Current knowledge and contemporary management of non-A non-B aortic dissections
Konstantinos C Christodoulou,Dimos Karangelis,Gioultzan Memet Efenti,Panagiotis Sdrevanos,Jennifer R Browning,Fotis Konstantinou,Efstratios Georgakarakos,Fotios A Mitropoulos,Dimitrios Mikroulis
Konstantinos C Christodoulou,Dimos Karangelis,Jennifer R Browning,Fotis Konstantinou,Dimitrios Mikroulis,Department of Cardiac Surgery,Democritus University of Thrace,University Hospital of Alexandroupolis,Alexandroupolis 68100,Greece
Gioultzan Memet Efenti,Department of Surgery,Didimotichon General Hospital,Didimotichon 68300,Greece
Panagiotis Sdrevanos,Cardioiasis Cardiology Clinic,Xanthi 67100,Greece
Efstratios Georgakarakos,Department of Vascular Surgery,University Hospital of Alexandroupolis,Democritus University of Thrace,Alexandroupolis 68100,Greece
Fotios A Mitropoulos,Department of Cardiac Surgery,Mitera Hospital,Athens 15123,Greece
Abstract Non-A non-B aortic dissection (AAD) is an infrequently documented condition,comprising of only a small proportion of all AADs.The unique anatomy of the aortic arch and the failure of the existing classifications to adequately define individuals with non-A non-B AAD,have led to an ongoing controversy around the topic.It seems that the clinical progression of acute non-A non-B AAD diverges from the typical type A and B dissections,frequently leading to serious complications and thus mandating early intervention.Currently,the available treatment methods in the surgical armamentarium are conventional open,endovascular techniques and combined hybrid methods.The optimum approach is tailored in every individual case and may be determined by the dissection’s location,extent,the aortic diameter,the associated complications and the patient’s status.The management of non-A non-B dissections still remains challenging and a unanimous consensus defining the gold standard treatment has yet to be reached.In an attempt to provide further insight into this perplexing entity,we performed a minireview of the literature,aiming to elucidate the epidemiology,clinical course and the optimal treatment modality.
Key Words: Aortic dissection; Aortic disease; Aortic surgery; Thoracic aorta disease; Aortic arch dissection
INTRODUCTION
As part of the cluster of the clinical entities related to acute aortic syndromes[1],acute aortic dissection (AAD) is a challenging and life-threatening cardiovascular emergency[2],with approximately 6 new cases per 100000 population per annum[3].In an AAD,an intimal tear compromises the medial layer’s structural integrity,separating the aortic wall layers.Subsequently,a “new” false lumen is formed,allowing blood to enter the tunica media[3].If not addressed,it has a significant propensity for developing into a fatal disorder due to rupture,myocardial infarction,cardiac tamponade,aortic valve insufficiency[4],or even end-organ malperfusion[5].Since the second half of the previous century,the Stanford and DeBakey classifications are the primary systems,which have consistently determined the patients’ management.However,by default,they both fail to distinguish and address dissections confined or involving the aortic arch[5].von Segesseretal[6] were the first to introduce the term “non-A non-B” when referring to intima tears sparing the ascending aorta.
Non-A non-B AAD can be defined as an entry intimal tear,located beyond the left subclavian artery (LSA),with the dissection extending retrogradely into the aortic arch (descending entry type),or as an entry tear located between the innominate and the LSA (arch entry type),with or without distal extension of the dissection[7].It seems that there is scarcity of data regarding their natural history,clinical course and management[8].Accordingly,we performed a minireview of the literature,to unveil the details of the topic with regards to epidemiology,contemporary classification systems as well as the available surgical armamentarium and possible treatment options.
