Pharmacoepidemiologic study of association between apparent treatment resistant hypertension,cardiovascular disease and interaction effect by sex and age
Julianne Theresa Nelson,Longjian Liu
Julianne Theresa Nelson,Longjian Liu,Department of Epidemiology and Biostatistics,Dornsife School of Public Health,Drexel University,Philadelphia,PA 19104,United States
Abstract BACKGROUND A limited number of studies have been conducted to test the magnitudes of the association between apparent treatment resistant hypertension (aTRH) and risk of cardiovascular disease (CVD).AIM To investigate the association between aTRH and risk of CVD and examine whether sex and age modify this association.METHODS We applied an observational analysis study design using data from the United States Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).ALLHAT recruited participants (n = 25516) from 625 primary care settings throughout the United States,Canada,Puerto Rico,and United States Virgin Islands,aged 55 and older with hypertension and at least one additional risk factor for heart disease.aTRH was assessed from the year 2 visit.CVD event was defined as one of the following from the year 2 follow-up visit: Fatal or non-fatal myocardial infarction,coronary revascularization,angina,stroke,heart failure,or peripheral artery disease.Cox proportional hazards regression was used to examine the effect of aTRH on CVD risk.Potential modifications of sex and age on this association were examined on the multiplicative scale by interaction term and additive scale by joint effects and relative excess risk for interaction.RESULTS Of the total study participants (n = 25516),5030 experienced a CVD event during a mean of 4.7 years follow-up.aTRH was associated with a 30% increase in risk of CVD compared to non-aTRH [hazards ratio (HR) = 1.3,95%CI: 1.19-1.42].Sex and age modified this relationship on both multiplicative and additive scales independently.Stratified by sex,aTRH was associated with a 64% increase in risk of CVD (HR = 1.64,95%CI: 1.43-1.88) in women,and a 13% increase in risk of CVD (HR = 1.13,95%CI: 1.01-1.27) in men.Stratified by age,aTRH had a stronger impact on the risk of CVD in participants aged < 65 (HR = 1.53,95%CI: 1.32-1.77) than it did in those aged ≥ 65 (HR = 1.18,95%CI: 1.05-1.32).Significant two-way interactions of sex and aTRH,and age and aTRH on risk of CVD were observed (P < 0.05).The observed joint effect of aTRH and ages ≥ 65 years (HR = 1.85,95%CI: 1.22-2.48) in males was less than what was expected for both additive and multiplicative models (HR = 4.10,95%CI: 3.63-4.57 and 4.88,95%CI: 3.66-6.31),although three-way interaction of sex,age,and aTRH on the risk of CVD and coronary heart disease did not reach a statistical significance (P > 0.05).CONCLUSION aTRH was significantly associated with an increased risk of CVD and this association was modified by both sex and age.Further studies are warranted to test these mechanisms.
Key Words: Apparent treatment resistant hypertension; Cardiovascular disease outcomes; Chronic kidney disease; Sex; Age
INTRODUCTION
Hypertension has long been a serious public health concern.Its impact on cardiovascular health and long-term outcomes has been well studied[1].In the United States approximately 121.5 million (47.3%) adults suffer from hypertension leading to an added economic burden costing up to $51.1 billion per year[2].One of the significant challenges in control of hypertension is the appearance of treatment resistant hypertension.
Treatment resistant hypertension is defined as having blood pressure (BP) that remains uncontrolled [systolic BP (SBP) ≥ 140 mmHg or diastolic BP (DBP) ≥ 90 mmHg] while a patient is on ≥ 3 different antihypertensive medications.Additionally,those who are on 4 or more different classes of antihypertensive medications,regardless of BP are also classified as treatment resistant hypertension.Individuals with diabetes or chronic kidney disease (CKD) have an altered definition,these patients with SBP/DBP ≥ 130/80 mmHg are classified as treatment resistant hypertension[3-5].In addition to the number of antihypertensive medications and BP readings,ideally at least one of the medications should be a diuretic[6].Apparent treatment resistant hypertension (aTRH) is used to define observed treatment resistant hypertension when factors relating to pseudoresistance (adherence to regimen,sufficient dose for therapy,etc.) are unknown[7].
It is estimated that 19.7% of patients on antihypertensive medication have aTRH,a 2% increase within the recent decade[3-5].While it is known that treatment of hypertension can reduce the risk of cardiovascular events and mortality,little research has been done on outcomes of those with resistant hypertension[3,8].Several cross-sectional studies have found relationships between aTRH and cardiovascular disease (CVD),however,longitudinal studies remain sparse[3,9].What has been observed is that aTRH is associated with higher rates of cardiovascular and renal diseases,including: Coronary heart disease (CHD),peripheral artery disease (PAD),stroke,heart failure (HF),end-stage renal disease,and all-cause mortality.Of particular note is that aTRH increased the risk of CHD by 44% and the risk of death by 30% compared to non-aTRH[9,10].
