Feasibility and clinical benefits of the double-ProGlide technique for hemostasis after cryoballoon atrial fibrillation ablation with uninterrupted oral anticoagulants
Jia-Yin SUN, Chang-Bo XUAN, Hai-Liang YU, Hai-Yang WANG, Hong-Ya HAN, Zhi-Ming ZHOU, De-An JIA, Dong-Mei SHI, Yu-Jie ZHOU, Shi-Wei YANG,✉
1.Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart Lung and Blood Vessel Disease, the Key Laboratory of Remodeling-Related Cardiovascular Disease, Ministry of Education, Beijing, China; 2.Department of Cardiology, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China; 3.Department of Cardiology, Tangshan Fengrun District Second People’s Hospital, Hebei, China; 4.Department of Cardiology, Qingdao Municipal Hospital, Qingdao, China
✉ Correspondence to: yang.shiwei@ccmu.edu.cn https://doi.org/10.26599/1671-5411.2023.04.004
ABSTRACT OBJECTIVE To access the efficacy and safety of the double-ProGlide technique for the femoral vein access-site closure in cryoballoon ablation with uninterrupted oral anticoagulants (OAC), and its impact on the electrophysiology laboratory time as well as hospital stay after the procedure in this observational study.
Cryoballoon ablation has emerged as an important therapeutic option for patients with symptomatic, drug resistant atrial fibrillation(AF).[1]Due to the adequate use of oral anticoagulants(OAC) for thrombosis prevention during periprocedural period, as well as the use of large-caliber percutaneous sheaths up to 15-French (Fr) for device placement through femoral venous access-site, patients with AF undergoing cryoballoon ablation are at a higher risk of groin and vascular complications, including bleeding, hematoma, pseudoaneurysm and arteriovenous fistula.[2,3]Moreover, manual compression and prolonged compression bandage (usually ≥ 12 h) are commonly applied for hemostasis, which may lead to patient discomfort and increase the potential risk of deep vein thrombosis.[4]In addition, the time required for hemostasis and bed rest after cryoballoon ablation significantly affects the total electrophysiology (EP) laboratory time and patients’hospital stay after the procedure.
A variety of closure devices have been investigated to achieve rapid hemostasis for arterial access-sites and reduce complications,[5-7]which may allow patients to ambulate earlier and discharge sooner.However, there is few closure systems especially for venous access-sites.Some studies have indicated that the ProGlide, a suturemediated device (Abbott Vascular Devices, Santa Clara,CA, USA) could be applied for closure of femoral venous access requiring large venous sheaths,[8,9]and at least two devices are required for larger sheath sizes more than 8 Fr according to the manufacturer’s manual.However, the data about a double ProGlide-assisted closure technique in AF patients with uninterrupted OAC during cryoballoon ablation is limited.In this study, we analyzed the feasibility and clinical benefits of the double-ProGlide strategy on uninterrupted OAC for venous hemostasis, as compared to the manual compression, in AF patients after cryoballoon ablation.
METHODS
Study Population
A total of 140 patients, who underwent pulmonary vein isolation using cryoballoon technique from May 2019 to May 2021, were considered to be outside the initial learning curve and enrolled in this study.Among these participants, 70 consecutive patients between May 2019 and September 2020 received manual compression for closure of the femoral venous site.The next 70 consecutive patients between October 2020 and May 2021 used double-ProGlide technique for femoral venous site hemostasis.This study was approved by the Institutional Ethics Committee of Beijing Anzhen Hospital (No.2023 048X), Capital Medical University, Beijing, China and all patients signed informed consent.
Ablation Procedure
The cryoballoon ablation procedures were performed as previously reported.[10]Under deep conscious sedation, venous puncture was applied using the Seldinger technique.Two 6 Fr access sheaths and one 8 Fr transeptal sheath were inserted into the left and right femoral vein, respectively.The former sheaths were used to introduce a multielectrode coronary sinus catheter and a right ventricular catheter.And the latter sheath was used for gaining a single transseptal access.Heparin was administered to achieve an activated clotting time > 300 s.After that, the 8 Fr sheath was removed and replaced by the 15 Fr sheath, through which a 28-mm second-generation cryoballoon (Arctic Front Advance, Model# 2AF-283, Medtronic, Mounds View, MN, USA) was placed into the left atrium, then inflated and positioned at each pulmonary vein ostium for cryoenergy applications (180 s).
