Robotic approach with neoadjuvant chemotherapy in adult Wilms’ tumor: A feasibility study report and a systematic review of the literature
Simon Sorz , Vlri Emm Plmiri ,Mri Rosri Rspollini , Ginomnio Rovillo ,Alrto Mntovni , Umrto Bsso , Mri Crmn Ainit ,Alrto D’Anlo , Lornzo Antonuzzo , Mro Crini ,Anr Minrvini , Lornzo Msiri ,
a Department of Oncologic, Minimally-Invasive Urology and Andrology, Careggi Hospital, University of Florence, Florence, Italy
b Department of Pediatric Urology, Meyer Children Hospital, University of Florence, Florence, Italy
c Clinical Oncologic Unit, Careggi Hospital, University of Florence, Florence, Italy
d Histopathology and Molecular Diagnostics, Careggi Hospital, University of Florence, Florence, Italy
e Medical Oncology Unit 1, Istituto Oncologico Veneto IOV IRCCS, Padua, Italy
f Hematology Oncology Division, Department of Women’s and Children’s Health, Padova University Hospital, Padua, Italy
g Department of Biology and Biochemistry, University of Bath, Bath, UK
KEYWORDS Nephroblastoma;Nephrectomy;Renal neoplasm;Minimally invasive surgery;Rare tumor;Wilms’ tumor
Abstract Objective: The incidence of Wilms’ tumor (WT) among adult individuals accounts for less than 1%of kidney cancer cases,with a prognosis usually less favorable when compared to younger individuals and an overall survival rate of 70% for the adult patients versus 90% for the pediatric cases.The diagnosis and treatment of WT are complex in the preoperative setting; neoadjuvant chemotherapy (NAC) or robotic surgery has rarely been described.This study aimed to review the literature of robotic surgery in WT and report the first adult WT management using both NAC and robotic strategy.Methods: We reported a case of WT managed in a multidisciplinary setting.Furthermore, according to Preferred Reporting Items for Systematic reviews and Meta-Analyses recommendations, a systematic review of the literature until August 2020 of WT treated with a robotic approach was carried out.Results: A 33-year-old female had a diagnosis of WT.She was scheduled to NAC,and according to the clinical and radiological response to a robotic radical nephrectomy with aortic lymph nodes dissection, she was managed with no intraoperative rupture, a favorable surgical outcome, and a follow-up of 25 months, which did not show any recurrence.The systematic review identified a total number of 230 cases of minimally invasive surgery reported in the literature for WT.Of these, approximately 15 patients were carried out using robotic surgery in adolescents while none in adults.Moreover, NAC has not been administered before minimally invasive surgery in adults up until now.Conclusion: WT is a rare condition in adults with only a few cases treated with either NAC or minimally invasive approach so far.The advantage of NAC followed by the robotic approach could lead to favorable outcomes in this complex scenario.Notwithstanding, additional cases of adult WT need to be identified and investigated to improve the oncological outcome.
1.Introduction
The incidences of Wilms’ tumor (WT) among pediatric patients range from 8 to 12 cases per million people and accounts for the most common solid malignancy, which is after neuroblastoma and brain tumor [1—3].In contrast,regarding the adult population, the estimated incidence of WT accounts for less than 0.2 cases per million people with a total impact on kidney cancer cases just less than 1%[4,5].Although the overall survival (OS) rate is approximately 90% [6,7] for pediatric patients, the prognosis is usually less favorable for adult patients with an OS of approximately 70% [4,8].
The OS discrepancy between pediatric and adult patients is the result of a faster diagnosis, a multidisciplinary approach, and on-time neoadjuvant chemotherapy (NAC)administered by WT-expert pediatric urologists, oncologists, and pathologists at referral pediatric hospitals [9].More recently,according to favorable oncological outcomes and the increasing knowledge of minimally invasive surgery(MIS), preliminary evidence of robotic and laparoscopic procedure strategies in young patients has been reported.Pediatric urologists have recently tried to correlate the well-established oncological results of the open approach with the benefit from reduced hospitalization, a better cosmetic surgery outcome, and minimized postoperative adhesions given by MIS [10,11].
