Daily activities and training experiences of urology residents during the coronavirus disease 2019 pandemic in Indonesia: A nationwide survey
Pono Birowo , Nur Rsyi Chiir A.Mohtr Bmng S.Nogroho , H.R.Dnrto , Bsut Drynto ,Lukmn Hkim , Dynr Priksit , Fkhri Rhmn S.Chyo Ariwiksono
a Department of Urology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital,Jakarta, Indonesia
b Department of Urology, Faculty of Medicine, Padjadjaran University, Hasan Sadikin Hospital,Bandung, Indonesia
c Department of Urology,Faculty of Medicine,Gadjah Mada University,Sardjito Hospital,Yogyakarta,Indonesia
d Department of Urology, Faculty of Medicine, Universitas Brawijaya, Saiful Anwar Hospital, Malang,Indonesia
e Department of Urology, Faculty of Medicine, Airlangga University, Soetomo Hospital, Surabaya,Indonesia
f Department of Urology, Faculty of Medicine, Universitas Indonesia, Universitas Indonesia Hospital,Depok, Indonesia
KEYWORDS Activity;Coronavirus disease 2019;Learning method;Training;Urology resident
Abstract Objective: To explore the impact of the coronavirus disease 2019 (COVID-19)pandemic on the training experiences of urology residents in Indonesia.Methods: A cross-sectional study using a web-based questionnaire(SurveyMonkey)involved all registered urology residents in Indonesia.The questionnaire was structured in Bahasa Indonesia,composed of 28 questions,and divided into three sections:demographic characteristics,current daily activities,and opinions regarding training experiences during the COVID-19 outbreak.The survey was distributed to all respondents via chief of residents in each urology center from May 26, 2020 to Jun 2, 2020.Results: Of the total 247 registered urology residents, 243 were eligible for the study.The response and completeness rate for this study were 243/243(100%).The median age of respondents was 30 (range: 24—38) years old, and 92.2% of them were male.Among them, 6 (2.5%)respondents were confirmed as COVID-19 positive.A decrease in residents’involvement in clinical and surgical activities was distinguishable in endourological and open procedures.Most educational activities were switched to web-based video conferences, while others opted for the in-person method.Smart learning methods, such as joining a national or international speaker webinar or watching a recorded video, were used by 93.8% and 80.7% of the respondents, respectively.The respondents thought that educational activities using web-based video conferences and smart learning methods were effective methods of learning.Overall,the respondents felt unsure whether training experiences during the COVID-19 pandemic were comparable to the respective period before.Conclusion: The COVID-19 pandemic negatively affected urology residents’ training experiences.However, it also opened up new possibilities for incorporating new learning methodologies in the future.
1.Introduction
Coronavirus disease 2019(COVID-19)has affected various aspects of daily life,particularly socioeconomic and health car e practices[1,2].The disease,caused by severe acute respiratory syndrome coronavirus 2, has infected more than five million people and resulted in more than 300 000 deaths worldwide.In Indonesia, the first case of COVID-19 was reported on March 2nd, 2020, and its number has rapidly increased since then.This forced the Indonesian government to apply the first large-scale social restriction that started on April 10th,2020 for almost 2 months.Therefore,it is considered the most significant challenge for health care services today [3].Also, the exact time when the current pandemic situation will end remains obscure to this day.
The pandemic has also impacted health care services in the urological field.Pattern changes in daily clinical practices,reduction of patient visits to the outpatient clinic and surgical services, and careful selection of surgical patients were seen as a part of urological service adaptation during the COVID-19 pandemic [4,5].Current literature shows a significant decrease in urology residents’ clinical and surgical activities and a higher stress level during the COVID-19 pandemic in Italy and France[6,7].Moreover,in Indonesia,where urology residents mainly gain surgical experiences from affiliated teaching hospital rotations,only one urology center continued rotation for residents at such hospitals[5].To overcome this limitation, various mechanisms concerning smart learning technology were rapidly adopted,such as recorded video,webinar,virtual round,and surgery simulation [8,9].