The function of phrenic nerve was monitored by diaphragmatic stimulation.Heparin was not routinely antagonised after the procedure.Warfarin or novel OAC were uninterrupted for the ablation procedure, so were the antiplatelet agents (acetylsalicylic acid or clopidogrel).
Hemostasis After the Cryoballoon Ablation
For patients in manual compression group, manually pressure was applied at puncture sites until bleeding stopped, then a compression bandage was used for at least 12 h and removed in case of no groin complications.For patients in ProGlide group, two ProGlide devices were used post-insertion of the 15 Fr sheath since pre-insertion might interfere with subsequent procedures.According to the manufacturer’s instructions, one ProGlide suture system was rotated about 30° to one side and another one was rotated to the other side (Figure 1).After that, a light compression bandage was used for no more than 8 h.
Endpoints
The primary endpoints of the study were the vascular and groin complications, the total time in the EP laboratory and the hospital stay length after the ablation procedure.Moreover, the time from completion of the procedure until femoral vein hemostasis and bed rest time were also obtained from all participants and compared between two groups.The occurrence of vascular and groin complications, including haematomas, retroperitoneal bleed, re-bleeding access-site, pseudoaneurysm, arteriovenous fistula, infection and thrombosis were accessed by clinical examination and color duplex sonography the day after the procedure and during three-month follow-up.Major vascular complications were defined as surgical repair of vascular injury, groin-related transfusion or infection and ultrasound-guided compression.[8]

Figure 1 Closure of femoral vein access-site with the Perclose ProGlide® device in the course of cryoballoon atrial fibrillation ablation with uninterrupted oral anticoagulants.(A): The Perclose ProGlide device is inserted through the wire; (B): intraluminal positioning is confirmed by slow blood flow out of the side port; (C): the surgical knot is pushed against the venous wall using a knot pusher for haemostasis; and (D): the groin site is free of any bleeding once the knot has been deployed.
Statistical Analysis
Statistical analysis was conducted by SPSS 22.0 (SPSS Inc., IBM, Chicago, IL, USA).Continuous variables were expressed as mean ± SD or medians (interquartile range), and comparison between two groups were performed by the independent samplest-test or the Mann-WhitneyUtest.Categorical variables were presented as counts (percentages), and the Pearson’s chi-squared test or the Fisher’s exact probability test determined differences between the two groups.Values ofP-value < 0.05 in a two-sided test were considered statistically significant for all tests.
RESULTS
A total of 140 patients (69.30% of male, mean age: 59.21± 10.29 years) were enrolled in this study.Baseline characteristics of patients are outlined in Table 1.The proportion of HAS-BLED score ≥ 3, which predicted high risk of bleeding after anticoagulant therapy in response to AF,was similar in the ProGlide group and the manual compression group (12.86%vs.10.00%,P= 0.791).Other parameters possibly affecting the efficacy of venous accesssite closure, such as body mass index, international normalized ratio, use of antiplatelet agents, hemodialysis, estimated glomerular filtration rate, prior ipsilateral groin operation as well as the values of prothrombin time, activated partial thromboplastin time and platelet, did not show any significant differences between the ProGlide group and the manual compression group.Only AF years showed a significant difference between the ProGlide group and the manual compression group [1.00 (0.32-3.25) yearsvs.3.00 (1.00-7.00) years,P= 0.026], but was considered of no clinical relevance (Table 1).
Compared with the manual compression group, the ProGlide group was associated with significantly shorter total time in the EP laboratory [112.0 (93.3-128.8) minvs.123.5 (107.3-158.3) min,P= 0.006], time from sheath removal until venous site hemostasis [3.8 (3.4-4.2) minvs.8.0 (7.6-8.5) min,P< 0.001], bed rest time [8.0 (7.6-8.0)hvs.14.1 (12.0-17.6) h,P< 0.001] and hospital stay after the cryoballoon ablation procedure [13.8 (12.5-17.8)hvs.38.0 (21.5-41.0) h,P< 0.001] (Table 2).