EPIDEMIOLOGY,RISKS AND PREDISPOSING FACTORS
Non-A non-B AAD is an infrequently documented condition,comprising only a small proportion of all AADs.Its comparatively elevated mortality,hinders the ascertainment of its true incidence,since a considerable number of patients die prior to the diagnosis[2].Regardless of the divergent results across different studies,a recent review exhibited that the incidence of non-A non-B AAD lies between the respective of type A and type B,varying from 2.8% to 16.5%[5].The affected individuals tend to be 5 to 10 years younger in comparison to patients with other AADs[9],while some disagreement exists as to whether or not there is a prevailing type of location for the entry tear (arch or descending)[10,11].
There are several risk factors associated with non-A non-B AADs,with chronic and mainly poorly controlled hypertension being the most frequently reported.In the majority of the published cases,roughly 80% of the patients have a medical history of hypertension[5,8,10,12,13].Tobacco addiction,hypercholesterolemia and diabetes mellitus were also found to pose a great risk for AAD.In addition,connective tissue disorders like Ehlers-Danlos and Marfan Syndromes,inflammatory vasculitis,pregnancy,trauma,previous heart surgery,the presence of bicuspid aortic valve,stimulant usage,infections and some very rare genetic disorders are among the predisposing medical conditions linked to AAD[2].Additionally,a non-A non-B dissection can be attributed to an intramural hematoma and penetration aortic ulceration[1].
Furthermore,the role of other factors has also been investigated.Recent papers have exhibited a correlation between this specific type of AAD and anatomic characteristics of the aortic arch.Rylskietal[12] demonstrated that arch types are distributed variably among different dissections.Type I in which the vertical distance between innominate artery and the top of the aortic arch is less than the diameter of the left common carotid artery (LCCA),was usually seen in type A AADs,while in non-A non-B AADs arch type II (vertical distance between innominate artery and aortic arch is equal or twice the diameter of the LCCA) prevailed (49%).In approximately 1/3 of the non-A non-B patients (28%),two instead of the three branches arise from the arch,since the innominate and the LCCA were found to share a common trunk and in 16% of the cases the left vertebral artery arose directly from the arch[10].Irrespective of these variations,the aortic arch’s curved shape and its branches,form two natural barriers,which can prevent a dissection from spreading further.The origin of the innominate artery serves as the proximal barrier,while the distal barrier is considered to be the LSA.As a result,these margins may be incriminated as the two very distinctive arch and descending entry dissection types[11].
CLINICAL PRESENTATION
In most cases of AAD,the most common symptom is sudden,acute chest pain and/or back discomfort[3].Nevertheless,in rare cases a subtle or discrete type of AAD[3] has been reported,which is typically detected intraoperatively,despite being misdiagnosed during the patient’s initial assessment[14].Wangetal[15] in their retrospective study,stated that all non-A non-B patients reported an abrupt onset of severe chest pain for at least a six-hour duration.Notably,a recent meta-analysis showed that nearly 50% of the patients were admitted with or developed over time,signs of at least one organ malperfusion and that 6% were at risk of an impending rupture[8].In the same paper,the authors highlighted the surprisingly large proportion of patients (88%),who had a complicated clinical course,as distinct from type B dissections.Hence,cardiogenic shock,cardiac arrest,cardiac tamponade,periaortic hematoma,acute renal failure,stroke/neurologic deficits or even aortic rupture are some of the baseline characteristics of non-A non-B dissection patients[13].
CLASSIFICATION SYSTEM
Over the years and with the exploitation of the emerging imaging modalities,several classification systems have been proposed and deployed to facilitate the triage and enhance the post-treatment clinical outcomes.The two traditional and widely known DeBakey and Stanford classifications were introduced in the 1950s and 1960s,respectively,and are based on the intimal tear’s location and extension[16,17].It is evident,that since the aforementioned systems focus primarily on the ascending and descending part of the aorta,they lack clarity regarding aortic arch involvement[4].
