A rare cause of pulmonary hypertension in an elderly woman
Shing Ching, Chiu Sun Yue
Division of Cardiology, Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong, China
✉ Correspondence to: csa698@ha.org.hk https://doi.org/10.26599/1671-5411.2023.04.007
Diastolic dysfunction is a common substrate of pulmonary hypertension (PH) in the elderly.A minority of them, however, has another etiology of PH with diastolic dysfunction as a confounder,the alarming echocardiographic features of which are important to recognize.For example, dilated coronary sinus is unusual, as is significantly dilated right atrium,right ventricle or pulmonary artery.We report a rare case of PH in an elderly woman caused by an unrecognized partial anomalous pulmonary venous return (PAPVR)of the left and right pulmonary veins into the coronary sinus with intact atrial septum, which to our knowledge has not been reported in the literature.
A 62-year-old woman of unremarkable past health presented with insidious onset of ankle edema, exertional dyspnea and chest pressure.A soft ejection systolic murmur was heard on the left upper sternal border.Electrocardiogram showed sinus rhythm, right axis deviation and right ventricular hypertrophy.Chest radiography found dilated pulmonary arteries and cardiomegaly.Echocardiography confirmed moderate right ventricular, as well as severe biatrial enlargement (Figure 1A).The estimated right ventricular systolic pressure was 40 mmHg.Notably, the coronary sinus was dilated(Figure 1B).Transesophageal echocardiogram (TEE) did not find any septal defects.Cardiac catheterization was performed to evaluate the severity and the etiology of PH, the result of which is shown in Table 1.Pulmonary wedge was technically challenging and not obtained.Oxygen saturation in the left ventricle was used as surrogate of that of pulmonary vein.The Qp:Qs ratio was 1.9:1.Oxygen step-up was noted at the right ventricular level indicating left to right shunt at the atrial level.Interestingly, coronary angiogram, done to evaluate possible concomitant coronary artery disease, showed, in addition,coronary fistulas draining from left anterior descending and right coronary arteries to the pulmonary artery (Figure 2A & 2B).Computed tomography (CT) of the chest was performed to define the anatomy of shunt, revealing partial anomalous venous drainage into the coronary sinus (Figure 3A-3D).Specifically, not only the left upper and lower veins, but also a vein from the posterior segments of the right upper lobe, connect to the coronary sinus, accounting for the echocardiographic and hemodynamic findings.The pulmonary artery was grossly dilated, as was the right atrium and right ventricle.The patient declined surgical correction.In the ensuing 14 years of follow-up, the patient developed dementia and moved to a long-term care facility.Aside from four admissions for edema and pulmonary congestion, she had New York Heart Association class 2 symptom without evolving into Eisenmenger physiology.The latest echocardiography showed dilated right ventricle with normal systolic function and mild PH similar to her initial study.
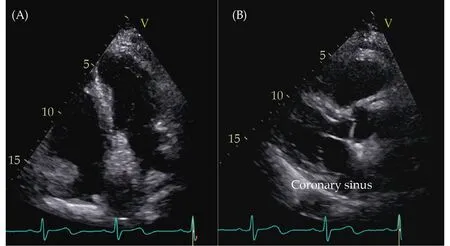
Figure 1 Four chamber view shows moderate right ventricular and severe biatrial enlargement (A) and parasternal long axis view shows dilated coronary sinus (B).
Echocardiography is often the first modality to evaluate patients with suspected PH.Coronary sinus dilation is an important finding not to be dismissed.In the absence of significant tricuspid regurgitation or elevated right atrial pressure, it signals abnormal blood flow into the coronary sinus, such as in persistent left superior vena ca-va, unroofed coronary sinus, or PAPVR.Isolated atrial septal defect is an unlikely cause unless it is large and long-standing.Agitated saline injection via the left arm would preferentially opacify the coronary sinus before other right-sided chambers in the setting of persistent left superior vena cava, but not in other conditions.Persistent left superior vena cava is a benign condition and does not explain shunting or right heart dilation.The concurrence of coronary sinus and right heart dilation raises the suspicion of unroofed coronary sinus or PAPVR, which goes in line with oxygen step-up at the right ventricle.The incidental finding of coronary to pulmonary artery fistula is a red herring in this circumstance and does not account for the left to right shunt, since there is no oxygen step-up from the right ventricle to the left pulmonary artery.Furthermore, coronary fistulas of hemodynamic significance are physiologically akin to patent ductus arteriosus causing, besides angina from coronary steal, predominantly left heart and pulmonary artery, but not right ventricular dilation.CT is the modality of choice
to define the location and course of the shunt.It is important to trace all pulmonary veins to their origins as many variants of PAPVR exist, the commoner of which is a connection of the right upper pulmonary vein to the superior vena cava often associated with a sinus venosus defect.More than 70% of PAPVR patients have coexisting atrial septal defect.Drainage into the coronary sinus is a rare form of PAPVR accounting for only 3% of cases in a series.[1]The left pulmonary veins may connect to the coronary sinus, or drain via a vertical vein into the brachiocephalic vein.In our patient, interestingly, while the left upper and lower veins drain into the coronary sinus, the right upper lobe has two separate drainage veins, one from the anterior segments into the left atrium while the other vein from the posterior segments crossing the midline into the coronary sinus (Figure 3C & 3D).Importantly, no other venous anomaly or atrial septal defect exists.This pattern of drainage is very unusual and has not been reported before.Although TEE is used to diagnose PAPVR in some cases,[2]the anomalous right upper pulmonary vein is sandwiched between the right pulmonary artery and the right main bronchus obscuring any ultrasound emitting from the esophagus (Figure 3E) and may therefore be missed on TEE.Cross-sectional imaging such as CT is preferred to fully delineate the shunt anatomy.

Table 1 Hemodynamic data of cardiac catheterization.

Figure 2 Coronary fistulas draining from left anterior descending (A) and right coronary arteries (B) into the pulmonary artery.

Figure 3 Contrast computed tomography thorax shows the left upper (A), left lower (B) and a vein from the posterior segments of the right upper lobe (C) connecting to the coronary sinus, (D) the anterior segments of the right upper lobe is drained by another vein into the left atrium, and (E) multiplanar reconstruction image of the anomalous right upper vein shows it courses between the right pulmonary artery and the right main bronchus, which obscures any ultrasound emitting from the esophagus on transesophageal echocardiogram.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2023年4期
Journal of Geriatric Cardiology2023年4期
- Journal of Geriatric Cardiology的其它文章
- Tricuspid valve avulsion
- How to effectively manage the refractory coronary thrombus? A systemic mini-review
- Safety of butylphthalide and edaravone in patients with ischemic stroke: a multicenter real-world study
- Prevalence and incidence of heart failure among community in China during a three-year follow-up
- Minimally invasive valve surgery: pushing boundaries over the eighty
- Feasibility and clinical benefits of the double-ProGlide technique for hemostasis after cryoballoon atrial fibrillation ablation with uninterrupted oral anticoagulants