Men and women experience differing rates of hypertension and CVD[11,12].However,findings of sex-specific aTRH studies remain inconsistent[3,5,13-15].Women experience an increase in risk of hypertension post-menopause indicating a possible impact of sex and age on the risk of aTRH and CVD outcomes[12].
Of the many risk factors for CVD,age is one of the most important factors as age is an independent risk factor for the development of atherosclerosis[5,11,16,17].However,the degree of this effect does not impact men and women in the same way neither in the risk of incident hypertension nor in the progress of hypertension in clinical treatment[11,18].Several studies have observed that age is significantly and independently associated with risk of aTRH[3-5,14].However,studies of the potential modification effects of sex and age on the association between aTRH and risk of CVD are limited.In this study,we hypothesized that sex and age play an important role both independently and together in the risk of aTRH for CVD outcomes.To test this hypothesis,we examined the independent and additive effects of sex and age on aTRH and risk of CVD,and whether sex and age modify the association between aTRH and CVD risk.
MATERIALS AND METHODS
Study sample
We analyzed data from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).In ALLHAT,a total of 42418 participants aged 55 and older were recruited from 625 primary care settings throughout the United States,Canada,Puerto Rico,and United States Virgin Islands.Participants were randomly assigned into four groups and then received one of four antihypertensive treatment arms: Chlorthalidone,amlodipine,lisinopril,and doxazosin.Participants who received doxazosin are excluded in the analysis because this group was discontinued early.All participants had hypertension and at least one additional risk factor for CHD.Participants were followed for an average of 6 years[19-21].The study design and process of ALLHAT have been published in detail elsewhere[21].
This study,using de-identified data from the National Heart,Lung,and Blood Institute,has been approved by Drexel University Institutional Review Board (# 1608004781).
Measures
Exposure (aTRH): In ALLHAT the recruited participants were initially randomized to one of 4 first-line antihypertensive drugs.Additional anti-hypertensive medications were added on to therapy over the course of follow-up visits,thus,aTRH was determined at the year 2 visit to allow time for additional medications to be added,consistent with follow-up studies[10,21].aTRH was defined as BP ≥ 140/90 while on 3 antihypertensive medications,or being on 4 antihypertensive medications regardless of BP at the year 2 visit.For subjects with either type II diabetes or CKD (assessed by glomerular filtration rate,epidermal growth factor receptor (eGFR) < 60 mL/min),the cut-offs of SBP/DBP were set at ≥ 130/80 mmHg.Due to subjects being randomized to first-line anti-hypersensitive treatment,the condition that one medication be a diuretic for aTRH classification could not be applicable in the study.
Outcome (CVD): Subjects were classified as having had a CVD event if they experienced one of the following after the year 2 follow-up visit: Fatal or non-fatal myocardial infarction (MI),coronary revascularization,angina,stroke,HF,or PAD.These events were ascertained from follow-up visits and medical recording during the course of the trial[10].
Covariates: Covariates were selected based on their independent associations with both the exposure (aTRH) and outcome (CVD),existing literature,and use of a directed acyclic graph[10].All covariates were measured at baseline of ALLHAT.They included: Race (white,African American,American Indian/Alaskan Native,Asian/Pacific Islander,other),ethnicity (Hispanic),geographic region (East,Midwest,South,West,Canada,Puerto Rico/Virgin Islands),measures of GFR,SBP and DBP at baseline,and history of CHD,history of MI or stroke,history of coronary revascularization,previous use of BP medication,smoking status (current,former,never),history of left ventricular hypertrophy,estrogen use (in women subgroup analysis only),aspirin use,and enrollment in concurrent lipid lowering trial.
Statistics
Univariate analysis was conducted to describe the baseline characteristics of participants by aTRH status.Student’sttest was used to examine mean difference in continuous variables,and Chi-square tests to examine rate and proportion differences in categorical variables.We used Cox Proportional Hazards regression models to examine the association between aTRH and CVD risk with adjusting covariates.Assumptions of the proportional hazards in Cox model were tested graphically by log-log survival curves.To test potential modification effects of sex (menvswomen) and age (< 65vs≥ 65) on the association between aTRH and CVD risk,we assessed potential multiplicative interaction (e.g.,aTRH*modifier) on CVD risk.We also assessed potential additive interaction effects on CVD risk by estimating the joint effects and calculating the relative excess risk for interaction (RERI)[22].If the RERI ≠ 0 then there is evidence that the observed additive risk of our exposures is different (more or less depending on the direction of the RERI) than what was expected.The methods of the calculations and hypothesis tests for the RERI have been discussed and published in detail elsewhere[23].To test the overall interaction effect of sex and age and aTRH on CVD risk,we tested three-way interaction through a product interaction term (e.g.,aTRH*sex*age) in Cox models.Observed joint effects were compared to expected for both additive and multiplicative models to determine presence of effect modification and subgroup analyses were performed.