Nevertheless,WT usually has a more aggressive behavior and features in adult patients with reduced OS that might be explained by a miscellaneous of factors such as the missing preoperative diagnosis without preoperative biopsy that not allow scheduling NAC, the inadequate staging due to low rate of lymph node sampling, and the unfamiliarity of an adult team with the diagnosis of WT.A combination of the aforementioned factors can potentially lead to a delay of appropriate risk-adapted therapy.Additionally, an ideal and shared management has not been validated so far [9].Given this background, some evidence supported a lack of experience in recording NAC or robotic approach(RA)in the adult setting[4,12].This study aimed to discuss the first WT management in an adult patient with the use of both NAC and RA, and review the RA approach in WT.
2.Patient (materials) and methods
2.1.Case report
After the obtainment of the institutional review board approval (IRB 567/19) in June 2019, all preoperative,oncological, and perioperative data of the case were prospectively collected.Written informed consent for the treatment and publication was obtained from the patient.
2.2.Systematic review
2.2.1.Search strategy
We performed a systematic review of the literature according to the updated Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) recommendations until August 2020[13].We defined a specific search strategy for WT treated with RA by combining free text and Mesh terms“Wilms OR nephroblastoma AND robotic OR robot-assisted OR robotic-assisted OR minimally invasive surgery”.We performed the retrieval using online databases, including MEDLINE,Cochrane Central Register of Controlled Trials,and Web of Science.
2.3.Inclusion criteria