The European Society of Cardiology guidelines about aortic diseases fail to include the arch dissection as a distinct entity.The American Heart Association guidelines propose the term “proximal type B aortic dissection” for patients with entry tears in the arch,expanding antegradely to the descending aorta[18,19].The 2019 consensus of the European Association for Cardio-Thoracic Surgery and the European Society for Vascular Surgery,referred to non-A non-B AAD,as an arch involvement either by the most proximal tear or by retrograde extension,but sparing the ascending aorta[20].
Since the introduction of the term non-A non-B AAD back in 1994[6],several studies have proposed the modification of the already existing classifications,by adding this type of dissection.Based on the entry tear’s location,in 2017,non-A non-B AADs were divided into two distinct groups; arch and descending entry tear[10].Recently,Qanadlietal[4] driven by the Stanford classification,proposed the incorporation of “type C” AAD,referring to the corresponding non-A non-B dissection suggested earlier by Rylskietal[10].For the first time,they also mention,grades of malperfusion syndrome (MPS grade 0-3).More specifically,the absence of malperfusion is classified as grade 0,compression of the true lumen as grade 1,while the extension of the dissection to renal artery is categorized as grade 2.According to the authors grade 3 incorporates both the absence of malperfusion and the extension of the dissection to the renal artery.Therefore,the MPS grade dictates the need for additional therapy to maintain perfusion of vital organs.
Sieversetal[9] extended the Stanford classification by including all types of AAD,the location of primary aortic entry tear and the malperfusion status (TEM).According to their proposal,T refers to type A,type B or non-A non-B dissections,E includes E0: No visible entry site,E1: Entry tear in ascending aorta,E2: Tear in arch,E3: Tear in descending aorta and M includes M0,M1,M2,M3 when no malperfusion,coronary artery,subra-aortic arteries,renal/visceral ± lower extremity arteries were involved,respectively.They also mention the presence (+) and absence (-) of clinical symptoms of organ malperfusion offering a more complete picture of AADs in an attempt to achieve optimal therapeutic planning and outcome[9].
TREATMENT MODALITIES
Decision on optimal medical treatment of AADs is determined based on the dissection’s location,extent,the aortic diameter,the accompanying complications,the adjacent anatomy,the patient’s status and comorbodities[21].Stanford type A/DeBakey type I or II dissections,when left untreated,typically have a mortality rate exceeding 50% the first 48 h,so open surgery on emergency basis with replacement of the ascending aorta is highly recommended[3,19].On the other hand,when the dissection involves solely the descending thoracic aorta (DTA) (Stanford type B/DeBakey type III dissections),the clinical course is usually uncomplicated.When that is the case,the 30-d mortality rate is approximately 10%,thus,conservative medical therapy or interventional,endovascular treatment (for complicated type B dissections) are the most common,yet not exclusive,treatment options[3,19].However,aortic arch dissections have not been accurately classified,which leads to uncertainty and disagreement on treatment planning[4].In addition,the contribution of the imaging modalities,towards an accurate diagnosis should not be omitted.The transthoracic echocardiography,although mostly employed in nonemergency cases,could potentially provide useful details regarding the proximal DTA,the aortic arch branches and detect some of the dissection’s complications[19].Yet,the valuable role of the preoperative computed tomography is constantly increasing,as it can sometimes detect the dissection and its extent,delineate the anatomy of the area,and even depict clinically significant incidental findings[22],enhancing the diagnostic accuracy and tailoring the treatment plan[19].
Aiming for the closure of the proximal entry tear,a great number of research papers have suggested the implementation of surgical treatment for non-A non-B AADs,explicitly exhibiting that conservative treatment is inferior to any type of intervention,presenting a 30-d mortality rate of 14% as compared to 3.6% for surgically or endovascularly treated patients[8].According to recent data,it seems that the clinical manifestation and progression of acute non-A non-B AAD diverge from the typical type A and B dissections and especially from the acute type B AAD,which is confined to the DTA[23].Valentineetal[24] noted that dissections including the arch had a worse outcome than those affecting only the DTA.Equally important results from an expert consensus state that the arch’s involvement in the dissecting process has an immense impact on the patients’ outcome,including but not limited to the prolonged hospital stay,the increased probability of cardiac and neurologic complications such as rupture,congestive heart failure,MPS,stroke,spinal cord injury (SCI) and the need for reintervention if not addressed betimes[20,25].