Sensitivity analyses: To avoid overfitting attributable to multiple control covariates,we applied a propensity score analysis technique[24].A propensity score for the probability of aTRH was estimated utilizing all confounders and created using the boosted CART method in the “twang” package in R software[25-27].Extreme weights were trimmed and inverse probability weighting was used to weight observations by the propensity score[24,28].Second,in the ALLHAT study,missing data in BP measures occurred at year 2 visit.We conducted a sensitivity analysis using Markov Chain Monte Carlo method for multiple imputation based on the randomness of the missing values[29].Third,because of the pathophysiologic differences between hemorrhagic and ischemic stroke,we conducted a subgroup of CVD analysis by strokes and CHD (fatal CHD or nonfatal MI,coronary revascularization,or hospitalized angina).Fourth,to control the effects attributable to the conclusion of patients who had uncontrolled hypertension (BP ≥ 140/90) but with < 3 medications (n= 11223),on the estimate of hazards ratio (HR) for CVD risk,we excluded this group of patients in the final sensitivity analysis.
Data analyses were conducted using SAS software (Version 9.4,SAS Institute Inc.,Cary,NC,United States).Statistical significance as set up at a two-sidedP< 0.05.
RESULTS
From the original sample of 42418 subjects in ALLHAT,those on the doxazosin treatment arm (9061) were removed early for safety reasons.After excluding subjects with CVD events or death prior to year 2,and those missing year 2 visit information we had an analytic study sample of 25516.During the follow-up (average 4.7 years),5030 (19.7%) participants had a CVD event.Table 1 shows baseline characteristics of the participants.
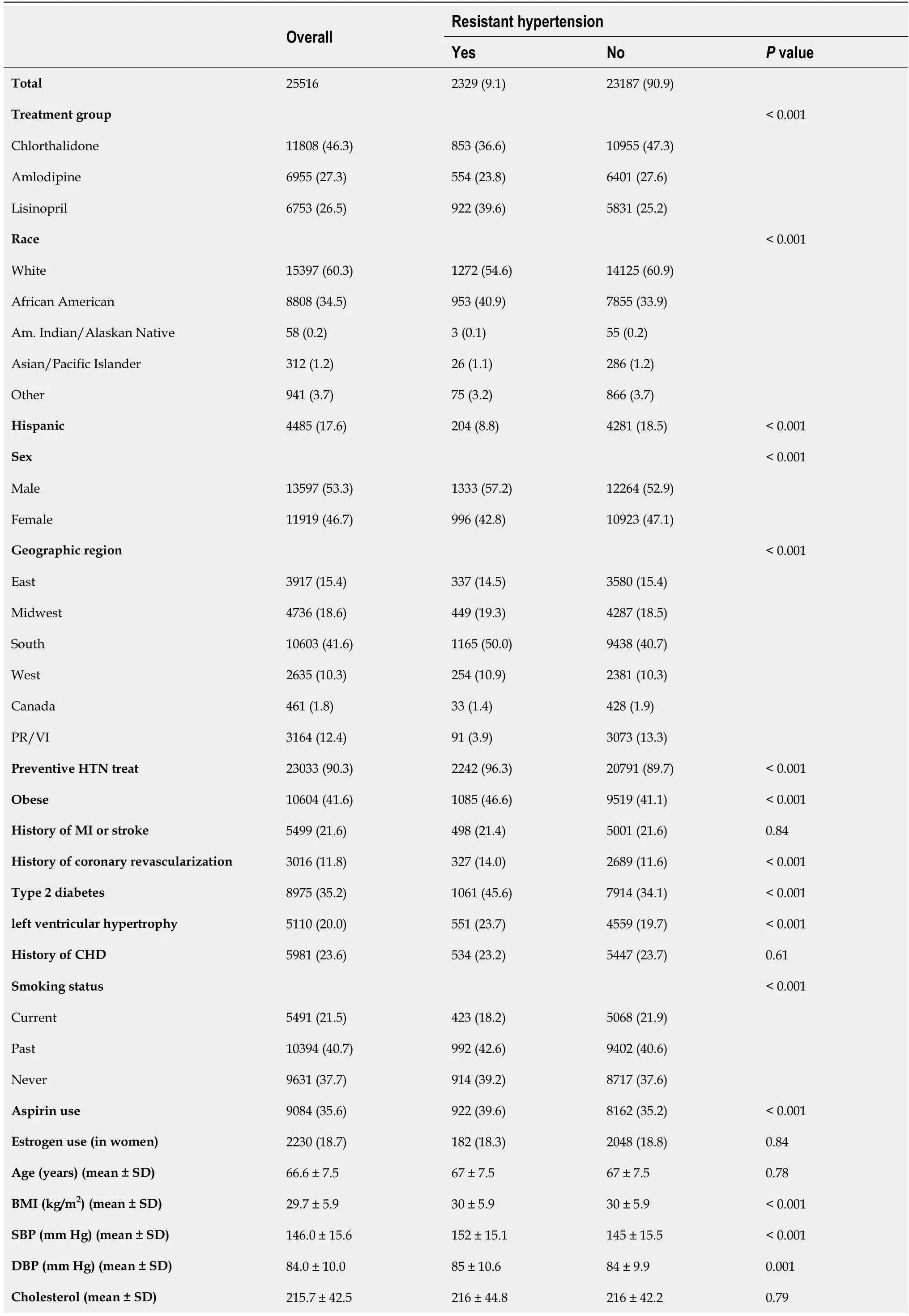
Table 1 Baseline characteristics overall and by apparent treatment resistant hypertension status,n (%)
HTN: Hypertension; MI: Myocardial infarction; CHD: Coronary heart disease; BMI: Body mass index; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; GFR: Growth factor receptor; PR: Puerto Rico; VI: United States Virgin Islands.