Population, Intervention, Comparative, Outcomes, Study design(PICOS)criteria were used to assess the eligibility of articles for our systematic review:
· Population: patients enrolled with diagnosed of WT.We excluded patients with other histotypes from both the adult and the pediatric groups.
· Intervention: cases were scheduled to RA radical or partial nephrectomy.
· Comparative and non-comparative studies were included.Among the comparative studies (roboticvs.open; roboticvs.laparoscopic) only when a single patient underwent RA (with available data on WT) was enrolled.
· Outcomes considered were intraoperative results (i.e.,operative time and complication rate), postoperative,and follow-up features such as hospitalization, recurrence rate, and OS.
· Study design included retrospective studies,prospective studies, and case reports.
2.4.Systematic review process
We preliminarily identified 194 articles related to RA for WT.We excluded off-topic articles, reviews, book chapters, and editorials as well as those manuscripts with reports of noncompliance with PICOS criteria.Titles and abstracts were subsequently screened according to topic relevance(Fig.1).
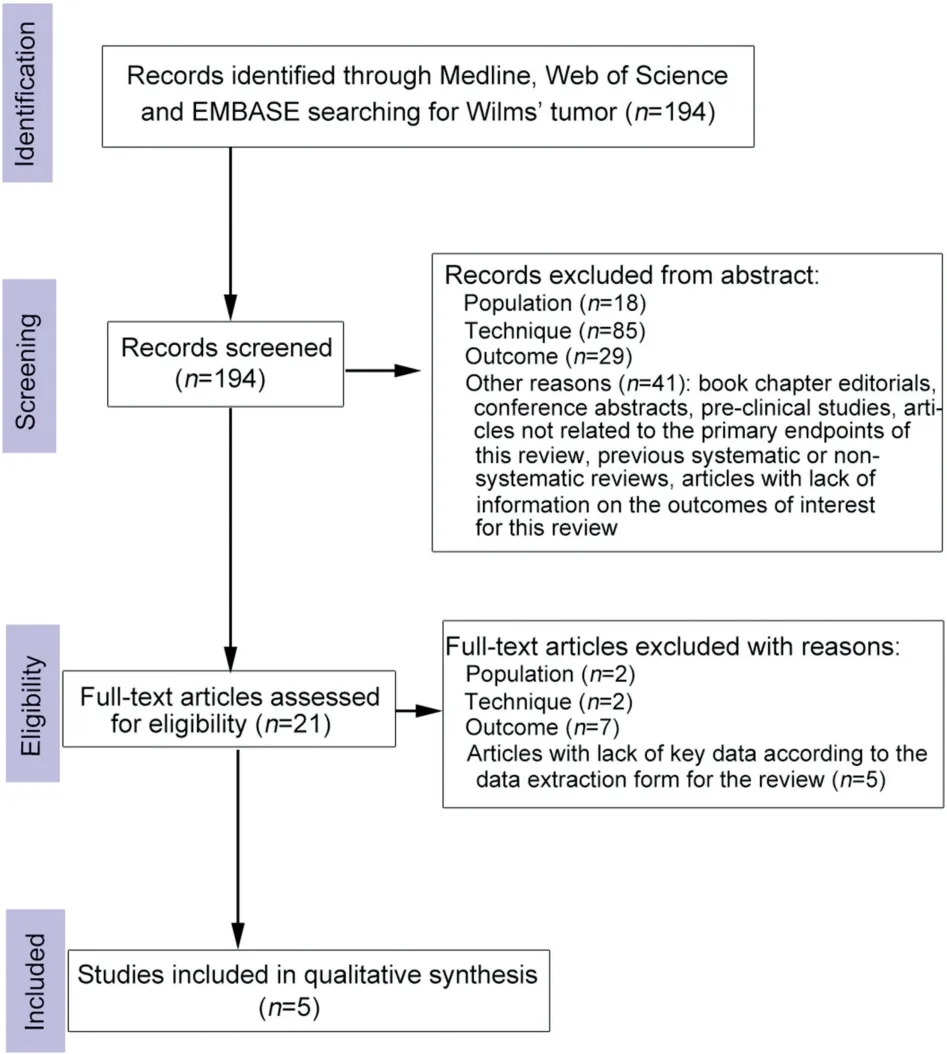
Figure 1 The updated Preferred Reporting Items for Systematic reviews and Meta-Analyses diagram for the systematic review.

Figure 2 Preoperative computed tomography scan showing a 13 cm × 11 cm × 14 cm low-density mass (arrow) with a subvert structure in the left kidney, without hydronephrosis.(A)Coronal scan; (B) Axial scan.
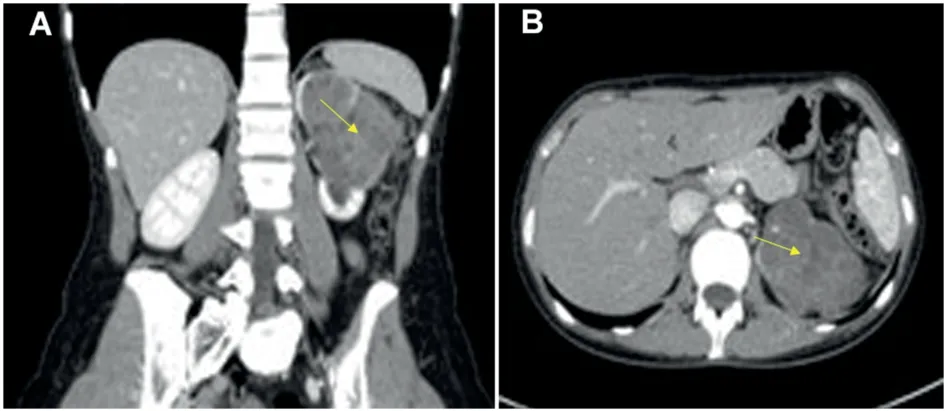
Figure 3 Computed tomography scan after neoadjuvant chemotherapy showing the radiological partial response to the therapy with a reduction of the renal mass (dimension of 8.5 cm × 60.0 cm × 8.0 cm, arrow) without the infiltration of other organs.(A) Coronal scan; (B) Axial scan.