In general, it can be assumed that the pandemic negatively impacted urology residents’ quality of training.However, whether all urology residents at different levels negatively reflected their training experiences during the COVID-19 pandemic is still unknown.Besides, a previous study in Indonesia, which tried to evaluate the impact of COVID-19 on urology practice, did not specifically explore urology resident training[5].Therefore,this study aimed to explore urology residents’ daily activities and training experiences during the COVID-19 pandemic.
2.Methods
2.1.Study design and population
This study was an observational, cross-sectional study conducted using a web-based survey and involved all registered urology residents across Indonesia.Residents on leave were excluded from this study.
2.2.Questionnaire development
The questionnaire was constructed using Bahasa Indonesia(Indonesian language)in a cloud-based online survey called SurveyMonkey (www.surveymonkey.com).The survey comprised 28 questions and was divided into three sections to explore the demographic characteristics of the respondents, their current daily activities, and opinions regarding their training experiences during the COVID-19 period.The whole items in the questionnaire in both Bahasa Indonesia and English were presented in the Supplementary file.Residents concluded in this study have given their consents beforehand.This study was carried out after ethical approval obtained from the Health Research Ethics Committee of Universitas Indonesia (No.KET-682/UN2.F1/ETIK/PPM.00.02/2020).
2.3.Data collection
Survey distribution and data collection were completed within 1 week(May 26,2020 to Jun 2,2020)in collaboration with the chief of residents in every urology center.The survey was filled in anonymously and, therefore, a single response option was activated in the questionnaire to prevent data duplication from the same respondent.The response rate was checked by matching the total number of residents and their semesters of study across each urology center database.
2.4.Data analysis and presentation
SPSS version 23 (IBM Corp, Armonk, NY, USA) was used for data analysis, and only the completed questionnaire was further analyzed.Data interpretation from three segments of the questionnaire was presented as five different subsections in the result section, which were respondents’ demographic characteristics (subsection 1),COVID-19-related training and duties (subsection 2),residents’ involvement and opinions concerning educational activities(subsection 3),residents’involvement and opinions on clinical and surgical activities (subsection 4),and residents’ opinions related to research activities and overall experiences during COVID-19 pandemic and future direction (subsection 5).Tables and graphs were used in the study for convenient data interpretation.Scale question within the residents’ opinion section was treated as numerical data and presented as mean without 95% confidence interval if it had a skewed data distribution to give more information to the readers.The residents’ opinions regarding self-assessment of COVID-19 knowledge were compared between those who received training and those who did not.The residents’ opinions regarding the effectiveness of educational activities were presented as overall respondents and urology rotation only respondents(i.e., urology rotation and board exam candidates).Moreover, the analyses of the residents’ opinions in subsections 4 and 5 were compared based on their current rotation and competency level.Lastly, the analyses of opinions in subsections 3—5 excluded candidates who did not participate in the activity or did not use smart learning methods.A non-parametric test (Mann-Whitney test for two independent variables or Kruskal-Wallis test for more than two independent variables) was used to analyze the residents’opinions if it had a skewed data distribution and thep-value of less than 0.05 was considered as statistically significant.This study assigned three cut-off values of<2.75, 2.75—4.25, and >4.25 to classify the means of respondents’ responses to the opinion-related questions.A cut-off value of <2.75 was considered as non-functional for the learning method effectivity question.Thus, this item was not suggested as the learning method recommendation question or contradictive to the statement for the statement question.On the other hand,a cut-off value of >4.25 was considered adequate for the learning method effectivity question and was recommended for the learning method recommendation question or was found to be in line with the statement question.Lastly,a cut-off value of 2.75—4.25 was considered uncertainty depicted by the respondents regarding their opinions.These cut-off values were determined based on the authors’ agreement before the start of the study.
3.Results
3.1.Respondents’ demographic characteristics
Of 247 registered urology residents, four were on leave;hence,243 urology residents with a median age of 30 years(interquartile range: 24—38 years) were eligible for this study.About 92.2% of the respondents were male and currently worked in a teaching hospital.About 21.8% respondents were suspected of having COVID-19 but confirmed to be negative,and 6(2.5%)of respondents were confirmed as positive cases.The completeness and response rate in this study was 100%.Respondents’ demographic characteristics and characteristics of current rotation and level of competency with its correlation with the year of study can be seen in Tables 1 and 2,respectively.