Overall subjects were more likely male (53.3%),from the South (41.6%),white (60.3%),and previously treated for hypertension (90.3%).Over a third (35.2%) had type 2 diabetes (T2DM),and 40.7% were former smokers.While over 40% of subjects were obese,the average body mass index (BMI) was 29.7 (SD 5.92).The average age was 66 years,and average GFR 78 mL/min.The rate of aTRH was 9.1% (n= 2329) in the total sample,9.8% in men,8.4%% in women,and 9.1% in those aged 65 and older.Subjects with aTRH were predominantly more likely to be African American,male,BMI ≥ 30 kg/m2,and T2DM than their corresponding counterparts.
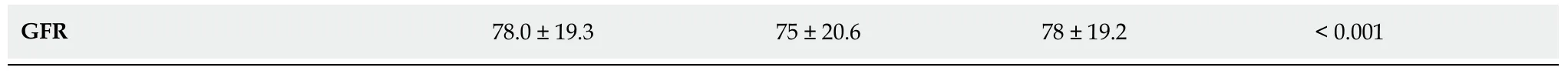
Table 2 shows that after adjustment for covariates,aTRH remained significantly associated with risk of CVD (HR = 1.30,95%CI: 1.19-1.42,P< 0.0001).
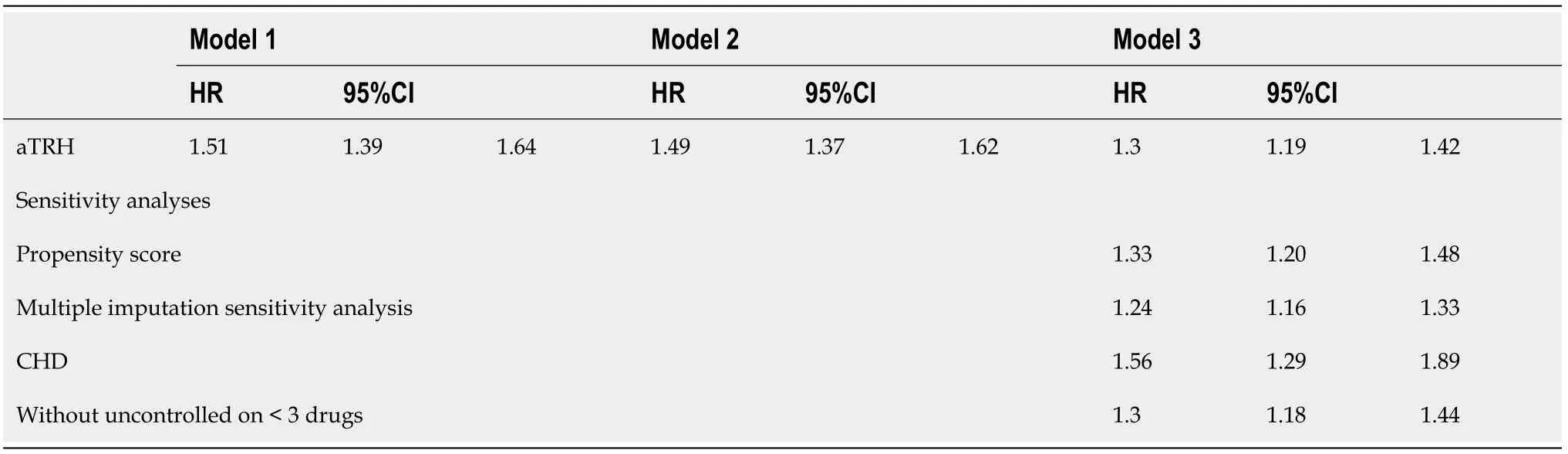
Table 2 Hazard ratios of apparent treatment resistant hypertension for cardiovascular disease risk and sensitivity analyses
Sensitivity analyses of propensity score for adjusting multi-covariates and multiple imputation for estimates of missing values produced similar results as did the analysis involving exclusion of participants with uncontrolled BP on < 3 medications.When CHD was examined as the endpoint instead of CVD,the overall risk associated with aTRH was stronger (HR = 1.56,95%CI: 1.29-1.89).