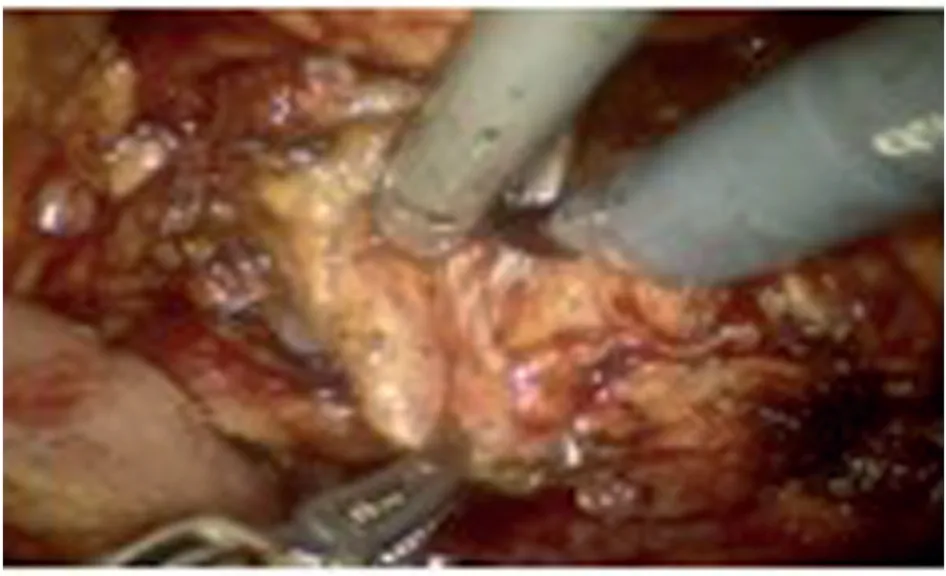
Figure 4 Intraoperative robotic lymphadenectomy.In the surgery, the lymph nodes presented aspects of fibrosis and adhesion to the major vessels.

Figure 5 Histopathological examination (20×).The picture showed nephroblastoma (Wilms’ tumor) which consisted of a mixture of three different tissue, including blastema (left),epithelium (right), and stroma (central).
2.5.Data extraction
Data were reported into a chart including significant information previously selected.The extracted features from each study included first author’s name, publication year,study design, number of patients, sex, age, NAC, type of surgery, operative time, estimated blood loss, length of hospital stay, complication, positive surgical margin,retrieval lymph node, follow-up period, local recurrence,and OS.
The overall quality of evidence was assessed according to the grading of recommendations, assessment, development, and evaluation.A narrative form was used for qualitative data synthesis.
3.Results
3.1.Case report
3.1.1.Clinical presentation and preoperative management with biopsy
We reported the case of a 33-year-old Caucasian female with no medical history.She self-admitted to the emergency department complaining of hematuria in April 2019.The patient reported that she has been suffering from occasional and slight flank pain for a year without any grinding urinary or local symptoms.Abdominal and thoracic computed tomography (CT) revealed a 13 cm × 11 cm × 14 cm lowdensity mass with a subverted structure in the left kidney,with no hydronephrosis.Some para-aortic and inter-cavaaortic lymph nodes, with the major axis below 9 mm, were identified, with no additional noteworthy lymph nodes or metastasis reported by CT (Fig.2).The radiologist from the emergency department originally supposed the lesion suspicious of kidney lymphoma, although the tentative diagnosis was considered questionable by the clinical team.
Due to the controversial clinical presentation, a percutaneous needle biopsy of the kidney was scheduled.After a few days, the genitourinary expert pathologist (Raspollini MR) hypothesized the lesion was suggestive of nephroblastoma: immunohistochemistry showed expression of WT protein 1 and cytokeratin AE1/AE3 marker whereas other neoplastic markers such as chromogranin, synaptophysin,myogenin, or common antigen (CD45) were negative.The specimen revealed absence of anaplasia.The mandatory second opinion required by the Italian Network of Rare Tumors confirmed the diagnosis of WT.
3.1.2.NAC
Following the multidisciplinary tumor board evaluation that involved high experienced urologists, oncologists, and pediatric oncologists from two referral centers, the patient was enrolled in the high-risk group of WT,mainly due to her age of 33 years, and scheduled for NAC accordingly.The patient was in good general condition with an Eastern Cooperative Oncology Group Performance Status of zero.At first, for the prevention of the cardiotoxic effect of anthracyclines, the patient underwent a cardiological evaluation before treatment onset, with baseline echocardiography that showed an ejection fraction of 57%.The neoadjuvant treatment, according to the SocitInternationale d’Oncologie Pdiatrique WT protocol, consisted of a 6-week regimen of three drugs: actinomycin D,vincristine, and doxorubicin.Vincristine was administered weekly (1.5 mg/m2intravenously [i.v.], maximum 2 mg),actinomycin D(45 μg/kg i.v.,maximum 2 mg)at Weeks 1,3,and 5, while doxorubicin (50 mg/m2i.v.) at Weeks 1 and 5.Neutropenia grade (G) 3 (neutrophil 720/μL) occurred at Week 3 and the treatment was therefore 1-week delayed.Additional adverse events were alopecia G2, anemia G1,and oral mucositis G1.