Because non-A non-B AADs are associated with an increased likelihood of a complicated course,the optimal management orders early intervention[5].In spite of the fact that,during the past years,many therapeutic plans have been proposed,there remains a dearth of literature regarding pertinent studies comparing different modalities for the treatment of non-A,non-B AAD.Moreover,the existing studies have limited patient samples and lack long-term follow-up[21].Therefore,a unanimous consensus defining the gold standard treatment has yet to be reached[5].Currently,the available treatment options in the surgical armamentarium are conventional open surgery with standard aortic arch replacement or frozen elephant trunk (FET),interventional therapies such as the thoracic endovascular aortic repair (TEVAR) with extra-thoracic surgical transposition or chimney stent graft and hybrid techniques combining TEVAR with debranching of the supra-aortic vessels[8].Lately,a new hybrid technique was launched by Wangetal[15] with satisfactory short-term outcomes,called the “inclusion aortic arch technique”,as an alternative to the traditional hybrid surgery,so to avoid endoleaks and retrograde type A dissection,which may complicate the procedure.
According to the International Registry of Acute Aortic Dissection study findings,arch entry and DTA entry type dissections differ from one another in terms of their course.More specifically,a DTA dissection,expanding retrogradely to the arch,has no impact on either early or late mortality or the management plan,with its clinical course resembling that of type B AAD.Whereas complicated arch entry dissections with antegrade expansion to the DTA,were found to have an elevated in-hospital mortality,requiring an even more urgent intervention[13,25].Trimarchietal[13] also presented data which argue that non-A non-B AAD should perhaps warrant a more aggressive approach.In their analysis,14% of patients with an “uncomplicated” arch tear had progression of the dissection,which likely contributed to a 30% incidence of lethal stroke.In the same frame,Kosiorowskaetal[7] stressed/pointed out the contemporary tendency towards an earlier intervention on the altar of a favorable aortic remodeling.In arch entry type patients,open aortic arch repair is preferable compared to endovascular techniques in term of survival and post-operative complications rate[7].In these cases,there are several arch replacement grafts commercially available (Figures 1 and 2).
The arch entry dissections,can be managed with standard aortic arch replacement combined with FET,as the procedure is associated with low peri and post-operative mortality and complication rates[7].Hybrid methods have been proposed as an effective alternative,which can prevent the need for cardiopulmonary bypass,hypothermic cardiac arrest and any related problems,but their efficacy has not yet been proven in the long run[26].However,the study conducted by Tianetal[27],employing different hybrid methods (type I-III) to treat 46 patients,has demonstrated promising outcomes with respect to overall mortality and complication rates,in comparison to surgical or endovascular repair.Taking into account the lack of guidelines regarding postoperative thromboprophylaxis,caution must be exerted to avoid the graft’s occlusion[28].Irrespective of the entry type,evidence shows that TEVAR is a valid treatment option provided that the aortic arch has favorable anatomy[8].Alternatively,when the entry tear is located in zone 1,a hybrid arch repair,aortic arch replacement or even FET should be given thorough consideration[8].This minireview focuses primarily on the FET and TEVAR techniques.

Figure 1 Pre-operative computed tomography images of a non-A non-B aortic dissection case contained in the aortic arch,which was surgically managed in our department.