Table 3 shows individual and joint effects.Among women,aTRH was associated with a 64% increase in risk of CVD event (95%CI: 1.43-1.88),and a 13% increase in risk of CVD (95%CI: 1.01-1.27) among men.aTRH had a stronger impact on risk of CVD among younger subjects than it did among older (HR = 1.53,95%CI: 1.32-1.77 In those aged < 65,and HR = 1.18,95%CI: 1.05-1.32 in those aged 65 and older).All HRs were statistically significant and the two-way multiplicative interaction terms of sex*aTRH,and age*aTRH and RERIs on risk of CVD were statistically significant (P< 0.05).
Table 3 Joint effects for interaction of sex and apparent treatment resistant hypertension,and age and apparent treatment resistant hypertension on cardiovascular disease risk
Results stratified by aTRH,age,and sex can be found in Table 4 and Figure 1.Females aged 65 and older with aTRH had the highest risk of CVD (HR = 2.61,95%CI 2.20-3.01),followed by men < 65 years with aTRH (HR = 2.17,95%CI: 1.76-2.58).The observed joint effect (HR = 1.85,95%CI: 1.22-2.48) was less than expected for both additive and multiplicative models (HR = 4.10,95%CI: 3.63-4.57 and HR = 4.88,95%CI: 3.66-6.31 respectively).However,the three-way interaction term for sex,age and aTRH was not significant for CVD (P= 0.28),and CHD (P= 0.42).
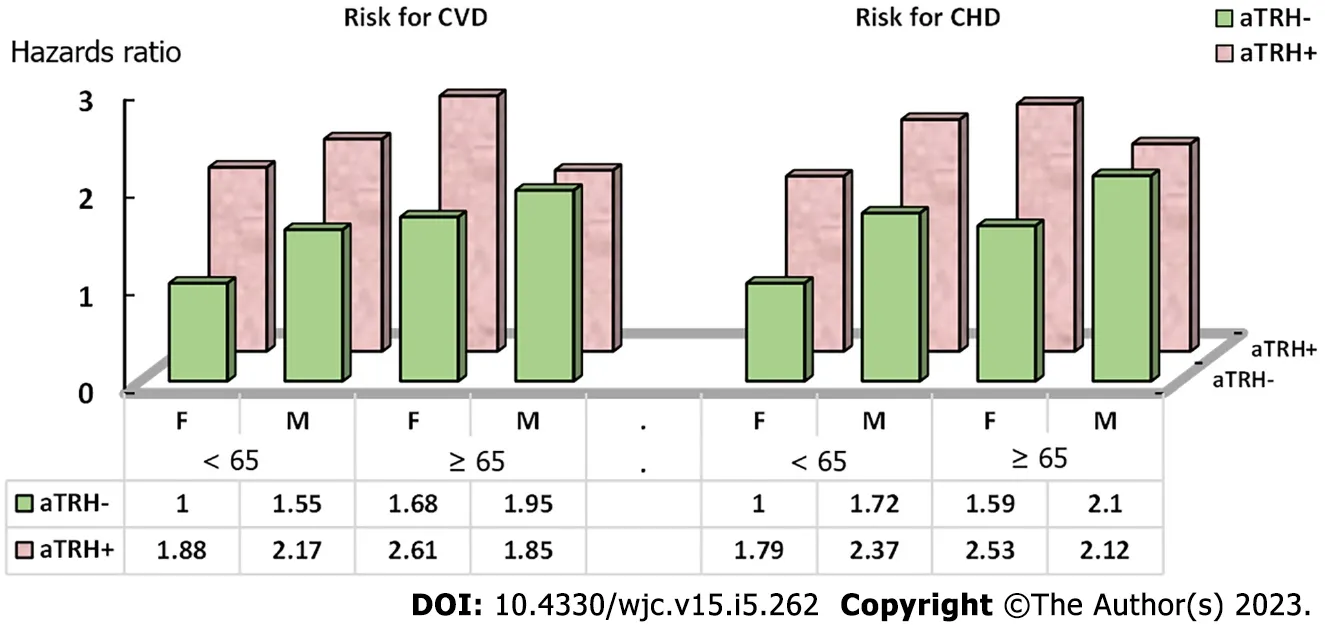
Figure 1 Joint effects of sex and age on the risk of cardiovascular disease and coronary heart disease by apparent treatment resistant hypertension status.