The CT restaging was scheduled for the middle of July(13 days after the end of chemotherapy) and showed a partial shrinkage (partial response) of the renal mass(8.5 cm × 6.0 cm × 8.0 cm) without infiltration of other organs.About 8—12 lesion-infiltrated lymph nodes were reduced in dimension(the higher major diameter of nodes:9 mmvs.5 mm), while previously identified lymph nodes were unchanged (Fig.3).
3.2.Surgical management
Given the positive radiological and clinical response to the NAC regimen,a robotic radical nephrectomy was scheduled for the end of July with aortic lymph nodes dissection.Due to the central and upper location of the mass, a nephronsparing approach was considered inappropriate.Surgery was performed by Masieri L, an adult and pediatric MIS expert urologist [14—16].
A transperitoneal approach was used in the flank position.Pneumoperitoneum was induced with the Hasson technique and the optical port (12 mm) was positioned periumbilically.Two 8-mm ports for robotic instruments were positioned at the external third part between the anterior superior iliac spine and the umbilicus and on the pararectal line 2 cm beyond the costal margin.A 5-mm port for the bedside assistant was positioned on the pararectal line, halfway from the optical port and the operative robotic arm while an AirSeal® system (12-mm port, CONMED, Russell House, UK) was placed halfway from the camera and the other robotic instrument (Da Vinci Si®,intuitive Surgical,Sunnyvale,CA,USA).The left colon was mobilized and a lymphadenectomy—including aortic and periaortic nodes from the inferior mesenteric artery over the renal artery—was carried out; the removed lymph nodes showed fibrosis and adhesion to the major vessels (Fig.4).Subsequently, the ureter was isolated and a clip was placed on its central part.The renal hilum was meticulously dissected to better delineate the vascular structures before their ligation with clips.The kidney was isolated with the adrenal gland-sparing technique and, thanks to the remarkable dexterity of the robotic platform, the risk of a potential kidney rupture was minimized.Moreover, a laparoscopic surgical specimen retrieval bag was inserted through the AirSeal® system and the entire kidney specimen, with associated lymph nodes, was placed into the bagen blocwhich was subsequently closed.Ultimately, a hemostasis control was performed and drainage was placed, followed by the specimen extraction through a Pfannenstiel incision(Fig.5).
The total operative time accounted for 180 min, with 140 min of console time.Intraoperative overall blood loss was 70 mL with no intraoperative complications.The length of hospital stay was 5 days with an uneventful postoperative period, although a lymphatic liquid output from the surgical drainage was documented for 2 days (150 mL and 140 mL,respectively).The patient reported no fever or other symptoms.
3.3.Final histological result and adjuvant chemotherapy
The final histological inspection confirmed the diagnosis of WT.The macroscopic examination reported a solid white-to-yellow unifocal lesion with brownish and ocher yellow areas involving the kidney with a dimension of 8.0 cm × 7.5 cm.The microscopic specimen investigation was suspicious of a potential change of malignancy induced by NAC due to the presence of fibrosis, hemosiderin, and xanthogranulomatous inflammation that involved 70%of the renal mass, whereas the remaining tissue consisted of epithelial (15%) and blastemal tissue (15%).There was no sign of anaplasia (Fig.5).Fortunately, the tumor was limited to the kidney with no sign of vessel, ureter, renal fat,or lymph node infiltration(0/24).No adult classification of WT is available and, according to the Children Oncological Group classification system, since a renal biopsy was performed in the preoperative setting, the malignancy stage for our patient was jointly agreed as Stage III.On the contrary, according to the SocitInternationale d’Oncologie Pdiatrique classification, the malignancy stage was classified as Stage I[17].An external review by a rare tumor-specialized pathologist (Angelo Paolo Dei Tos)confirmed the final histological diagnosis of WT.