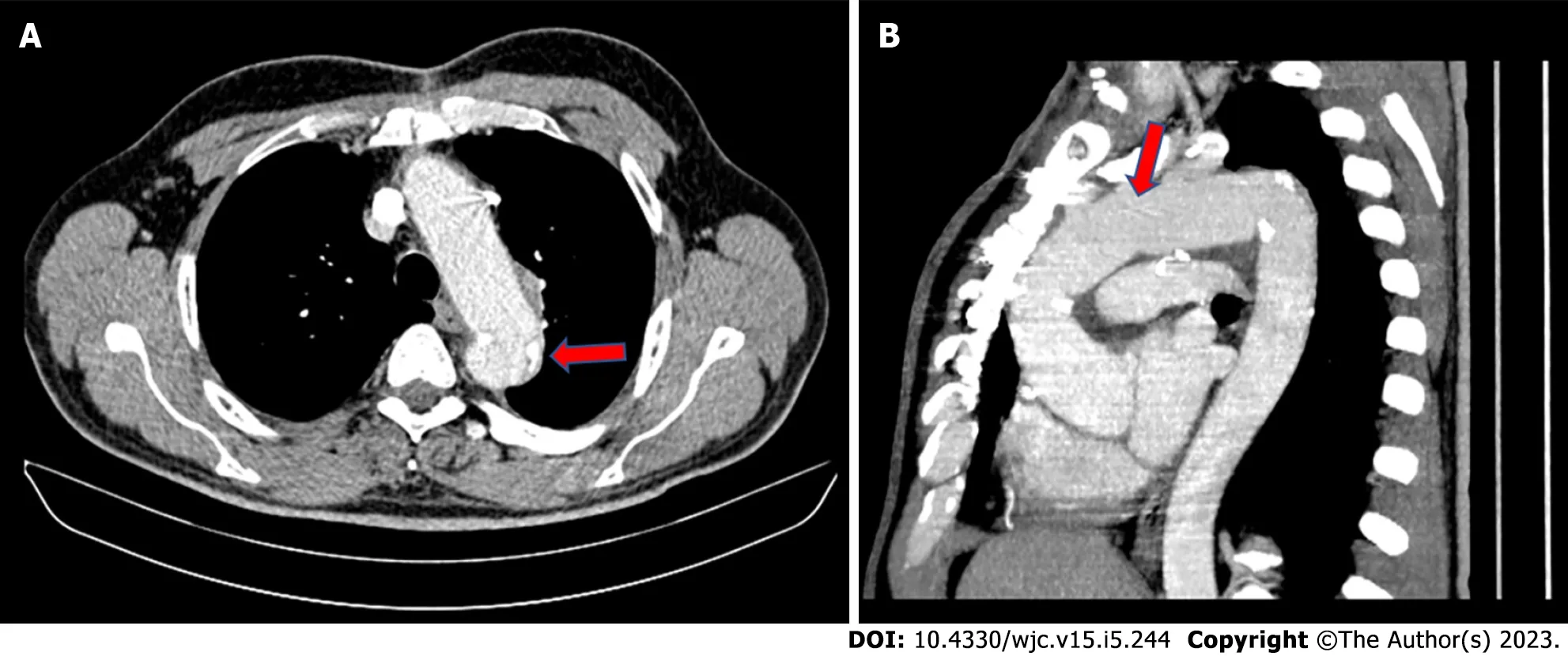
Figure 2 The aortic arch was replaced with a graft (prefabricated aortic branched graft),which contained three pre-attached branches for all three great vessels.
ET AND FET
Treatment of non-A non-B AAD can be performed with a two-stage surgical technique called “ET”[29].The first stage of ET includes a sternotomy and a reconstruction of the ascending aorta and the aortic arch with a graft while in the second stage,the floating extension of the graft (ET) in the descending aorta is utilized in order to extend the repair of the DTA.The second stageperseincludes a lateral thoracotomy to approach the descending aorta.The evolution of surgical and endovascular techniques has resulted in the development of a composite prosthesis,known as the “Frozen ET”[20].The use of FET instead of the conventional ET has been increasing over the last years[20].