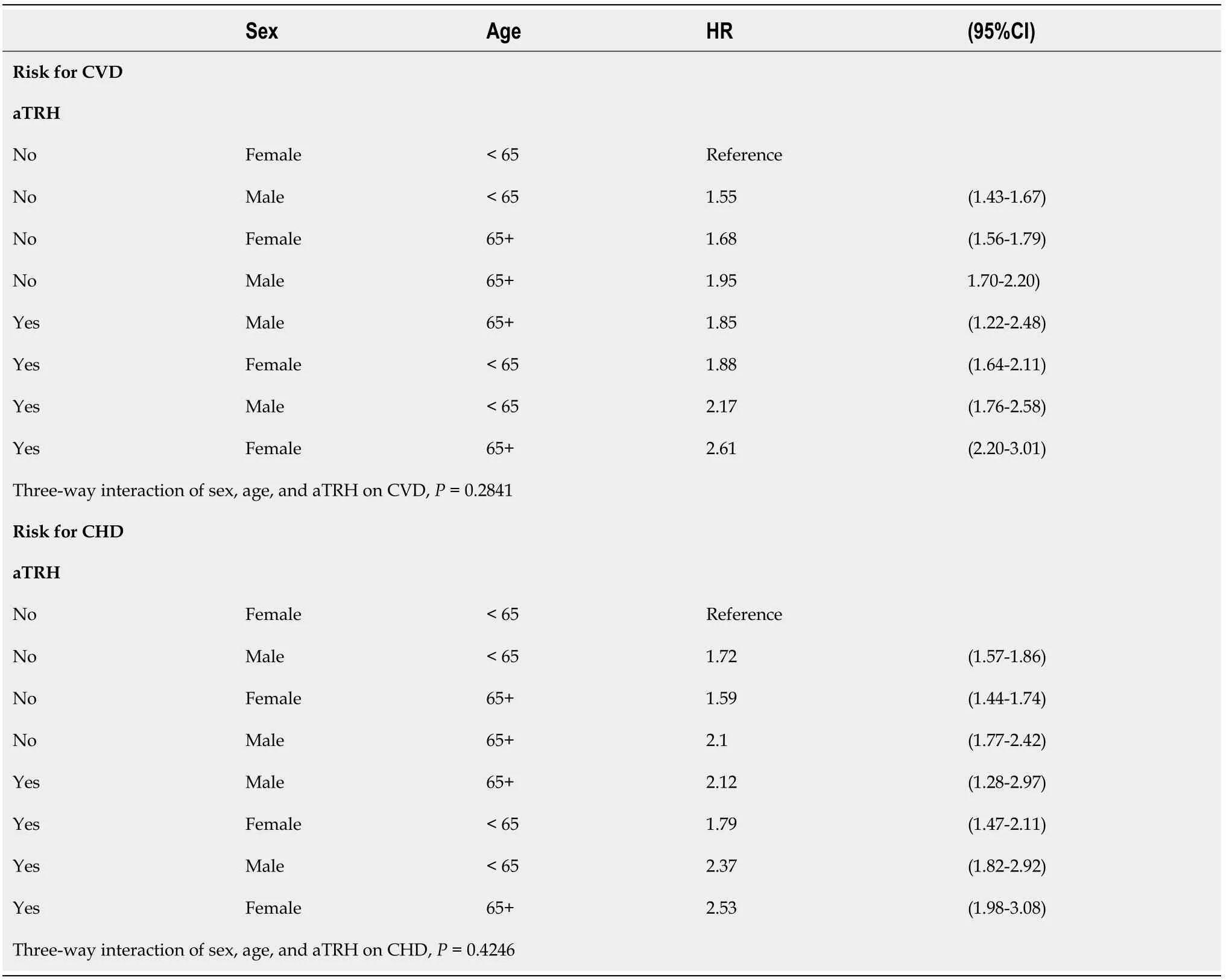
Table 4 Joint impact of age,sex,and apparent treatment resistant hypertension on cardiovascular disease and coronary heart disease risk
DISCUSSION
The overall findings of the present study indicate that there is a positive association between aTRH and risk of CVD.Based on statistically significant two-way interactions of sex with aTRH,and age with aTRH,heterogeneous strata results,statistically significant RERIs,and differing observed and expected joint effects,this study highlights that the association between aTRH and risk of CVD is modified independently by sex and age on both the additive and multiplicative scales.