Following a discussion between pediatric and adult oncologists, the patient was scheduled for adjuvant chemotherapy.As the neoplasm was assessed as high-risk malignancy due to the presence of blastemal component,the adjuvant systemic treatment was composed of weekly i.v.vincristine 1.5 mg/m2(maximum dose of 2 mg) for Weeks 1—8, then at Weeks 11, 12, 14, 15, 17, 18, 20, 21,23, 24, 26, and 27, combined with 3-weekly i.v.actinomycin D 45 μg/kg (maximum dose of 2 mg) from Week 2,and five doses of 6-weekly i.v.ADR 50 mg/m2from Week 2.Chemotherapy was scheduled to begin 25 days after surgery.Since the patient experienced neutropenia G3,granulocyte-colony stimulating factor was administered from Week 5 of treatment to avoid dose reduction.A cardiological evaluation was performed 6 months from the previous one with echocardiography that showed an ejection fraction of 55%.In December 2019, a CT scan showed no local or distance relapse.
Similarly, on a CT follow-up inspection in May 2020, 2 months after the end of chemotherapy and 10 months after surgery, the patient reported a good quality of life with no significant therapy-related adverse events, suggesting adequate treatment tolerability and no local or distance recurrence.At the last follow-up, 25 months after surgery,no local or distant recurrence was reported.
3.4.Systematic literature review
Despite several surgical procedures being available for the treatment of WT in children, limited data are currently available for adult WT treatment using MIS and open strategy.As a result,five studies that met all PICOS criteria were included (Table 1).Overall, a total number of 12 patients were included in five studies regarding RA.The key characteristics of each paper included in this review are reported in Table 1.Four studies were case reports, one paper reported data from eight patients [11,18—21].Regarding the gender,three patients are female, one male and it was not reported in the study of eight patients.

Table 1 Overall features of studies of Wilms’ tumor treated with robotic approach included in this systematic review.
Regarding the WT treated with RA, the ages reported ranged from 1.5 years old to 14.0 years old and the NAC was administered in eleven cases (11/12).The types of surgery were nine radical nephrectomies and four partial nephrectomies, respectively (one patient underwent a bilateral procedure) [21].The operative time ranged from 120 to 360 min with two conversions to the open approach(2/12).Regarding the complications, no significant blood loss occurred in the whole series analyzed.It suggested that no major complications occurred in these studies, and robotic surgeries are considered to be safety for WTs.The only complication reported is a persistent output from drain(28 days).The length of hospital stays ranged from 2 to 7 days.The only patient with a prolonged permanence in the hospital was connected to the persistent output drain, as before mentioned, with 28 days of inpatient department period.
Furthermore, concerning the oncological outcome, no positive surgical margins were assessed in all series.These data might suggest that a careful selection of the patient might produce a favorable histological exam.The lymph nodes retrieval number are not recorded in two studies[18,19];moreover,lymph nodes dissection is not practiced in other two studies[20,21],with only one series reported a median of 6(range 2—10)removed lymph nodes[11].No local recurrence was assessed in three studies [11,19,21]and was not recorded in the other two experiences[18,20].The OS rate is high with only one patient (1/12)dying of WT (Table 1).
4.Discussion
The WT incidences among pediatric patients ranged from 8 to 12 cases per million people and is the most common solid malignancy,after neuroblastoma and brain cancer,with an OS of approximately 90%[6,7].Generally,the open surgical approach helps minimizing the risk of rupture and over-staging [1,2,22].In recent years, however, MIS has become popular for the adult and pediatric patients for reconstructive purpose and oncological surgery [23—25].With the increase of the knowledge and according to encouraging outcomes reported in pediatric and adult urology, MIS has been used for WT treatment, with approximately 230 cases documented[10,11,26—29].Given this background, and despite several surgical procedures available for the treatment of WT in children, limited data are currently available for adult WT treatment using MIS and open approach [4,12,30—32].
NAC is rarely administered to adult WT patients since the diagnosis is normally achieved incidentally after radical nephrectomy; indeed, renal cell carcinoma accounts for the majority of the adult kidney cancer cases and is usually resistant to chemotherapy.Therefore, a preoperative biopsy might be irrelevant for the clinical course and early surgical treatment is the preferred option.Furthermore,the role of renal biopsy, although specific and sensible for cancer detection, is still considered controversial mostly due to the inability to properly evaluate peri-renal fat,vascular invasion, tumor grading, and distinguish oncocytic type neoplasms[33,34].In short,WT diagnosis is commonly achieved in the nephrectomy specimen.