Combining the benefits of both open and interventional repair,FET is a viable solution in cases of a proximal entry tear as well as for patients with non-A non-B AAD or complicated chronic type B,who are not suitable for TEVAR[30,31].This one-stage procedure allows a total aortic arch replacement with antegrade delivery of a descending aortic stent-graft[32].The stent-graft may serve as a proximal landing zone to facilitate future endovascular intervention in the distal aorta[30].The FET technique has been extensively applied in cases of acute dissections to restore true lumen patency,seal intimal tears in the descending aorta and promote false lumen thrombosis,as well as repairing chronic degenerative arch aneurysms[19,32].FET implantation has the potential to prevent secondary thoracic and abdominal aortic replacement by enlarging the true lumen and promoting favorable remodeling of the distal aorta[19,33,34].Yet,if replacement of the thoracic and abdominal aorta is required,its additional suture margins at each side,facilitate anastomosis[5,30].The two most common commercially available hybrid FET prostheses namely the Thoraflex hybrid and E-vita open are associated with comparable outcomes[20].
Carinoetal[8] mention that 7% of the non-A non-B patients underwent the FET procedure,pointing out that it should be considered in complicated cases,since it alleviates the compressed true lumen and covers any newly formed entry tears in the proximal DTA,applying pressure to the false lumen.Zhaoet al[35] reported the in-hospital mortality rate of their 24 non-A non-B AAD patients treated with FET,to be 4.1%,while the 5-year survival rate was approximately 92%.The authors concluded that,this surgical technique represents a feasible option with acceptable short and long-term outcomes.Another study cohort,whilst exhibiting similar early results,stresses the importance of the continuous monitoring and follow-up,due to the potential need for aortic reintervention[31]; results in accordance with Tianetal[27] paper.
Although the technique is more invasive than TEVAR,it minimizes the risk of type Ia endoleaks and retrograde type A dissection[30].On the other hand,FET’s primary disadvantage is the increased risk of surgical trauma brought on by the necessity for extended periods of extracorporeal circulation,circulatory arrest,myocardial ischemia,stroke and SCI,due to the extensive coverage of the descending aorta with the occlusion of intercostal arteries[8].Additionally,aortic valve insufficiency,bovine aortic arch,the dissection of the LCCA and preoperative cardiopulmonary resuscitation have all been linked to an increased risk for postoperative stroke[36,37].Notably,in many studies,including a meta-analysis with 3000 “aortic surgical” patients,SCI was documented in 4% of the cases.By diminishing the circulatory arrest time and FET maneuvers above the 8ththoracic vertebra,SCIs could be substantially reduced[38].Cerebrospinal fluid drainage and neuromonitoring should also be carried out for high-risk patients[39].
TEVAR
TEVAR,given its minimal invasive character,has recently been shown to be the most widely used technique to treat non-A non-B dissections,comprising 55% of the treatment[8].The aim of the stentgraft’s deployment in the thoracic aorta is the successful closure of the primary entry tear.As a result,the false lumen is excluded from the systemic circulation,thrombosed and shrank,thus it no more compresses the true lumen and organ perfusion is maintained.According to the location of the primary entry tear,different TEVAR sealing zones exist (zone 0,1,2,3).Zone 3 TEVAR refers to entry tears located in the DTA with retrograde extension,with the stent-graft deployed distal to the LSA.For more proximal entry tears,zone 2 TEVAR is employed,which includes a sealing zone between the origin of the LCCA and the LSA.TEVAR zone 1 refers to graft apposition between the innominate artery and LCCA,while TEVAR zone 0 includes a sealing zone proximal to the innominate artery[3,5,10,20].