Although it appeared there was a potential three-way interaction such that sex may modify the interaction of age and aTRH,and vice versa that age may modify the interaction of sex and aTRH on CVD risk,testing for these three-way interactions were not statistically significant.The results suggest that the interaction of sex and aTRH,or of age and aTRH did not depend on the third factor.This finding adds new insights into the body of the literature,that sex and age independently modify the association between aTRH and CVD.
Treating BP becomes more difficult as a patient ages and is complicated by differing BP goals by age and a possible U-shaped relationship between BP and mortality among the elderly.Among this population also exists the risk of over-correcting and lowering BP too much which can cause other health concerns including dizziness and falls[2,30,31].However,2017 ACC/AHA changes to the guidelines no longer specify a different target BP for those ≥ 60 and the SPRINT study of older Americans indicated better health outcomes among those with more aggressive BP lowering targets (SBP 120vs140 mmHg)[32,33].This area remains a topic of debate with more research needed on this unique population.
Research has shown that older women are more likely to adhere to medications and more likely to have their BP taken regularly,yet they appear to experience higher rates of uncontrolled hypertension[15].Multiple mechanisms are believed to contribute to this increase in hypertension and uncontrolled hypertension in aging women including: Activation of the renin angiotensin system,obesity,activation of sympathetic nervous system,and decline in estrogen levels[15,17,34].Stress on the body due to hypertension is believed to be more severe in women than in men[35].Coupled with gender biases in treatment and management of CVD symptoms and events,we can envision how uncontrolled hypertension and aTRH would lead to more adverse health outcomes in women than men,especially in an aging population[36,37].The pathophysiology of aTRH is believed to be linked to blood volume and salt,and salt-sensitive hypertension increases in women post-menopause thus we would expect aTRH to be more prevalent among post-menopausal women[18,38,39].
Very few studies have examined potential effect modifiers on the relationship between aTRH and CVD.Our findings are consistent with existing research in that aTRH is positively associated with CVD and both sex and age independently can modify the association between aTRH and CVD[3-5,9,10].However,these studies only examined relative measures of association.Our study both confirmed presence of two-way interaction on the multiplicative scale and also identified that this modification is present on the additive scale.Epidemiologists have noted that additive interaction is most important for public health as it indicates an absolute number of cases which would be prevented if the modifier were removed[22,40].
No study to date has examined potential three-way interaction with aTRH.With health effects of sex and age linked it is important to examine how these gender disparities in cardiovascular outcomes of patients with aTRH differ between subgroups of age[11,12].Public health programs aimed at improving awareness of aTRH should make specific effort to target women and informing them of the dangerous health consequences associated.This study suggests that physicians should take special note in their treatment considerations when female patients are experiencing uncontrolled hypertension and understand the serious cardiovascular risks associated with developing aTRH.For example,because the interaction of age and aTRH on CVD did not change by sex,we would still endorse applying these recommendations to vigorously control aTRH in women of all ages instead of focusing on the older group only.
This study has several strengths.ALLHAT provides us with one of the largest datasets to test the impact of aTRH on CVD risk.Sample size is particularly important when analyzing effect modification as it utilizes subgroup analyses.We also deployed two methods (propensity score weighting and multiple imputation) to conserve power in our analyses.Similar findings from our original analysis and both sensitivity analyses indicate our study is adequately powered.Another strength provided by use of ALLHAT is in our classification of aTRH.BP was taken twice from a seated position and averaged for each study visit,medication adherence was maintained through pill counts at each study visit,and doses of antihypertensive medications were appropriately titrated up to the maximum tolerated dose prior to adding on an additional medication.All of these factors allow for accurate ascertainment of aTRH status and reduce the likelihood of false positives due to pseudoresistance[2-5].
While a strong study,there are also several limitations.As this study is limited to its analysis of variables collected in ALLHAT only,additional data could be included in the analysis.For example,dietary salt intake was not measured in ALLHAT,thus we could not adjust for this in multivariate models as it is suggested that aTRH is influenced by blood volume and salt intake[38,39].However,because ALLHAT is a randomized clinical trial,potential unmeasured factors are balanced among the participants.The clinical trial nature of our data source,while a strength for validity of aTRH classification,is also a limitation as subjects were selected based on pre-determined criteria best fit for the goals of ALLHAT and thus further studies are needed to confirm the results among different study populations.The study participants consisted of older adults (≥ 55) and thus findings of the study in women should also be evaluated in women aged 55 and older,instead of interpretating the results to those aged < 55.Additionally,the impact of pseudoresistance can never be completely removed and “white coat” effect is always a possibility when examining BP readings.
aTRH increases the risk of CVD in patients with hypertension and this relationship is modified by age and sex independently on both the relative (multiplicative) and absolute (additive) scales.More research is needed to shed further light on these gender differences,especially with regard to women both pre and post menopause.Future research should focus on these sex and age differences and how it might impact treatment and control of aTRH as there is still much unknown about this specific relationship.Management of aTRH should take a patient’s age and sex into consideration and more preventive interventions should be aimed at aging women as they represent the subgroup of aTRH patients with the highest combined risk of CVD.