Table 1 Respondents’ demographic characteristics.

Table 2 The relation between residency year with their current rotation and competency level (n=243).
3.2.COVID-19-related training and duties
COVID-19 training was given to 120/243 (49.4%) urology residents.A majority of the training (91.4%) given to the urology residents was organized by the hospitals that employed them.Webinar or online source, not organized by their hospitals, became the other source of training,accounting for 8.2% of the respondents, and one respondent did not specify his source of training.The questionnaires presented the respondents with questions on their thoughts on COVID-19-related training and duty,where the respondents would choose between a scale ranging from 1 to 6 where option 1 referred to strongly disagree and option 6 referred to strongly agree.Overall,the residents felt uncertain whether they had enough knowledge about COVID-19 patient management (mean score: 3.79).Even though trained respondents had a statistically higher mean score than residents who did not receive COVID-19-related training (3.97vs.3.64,p=0.007), both groups expressed that they were unsure in this regard.
Regarding COVID-19-related duties outside the spectrum of the urology residents’ usual tasks, 95/243 (39.1%) residents were offered roles such as swab test officer,COVID-19 triage or screening officer in the emergency room and at the hospital entrance, and COVID-19 volunteer doctor.However, only 29/243 (11.9%) agreed to these duties,including the service as a triage or screening officer in the emergency room (51.7%), duty doctor in COVID-19 emergency room or ward(41.4%),and COVID-19 volunteer doctor(6.9%).Moreover, 122/243 (50.2%) urology residents were unwilling to become COVID-19 volunteers.
3.3.Residents’ involvement and opinions on educational activities during COVID-19 pandemic
Resident educational activities during the COVID-19 pandemic can be seen in Fig.1A and B.A web-based video conference was the most used method for educational activities during the pandemic, even though direct meeting was still used occasionally.Webinars from national or international speakers were used as a smart learning method by 93.8% of the respondents.
The residents’recommendations for future usage of smart learning methods and their opinions on the effectiveness of the learning method can be seen in Fig.1C and D,respectively.All types of smart learning methods such as webinar from national or international speaker, recorded webinar or video learning,and podcast were recommended.Our survey reported that webinar from national or international speaker was their favored method of smart learning(mean score: 4.91), followed by recorded webinar or video learning(mean score:4.83)(Fig.1C).

Figure 1 Residents’ activities and opinions on educational activities during the COVID-19 pandemic.(A) The methods used in education activities; (B) Smart learning methods used; (C) Residents’ opinions on the future use of smart learning methods; (D)Residents’ opinions on the effectiveness of the current educational methods used during the COVID-19 pandemic.COVID-19,coronavirus disease 2019.WVC, web-based video conference; CI, confidence interval.# Excluded pre-hospital rotation respondents;∧Excluded respondents of whom this activity was cancelled;* Only included respondents using this smart learning method.& Rating scale: 1 represents strongly disagree; 6 represents strongly agree.

Figure 2 Residents’ activities and opinions on clinical and surgical activities during the COVID-19 pandemic.(A) Residents’working from home opportunities;(B)Residents’involvement in clinical and surgical activities(n=243);(C)Reduction in residents’involvement in clinical and surgical activities; (D) Methods used in patient rounds (respondents could choose >1 method if applicated).COVID-19, coronavirus disease 2019; WFH, working from home.