Immediate hemostasis was achieved in all the patients who received double-ProGlide technique for venous access-site closure.Re-bleeding at the access-site occurred in two patients of the ProGlide group and in five patients of the manual compression group during hospitalization (2.86%vs.7.14%,P= 0.441), which required additional manual compression.Haematomas ≥ 5 cm, pseudoaneurysm as well as arteriovenous fistula occurred in the same patient of the manual compression group, who required surgical repair but no transfusion, while the complications mentioned above did not occur in the Pro-Glide group (1.43%vs.0,P= 1.000).The rate of blood vessel vagus reflex did not show any obvious differences between the ProGlide group and the manual compression group (0vs.1.43%,P= 1.000).However, the occurrence of dysuria was much higher in the manual compression group, as compared to the ProGlide group (7.14%vs.1.43%,P= 0.209).Moreover, retroperitoneal bleed, access-site infection or thrombosis was not detected in either group.At three-month follow-up, one patient of the manual compression group was diagnosed with pseudoaneurysm and arteriovenous fistula.For this patient, conservative compression was applied and no additional intervention was required (Table 3).
DISCUSSION
In this study that included AF patients undergoing cryoballoon ablation using a large 15 Fr sheath, the double-ProGlide technique was demonstrated to be safe and effective for femoral access-site hemostasis.The success rate of the double-ProGlide strategy was 100% among the patients with uninterrupted use of anticoagulants, and none of the patients had major vascular complications with this closure strategy.Moreover, patientstreated with the double-ProGlide technique experienced nearly 53% reduction in the hemostasis time, 9% reduction in the total EP laboratory time, 43% reduction in the bed rest time, and 64% reduction in the hospital stay after the procedure.

Table 1 Baseline characteristics of the study population.
In the course of transfemoral interventions, the most common cause of morbidity is groin complications, which continue to occur in 1% of cases with the use of closure devices.[11]Although the risk of vascular complications is lower in venous access than in arterial access,with the development of cardiac interventions requiring large-caliber venous sheaths, especially in patients using OAC or antiplatelet agents, the incidence of vascular complications related to the femoral venous access has increased.Therefore, effective hemostasis becomes particularly important.Manual compression, representing as the standard technique for hemostasis, can lead to more vascular complications, prolonged EP laboratory time and delay time to mobilization and discharge.[8,12]On the other hand, the Perclose ProGlide Suture-Mediate Closure System (Abbott Vascular, Lake Bluff, IL, USA), due to the high success rates and the low rates of complications, is used as a safe and effective alternative in many procedures requiring large bore vascular access closure.[13-15]Moreover, as approved by the United States Food and Drug Administration, ProGlide has also been utilized for hemostasis of percutaneous vein access using large-sized sheaths,[16]but the related studies are limited and most of them are performed with a different anticoagulation regimen and with no analysis of the total EP laboratory time and the length of hospital stay after the procedure.[8,9,17-19]

Table 2 Comparison of hemostasis time, bed rest time, total laboratory time and hospital stay after the procedure between ProGlide group and manual compression group.
