maintaining the integrity of the ureteral artery and improving blood circulation in the anastomosis area can reduce complications during surgical treatment of this group patients,in particular, to provide prevention of restenosis.At the same time,our limited experience of one-stage surgical treatment of patients with UPJ and UVJ stenosis complicated by hydroureteronephrosis using the new method,subadventitial resection of the ureter,creates certain hopes for the use of simultaneous operations in the future in this pathology.
Conflicts of interest
The author declares no conflict of interest.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
- The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
- Antioxidant status in patients with bladder cancer regarding cancer stage and grade