In this scenario, the clinical team, composed of urologists and oncologists, has no standard treatments or age-specific protocols validated for adult WT.Indeed,most cases were treated with stage-adjusted chemotherapy with or without local radiotherapy, and tailored according to pediatric chemotherapy regimens [4,12,35—37].
In the current paper, we described a multidisciplinary management of adult WT patient that involved two hospitals with expert urologists, oncologists, pediatric oncologists, and pathologists who, to the best of our knowledge,carried out the first NAC followed by robotic radical nephrectomy and lymphadenectomy.
The initial suspect of lymphoma was questioned and,given the unusual clinical presentation, we opted for a renal biopsy that showed a mixture of blastema, epithelium, and stromal tissue.The epithelial component consisted of small tubules lined with primitive columnar cells and abortive glomeruli.The diagnosis of WT was supported by the positive staining for WT protein 1 and different cytokeratins, within the epithelial component, and the negative staining for chromogranin, synaptophysin, myogenin, or CD45.
Although there are no histological differences between pediatric and adult WTs, the diagnosis of adult WT is somewhat complex and challenging for pathologists.In our case, to avoid unnecessary treatment and toxicity, according to the Italian Network of Rare Tumors, a second opinion from an external highly specialized pathologist confirmed the WT diagnosis [38,39].
After a multidisciplinary meeting, to replicate and maximize the effect of the pediatric experience, the NAC regimen was scheduled [7].So far, only eight adult WT cases described in the literature were administered with chemotherapy in a preoperative setting after biopsy[4,12].
The CT inspection scheduled after NAC showed a good response.Since the advent of robotic surgery has offered a more reliable minimally-invasive alternative than open surgery, we adopted a robotic radical nephrectomy approach plus lymphadenectomy.RA provides magnified tridimensional imaging motion scaling, tremor reduction,and higher maneuverability as well as dexterity,leading to substantial advantages in the reconstructive and oncological field [40—42].In contrast, regarding other MIS approaches, laparoscopy has intrinsic limitations such as two-dimensional imaging, surgeon discomfort, steep learning curve, and limited range of surgical instruments motion [43].
As shown in this study, the advantages of RA have been observed not only in the nephrectomy accuracy and the cosmetic results that are mainly subject to a laparoscopic surgeon’s skills, but also mainly in the lymph nodes dissection.Regardless of the adult patient’s age—if compared to other studies[10,44,45]—a safe and extensive lymphadenectomy was carried out, with 24 lymph nodes removed in total.Indeed, appropriate and accurate lymph node sampling is one of the milestones for WT staging[46,47].
In terms of RA advantages for WT treatment, the first report regarding a 14-year-old female who underwent robotic-assisted radical nephrectomy was documented by Cost et al.[18] The authors discussed the importance of patient eligibility for MIS when cancer was confined to endophytic nature, thus decreasing the risk of rupture.Moreover,they emphasized that robotic strategy employs a transperitoneal approach, including a full exploration of the peritoneal cavity and an optimal regional lymphadenectomy, with good cosmetic outcomes.They finally advised on the accurate selection of patients to preserve surgical oncology standards with the benefit from MIS[18,19,48].
Furthermore, partial robotic nephrectomy for WT treatment in a WAGR(WT,aniridia,genitourinary problems,and mental retardation) syndrome was described in 2016,with favorable surgical and oncological outcome in a 2-year-old pediatric patient who underwent NAC followed by surgery [20].Although preliminary reports of open partial nephrectomies have been reported, this surgical strategy should be recommended only for carefully selected patients with bilateral WT,solitary kidney,or those diagnosed withfavorabletumorlocationanddimension[11,17,49—52].
Noticeably, only one case in literature has been described for the contemporary robotic treatment of bilateral WT.Sala et al.[21] discussed the feasibility of a simultaneous RA approach for partial nephrectomy with contralateral radical nephrectomy after NAC in a 3-year-old WT patient.No significant intraoperative or postoperative complications occurred, with an operative time of 90 min and hospitalization period of 2 days.