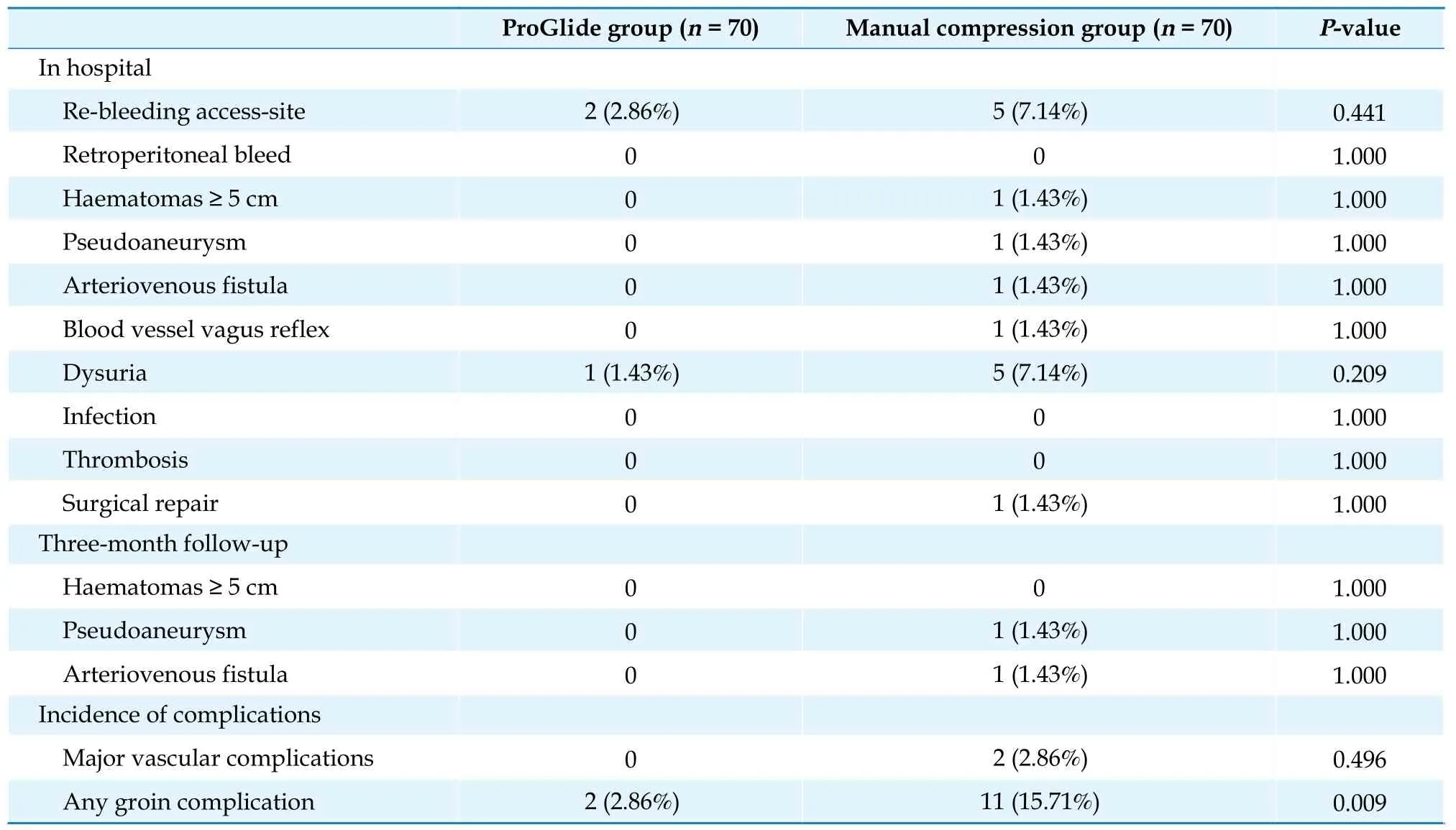
Table 3 Postprocedural complications in hospital and at three-month follow-up.
In a prospective analysis of retrospective data from the EVEREST II/REALISM MitraClip study subjects with large-caliber sheaths (24 Fr) application, ProGlide was identified to be a safe strategy showing a very high rate of freedom from major femoral vein access-site related complications at 30 days (98.1%) post procedure, which met the predefined acceptance safety criterion.[20]In the study of Geis,et al.,[8]ProGlide closure showed immediate femoral vein access hemostasis in 92.5% of patients with MitraClip implantation.Major complications were observed in only one patient (2.5%).Hamid,et al.[21]demonstrated the feasibility and safety of venous access-site closure using the ProGlide devices in patients undergoing percutaneous catheter intervention with mean sheath diameter 11.5 ± 3 Fr.Complete hemostasis was achieved in 98%of subjects and no major complications occurred.In our study, successful femoral vein access closure by the Pro-Glide devices were achieved in all the patients, which may due to the proper puncture access and correct execution of knot stability steps conducted by the skill hands.Furthermore, no major complications occurred in the ProGlide group, and patients using ProGlide devices had a lower rate of groin complication (2.86%), which was comparable to femoral vein access-site related complication rates reported in other studies.However, the anticoagulant therapy was not interrupted during cryoballoon ablation in this study.