In order to establish a disease-free sealing zone,the sacrifice of important aortic arch branches can be,in some cases,unavoidable.Nonetheless,there are several techniques to maintain perfusion; supraaortic branch bypass (hybrid technique),apposition of extra stent-grafts (chimney technique) or both[40].TEVAR zone 2 can be accompanied with carotid-subclavian (CS) bypass/transposition or with chimney graft to the LSA.Similarly,TEVAR zone 1 can be followed by two chimney grafts to the LCCA and LSA,but more frequently,a single chimney graft to the LCCA and a CS bypass/transposition are used.Finally,TEVAR zone 0 can entail two chimney grafts to the innominate artery and LCCA followed by a left CS bypass,or alternatively a chimney graft to the innominate artery,right to left carotid bypass and CS bypass[20].Compared to more distal landing zones,zone 0 is more likely to be associated with retrograde type A dissection,especially when accompanied by excessive oversizing of the stent-graft[41].Yet,it has also been demonstrated that the use of chimney grafts in the aortic arch,increases the risk of post-operative complications[40].
Liuetal[21] studied 215 patients with a non-A non-B AAD,treated with TEVAR,open surgical techniques or conservatively.TEVAR was used in 127 patients (59.1%) with a success rate of 85.9%.The 30-d mortality rate was 1.6%,compared to 7.1% in patients treated with open techniques.However,during the follow up,9 deaths occurred in the endovascular group,5 of which were related to the dissection,while no deaths occurred in the surgical group.Supplementary,following TEVAR,patients had a worse clinical outcome in terms of aortic rupture,retrograde type A dissection,distal stent graft induced new entry,major stroke and the need for reintervention.Likewise,a study published in 2022,observed that 67% of the initial TEVAR cases (10/15),demanded reintervention,with eventually 4 patients deceasing during the first 30 d[7].
CONCLUSION
Management of non-A non-B dissections remains challenging.The paucity of relevant studies reflects the fact that non-A non-B AADs account for a relatively modest percentage of all AADs.Although little is known about their natural history and course of treatment,it has been explicitly shown that surgical intervention surpasses medical treatment in the case of a non-A non-B dissection[5,8,42].Current data advocate that this clinical entity does not behave like an uncomplicated type B AAD,and perhaps a more aggressive approach is warranted.Open repair is mostly employed in arch entry,while TEVAR with hybrid procedures in descending entry dissections both of which are thought to be preferable as opposed to conservative treatment.Secondary analysis with long-term follow up of the existing studies as well as large prospective clinical trials will enlighten the field around non-A non-B AAD which still remains an obscure and perplexing variation of acute AAD.Future research is anticipated to determine the most optimal surgical method as well as the time to intervene,ultimately helping surgeons to navigate through these uncharted waters.
FOOTNOTES
Author contributions:Christodoulou KC wrote the manuscript; Karangelis D contributed to manuscript review and supervised the entire project; Efenti GM,Sdrevanos P,and Georgakarakos E contributed with bibliographic research and proofread the manuscript; Browning JR was responsible for the English language editing of the manuscript; Konstantinou F provided the accompanying figures; Mitropoulos FA and Mikroulis D designed the outline and coordinated the writing of the paper; and all authors have read and approved the final manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Greece
ORCID number:Konstantinos C Christodoulou 0000-0002-5807-9212; Dimos Karangelis 0000-0001-7633-9949; Gioultzan Memet Efenti 0000-0002-0030-0500; Jennifer R Browning 0000-0001-6942-9292; Efstratios Georgakarakos 0000-0003-3789-1110.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Yu HG
 World Journal of Cardiology2023年5期
World Journal of Cardiology2023年5期
- World Journal of Cardiology的其它文章
- Acute heart failure as an adverse event of tumor necrosis factor inhibitor therapy in inflammatory bowel disease: A review of the literature
- Atrial fibrillation and coronary artery disease: An integrative review focusing on therapeutic implications of this relationship
- Importance of concomitant functional mitral regurgitation on survival in severe aortic stenosis patients undergoing aortic valve replacement
- Impact of erythropoietin therapy on cardiorenal syndrome: A systematic review with meta-analysis
- Extracorporeal veno-venous ultrafiltration in congestive heart failure: What’s the state of the art? A mini-review
- Pharmacoepidemiologic study of association between apparent treatment resistant hypertension,cardiovascular disease and interaction effect by sex and age