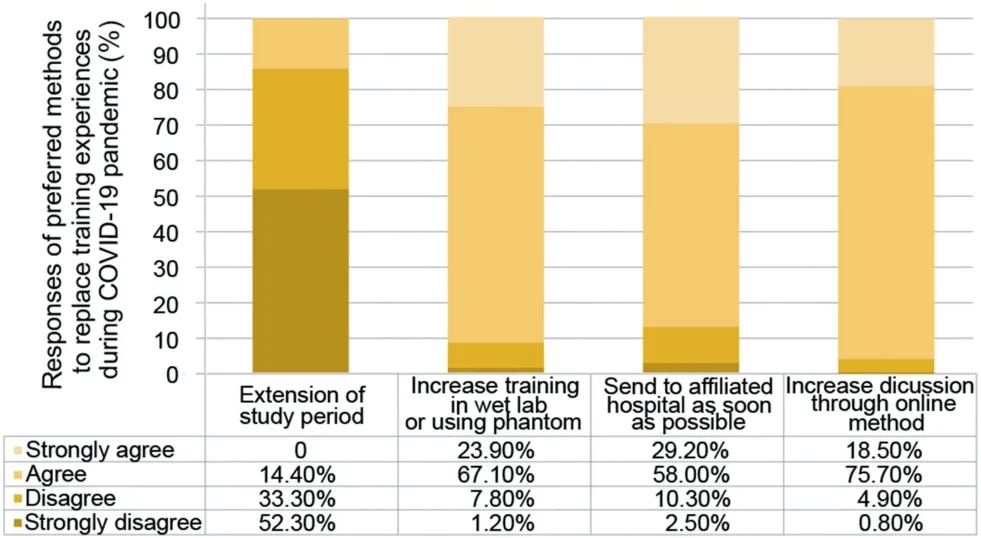
Figure 3 Residents’ suggestions of preferred methods to overcome lack of experiences during COVID-19 pandemic.COVID-19, coronavirus disease 2019.
The residents’ opinions on the statement given regarding educational activities during COVID-19 can be seen in Table 3.The highest respondent satisfaction in educational activities during the COVID-19 pandemic was seen in theory learning.
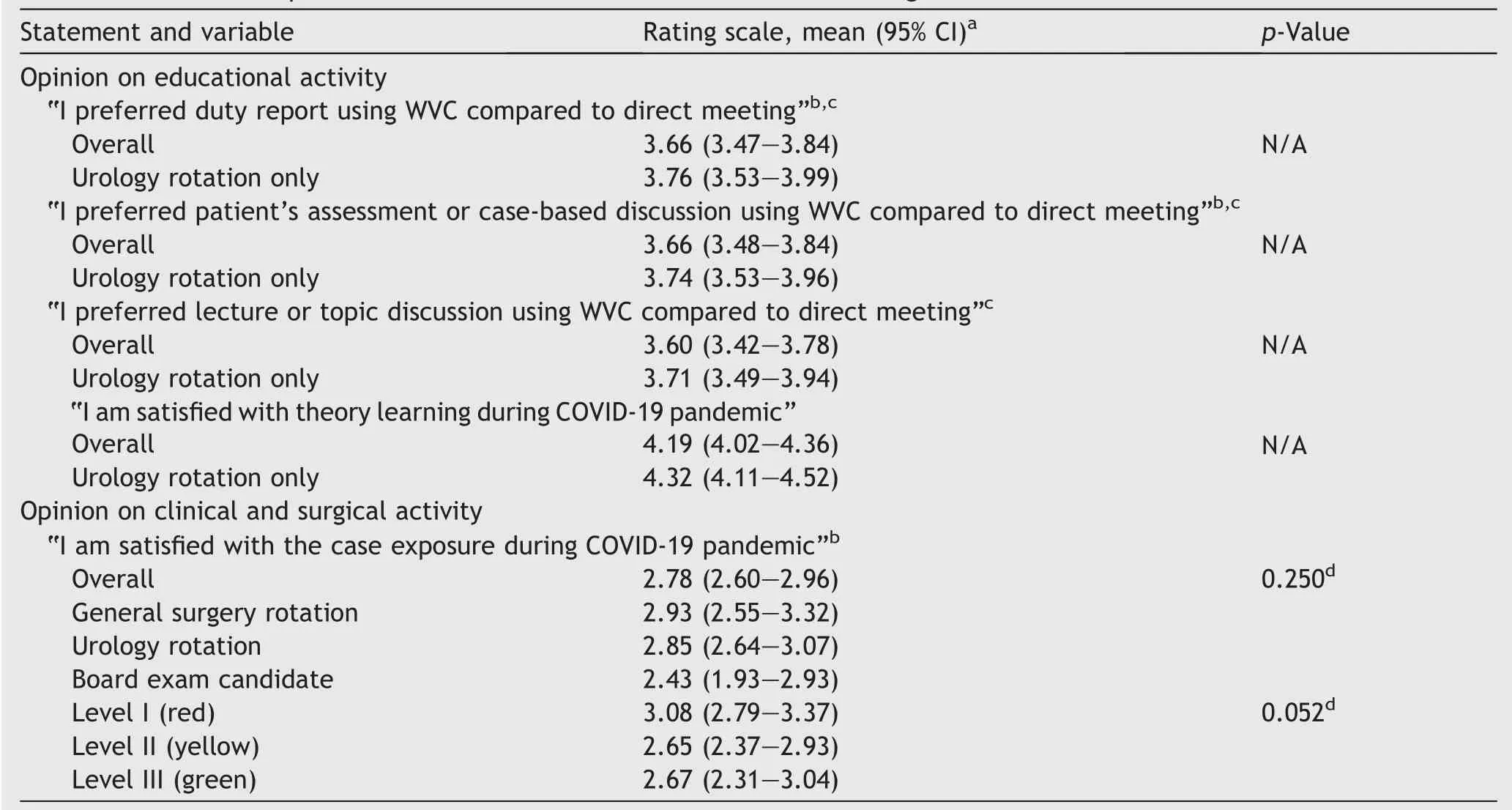
Table 3 Residents’ opinions on educational activities and clinical and surgical activities.