In previous studies with application of large-bore sheaths, patients on direct OAC always received their last dose 12-24 h before the procedure and restarted the therapy 4-6 h postprocedural.[22,23]Yet, in order to avoid thromboembolic complications, minimizing time without anticoagulation is clearly recommended.[24-26]Some reports have indicated that an uninterrupted OAC strategy during cryoballoon AF ablation is effective and safe.[27,28]While a recent study concerning on the combination of cryoballoon ablation and uninterrupted OAC showed an increased incidence of the femoral access-site complications in patients using the figure to eight suture technique for hemostasis followed by a 4 h bed rest.[29]In the current study, we used the double-ProGlid technique and prolonged bed rest time (8 h), which may contribute to the better outcomes.
Since the number of AF patients requiring catheter ablation has gradually increased, techniques which could reduce the total EP laboratory time and the length of hospital stay after the procedure become extremely important.Cryoballoon ablation, compared with the pointby-point radiofrequency catheter ablation, could significantly reduce the procedure time.[2]However, hemostasis after sheath removal in the EP laboratory could be time-consuming and have negative effect on the hospital stay after the procedure.A recent study showed hemostasis with the ProGlide device at the venous vascular sites was associated with a significant reduction in the overall duration of stay on an intensive care unit.[8]In our study, the double-ProGlide technique was demonstrated to reduce the EP laboratory time without increasing complication rates, then shorten the bed rest time as well as hospital stay after the procedure, which may improve the clinical efficiency.
In addition, since the vascular closure devices are expensive, the figure of eight suture, performing as a more economical approach, was widely used for groin access closure.Some studies indicated that hemostasis obtained with a figure of eight suture was associated with a significant shorter EP laboratory time and flat-time-inbed compared to manual pressure in AF patients receiving continuous therapeutic warfarin or interrupted novel OAC.[12,23,30]In the past half year, we have also evaluated the figure of eight suture for venous access closure.We found that for large-bore venous access closure, the figure of eight suture resulted in a shortened time to achieve hemostasis along with a lower overall risk of access site complications compared to manual pressure.We will summarize these data as soon as possible in order to find a better and more economical solution to reduce the groin complications and improve EP laboratory workflow.
LIMITATIONS
Our study has a few limitations.Firstly, this was a retrospective, non-randomized, single-center study, and the number of patients enrolled was small.Secondly, since the double-ProGlide technique as well as the manual compression were applied in non-overlapping time periods in the study, a further advance in the operator learning curve may affect the results.Last but not least, the costs of the ProGlide devices, which may exert negative effect on the total hospital costs, were not analyzed in the study.Therefore, further randomized and blinded studies are needed to draw a positive conclusion.
CONCLUSIONS
Utilization of the double-ProGlide technique for hemostasis after cryoballoon ablation with uninterrupted OAC is feasible and safe, which has the clinical benefit in reducing the total EP laboratory time and the hospital stay length after the procedure.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No.81100143), the Beijing Nova Program (Z121107002512053), the Beijing Health System High Level Health Technology Talent Cultivation Plan (No.2013-3-013), the Beijing Outstanding Talent Training Program (No.2014000021223ZK32), the Beijing National Science Foundation (No.7212100), the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX20 1303), and the National Key Clinical Speciality Construction Project.All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2023年4期
Journal of Geriatric Cardiology2023年4期
- Journal of Geriatric Cardiology的其它文章
- Tricuspid valve avulsion
- A rare cause of pulmonary hypertension in an elderly woman
- How to effectively manage the refractory coronary thrombus? A systemic mini-review
- Safety of butylphthalide and edaravone in patients with ischemic stroke: a multicenter real-world study
- Prevalence and incidence of heart failure among community in China during a three-year follow-up
- Minimally invasive valve surgery: pushing boundaries over the eighty