CONCLUSION
aTRH was significantly associated with an increased risk of CVD and this association was modified by both sex and age.Further studies are warranted to test these mechanisms.
ARTICLE HIGHLIGHTS
Research background
A Limited number of studies have been conducted to test the magnitudes of the association between apparent treatment resistant hypertension (aTRH) and risk of cardiovascular disease (CVD).
Research motivation
aTRH is significantly associated with the risk of CVD.It is important to understand whether age and sex significantly modify this association.Findings of the study could add new evidence to the body of literature,and provide new insights into further mechanism studies.
Research objectives
To investigate the association between aTRH and risk of CVD and examine whether sex and age modify this association.
Research methods
We applied an observational analysis study design using data from the United States Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).ALLHAT recruited participants(n = 25516) from 625 primary care settings throughout the United States,Canada,Puerto Rico,and United States Virgin Islands,aged 55 and older with hypertension and at least one additional risk factor for heart disease.aTRH was assessed from the year 2 visit.CVD event was defined as one of the following from the year 2 follow-up visit: Fatal or non-fatal myocardial infarction,coronary revascularization,angina,stroke,heart failure,or peripheral artery disease.Cox proportional hazards regression was used to examine the effect of aTRH on CVD risk.Potential modifications of sex and age on this association were examined on the multiplicative scale by interaction term and additive scale by joint effects and relative excess risk for interaction.
Research results
Of the total study participants,5030 experienced a CVD event during a mean of 4.7 years follow-up.aTRH was associated with a 30% increase in risk of CVD compared to non-aTRH [hazards ratio (HR) =1.3].Sex and age modified this relationship on both multiplicative and additive scales independently.Stratified by sex,aTRH was associated with a 64% increase in risk of CVD in women,and a 13% increase in risk of CVD in men.Stratified by age,aTRH had a stronger impact on the risk of CVD in participants aged < 65 than it did in those aged ≥ 65.Significant two-way interactions of sex and aTRH,and age and aTRH on risk of CVD were observed (P < 0.05).The observed joint effect of aTRH and ages ≥ 65 years in males was less than what was expected for both additive and multiplicative models,although three-way interaction of sex,age,and aTRH on the risk of CVD and CHD did not reach a statistical significance (P> 0.05).
Research conclusions
aTRH was significantly associated with an increased risk of CVD and this association was modified by both sex and age.
Research perspectives
Further studies are warranted to test these mechanisms.
FOOTNOTES
Author contributions:Nelson JT and Liu L contributed to the design and analysis of the study; Nelson JT prepared the written manuscript; Liu L critically reviewed and edited the manuscript.
Institutional review board statement: This study,using de-identified data from the National Heart,Lung,and Blood Institute,has been approved by Drexel University Institutional Review Board,No.1608004781 (Principal Investigator: Longjian Liu).
Informed consent statement:This ALLHAT data is de-identified and publicly available for investigators to obtain through an IRB application process.Signed Informed Consent Forms are unavailable for the investigators conducting a secondary data analysis project.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:The manuscript was prepared using ALLHAT Research Materials obtained from the National Heart,Lung,and Blood Institute (NHLBI).We are not allowed to share this dataset.For those who are interested in using this dataset,they need to apply for it from the NHLBI directly.
STROBE statement:The authors have read the STROBE Statement—checklist of items,and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Julianne Theresa Nelson 0000-0003-0817-5545; Longjian Liu 0000-0001-7956-7111.
S-Editor:Fan JR
L-Editor:A
P-Editor:Yu HG
 World Journal of Cardiology2023年5期
World Journal of Cardiology2023年5期
- World Journal of Cardiology的其它文章
- Acute heart failure as an adverse event of tumor necrosis factor inhibitor therapy in inflammatory bowel disease: A review of the literature
- Atrial fibrillation and coronary artery disease: An integrative review focusing on therapeutic implications of this relationship
- Current knowledge and contemporary management of non-A non-B aortic dissections
- Importance of concomitant functional mitral regurgitation on survival in severe aortic stenosis patients undergoing aortic valve replacement
- Impact of erythropoietin therapy on cardiorenal syndrome: A systematic review with meta-analysis
- Extracorporeal veno-venous ultrafiltration in congestive heart failure: What’s the state of the art? A mini-review