3.4.Residents’involvement and opinions regarding clinical and surgical activities during the COVID-19 pandemic
The residents’involvement in clinical and surgical activities and their opinions could be seen in Fig.2 and Table 3.During this pandemic, 86/243 (35.4%) respondents had worked with COVID-19 suspected or confirmed cases, of whom the attending physician accompanied only 20.9%.Moreover, 70/243 (28.8%) respondents accompanied the attending physician to visit other hospitals’patients outside their teaching hospital.
3.5.Residents’ opinions on research activities and overall experiences during COVID-19 pandemic and future direction
The residents’ opinions on research productivity and overall satisfaction concerning training experiences during the COVID-19 pandemic could be seen in Table 4.Overall,the respondents felt uncertain whether the workload and mental burden were heavier during the COVID-19 pandemic than before.Research activity was more productive during the COVID-19 pandemic for pre-hospital rotation respondents.

Table 4 Residents’ opinions on research and overall activities.
The residents’ suggestions for future training methods could be seen in Fig.3.Most respondents had agreed to increase discussion through online method (75.7%) and training in the wet lab or using phantom (67.1%).Other preferred methods used to replace training experiences during the COVID-19 pandemic, which mentioned by the respondents, were creating a web-based learning module,increasing the production of surgical videos, and performing live surgeries through online streaming.Lastly, most respondents (87.2%) were willing to go to an affiliated hospital even amid the current status of COVID-19.
4.Discussion
COVID-19 pandemic has become the greatest challenge to health care service and an obstacle for residency training.This study evaluated urology residents’training experiences using a web-based questionnaire and retrieved a 100%response rate and completeness rate.Therefore, it can provide a clear picture regarding urology residents’ training experiences during the COVID-19 pandemic in Indonesia.Residency training during the COVID-19 pandemic was endangered due to the limited building capacity and, more importantly,the residents’health and well-being.However,this study showed that 26.3% and 2.5% of urology residents had been appointed as COVID-19 suspected cases and through a swab PCR as positive cases, respectively.
Moreover, only 49.4% of the residents had received training related to COVID-19.Thus,increased advocacy and awareness among the residents and the head of the urology training program regarding resident safety and related COVID-19 training could provide a way forward.The residents who received COVID-19 training were more confident as compared to the ones who did not.However, the question did not specifically explore the effect of training on residents’ awareness.
During the COVID-19 pandemic, some of the residents’duties were diverted to facilitate COVID-19 care, which could cause higher stress [6,10].In Indonesia, only 11.9% of urology residents participated in COVID-19-related duties on top of their usual daily tasks.Moreover, half of them were not willing to become COVID-19 volunteers.The lack of contribution might be caused by fear toward severe acute respiratory syndrome coronavirus 2 and its risk for the residents’ families [11,12].Such fears can be alleviated by disseminating accurate COVID-19 knowledge and assuring the availability of personal protective equipment [6,13,14].