Recently, a large monocentric study has been reported that investigated young cancer patients treated with RA[11].They collected six nephrectomies and two partial nephrectomies of WT although two surgery conversions to open surgery have been reported.Overall,complete tumor removal with no kidney rupture was achieved for all cases.The postoperative course was uneventful, with neither recurrence nor medium-term complications occurred.Only a child had a fatal event following brain metastases 1 year after surgery.OS of WT patients was 87.5% at the median follow-up of 14.8 months (range: 4—25 months).The authors speculated that RA (radical or partial nephrectomy)for renal tumor in young individuals may be an option for carefully selected cases;eligibility should be discussed with a multidisciplinary approach and surgery strictly performed in full compliance with oncological surgery standards [11].
Concurrently, Bouty et al.[26] evaluated the feasibility and outcome of a large multicenter study of MIS in 50 young individuals diagnosed with WT.Regrettably, only four patients underwent RA.It is worth mentioning that one of the centers was already involved in the previous multicentric study by Blanc et al.[11].Although the precise number of patients recruited in both studies(same enrollment period)was not specified, Bouty et al.[26] reported that MIS was carried out in 19% of the 195 WT nephrectomies, with only six surgeries converted to open approach and low positivity of tumor margins(three cases).After a median follow-up of 34 months (range: 2—138 months), two local recurrences(both Stage I, intermediate-risk, at 7 and 9 months after surgery) and one metastatic relapse (Stage III, high-risk, at 4 months after surgery) were documented with the 3-year event-free survival of 94%.They hypothesized that MIS is actionable for selected patients with similar oncological outcomes to those who undergo open surgery, although follow-up surveillance is needed to evaluate the progress of this technique [26].
So far,fewer than 15 WT cases have been reported with RA in literature with only few adolescents and none for adult patients.Moreover, NAC has not been administered(before MIS) in adult WT patients up until now.
One of our take-home messages is the relevance of scheduling a renal biopsy for adult patients when the diagnosis is complex.Secondly, multidisciplinary team is pivotal, which should involve experts from different fields,hospitals, and areas.Nowadays, good networking between different centers is possible and can lead to favorable patient outcomes; complex patient management by a single clinician should be avoided.The third key message is the role of RA in difficult oncological cases such as WT.This surgical procedure could outperform the open approach in the presence of low surgical margins and large lymphadenectomy, and could also avoid the risk of rupture when carried out by highly skilled professionals.In addition, RA might reduce hospitalization time and lead to excellent cosmetic outcomes, minimizing postoperative adhesions risk.The fourth take-home message of our case, corroborated by a review of the literature,is the importance of the accurate selection of patients eligible for RA,in compliance with oncological surgery standards.Lastly,we advise on the importance of this specific procedure to be carried out at referral centers.
We must report a lack of data and evidence in the literature.Additional cases of adult WT need to be investigated, including those from multi-centers.This would allow for the collection of data such as imaging, biomarkers, immuno-histochemical features, resulting in the development of more efficient, reliable methods, and guidelines for the distinction of WT from other kidney cancers, thus zeroing therapy delay and improving the oncological outcome.
5.Conclusion
WT is a rare condition in adult, although it is possible.In such cases, a multidisciplinary approach should be mandatory and the use of NAC followed by RA might result in a favorable outcome.However,further cases of adult WT need to be recorded, including those from highly specialized centers, with the overarching goal of improving the clinical outcome.
Author contributions
Study concept and design: Simone Sforza, Lorenzo Masieri,Lorenzo Antonuzzo.
Data acquisition:Alberto Mantovani,Maria Carmen Affinita.
Data analysis: Simone Sforza, Valeria Emma Palmieri.
Drafting of manuscript: Simone Sforza, Valeria Emma Palmieri, Maria Rosaria Raspollini, Giandomenico Roviello.
Critical revision of the manuscript: Lorenzo Masieri,Umberto Basso, Marco Carini, Alberto D’Angelo, Andrea Minervini.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledge
The authors thank Doctor Angelo Paolo Dei Tos from Department of Pathology, Azienda Ospedale Universita`Padova, Padua, Italy for the final review of the histological result.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
- The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