As seen from different residency fields worldwide, a decrease in the clinical and surgical activity of urology residents during the COVID-19 pandemic was inevitable[7,15,16].The decrease in residents’ involvement was more clearly seen in surgical activity(endoscopic and open surgery).The findings were coherent with a previous study, which showed that 70% of urologists in Indonesia decreased more than 66% of their elective surgeries or stopped all the elective surgeries during the COVID-19 pandemic [5].A clear decrease in both clinical and surgical activity was also shown in Italy by Busetto et al.[16],specifically in the more prevalent COVID-19 region and COVID-19 hospital.Even though the residents felt unsure about their satisfaction on case exposure during the COVID-19 pandemic, green and yellow competency level residents felt unsatisfied.Moreover, this COVID-19 situation also decreased the relationship between colleagues during residency training [16].
The declining residents’ involvement in clinical and surgical activities explained why urology residents felt a lighter workload during the COVID-19 pandemic.The study showed different results from France,which indicated a higher level of stress during the pandemic.This factor may be attributable to lighter workloads and lower involvement in COVID-19-related tasks for urology residents in Indonesia[6].
Even though some of the residents still maintained in-person educational activities, the study showed that most of them switched to the web-based video conference method.Virtual learning was recommended to maintain relevant educational activities; however, maintaining physical distance was the highest priority.Even though this study could not show the superiority of the duty report,the patient assessment or lecture using web-based video conference compared to in-person activity denotes that the residents considered the former more effective.Many of the residents also used a smart learning method,such as joining a national or international speaker webinar or watching a recorded video, and considered it effective for learning and recommended it to be used as an integral part of urology resident training.The effectiveness of webinars as a “cognitive” learning method compared to the face-to-face meeting was showed by Hameed et al.[17].Furthermore, webinars were also considered more cost-effective and practical for urology residents.However, webinars limited the social networking interactions that would have been made in an offline seminar.We propose a hybrid meeting as a part of the urology resident training program in the future, where the practicality of an online webinar is held in conjunction with a face-toface meeting in hopes of reaching a broader audience.However, we also should be aware that this method is more beneficial in terms of cognitive area.Therefore, we also have to find a better method for resident’s surgical skill training during this pandemic.
Overall, urology residents in Indonesia felt unsure whether training experiences during the COVID-19 pandemic were comparable to the status before the pandemic.The residents expect that the reopening of affiliated hospitals rotations, an increased focus in phantom model training, and online discussions can overcome the lack of training experiences during the COVID-19 pandemic.However, extending the study period was not their choice.Other studies also encouraged an alternative learning approach to adapting to the current situation,such as free access to surgical video libraries, using software to learn anatomy and surgery in tandem with simulation[15,18,19].
The authors are aware that this study might have a limitation due to the nature of survey studies wherein respondents could easily misunderstand the questions and options given within a questionnaire.Moreover, the situation of the COVID-19 pandemic grows dire daily and could yield different situations compared to the one described in this study.However, this research still has value regarding how the pandemic affected urology residents’ training experiences.Furthermore, this study also assessed several learning methods used during the COVID-19 pandemic and highlighted how they might be helpful in the future of urology resident training.
5.Conclusion
It can be concluded that the COVID-19 pandemic has impacted the clinical, surgical, and educational activities of urology residents, which tended to be more negative.Nevertheless, the pandemic has also helped identify new learning methodologies, which could be an integral part of future urology resident training.
Author contributions
Study concept and design: Ponco Birowo, Nur Rasyid,Chaidir A.Mochtar.
Data acquisition: Ponco Birowo, Bambang S.Noegroho,H.R.Danarto, Besut Daryanto, Lukman Hakim.
Data analysis: Dyandra Parikesit, Fakhri Rahman.
Drafting of manuscript: Dyandra Parikesit, Fakhri Rahman,S.Cahyo Ariwicaksono.
Critical revision of the manuscript:Ponco Birowo,S.Cahyo Ariwicaksono.
Conflicts of interest
All authors declare no conflict of interest.
Acknowledgements
We want to express our gratitude to Dr.Ario Baskoro for creating our study figures and all chiefs of Urology residents in each Urology center to help in questionnaire distribution.This study was supported and financed by International Publication Research Grant Universitas Indonesia (Grant number: NKB-1535/UN2.RST/HKP.05.00/2020).
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2021.12.005.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
- The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
