A case of Posner-Schlossman syndrome treated by gonioscopy-assisted transluminal trabeculotomy
Xiao Tang, Jia-Jian Wu, Xue-Ning Ding, Hong-Jin He, Xiao-Qun Zhou, Yu He, Lin Jing,Liu-Zhi Zeng
1Eye School of Chengdu University of TCM, Chengdu 610075, Sichuan Province, China
2Chengdu First People’s Hospital, Chengdu 610095, Sichuan Province, China
Dear Editor,
We present the reported case of Posner-Schlossman syndrome (PSS) treated by gonioscopy-assisted transluminal trabeculotomy (GATT).A 28-year-old male presented recurrent PSS in his left eye, leading to uncontrolled intraocular pressure (IOP) and thus glaucomatous optic neuropathy.Two years ago, the patient suddenly experienced swelling with impaired vision in his left eye with no obvious cause, and was diagnosed with the PSS in left eye in another hospital.The patient had IOP of 30 to 40 mm Hg at attack every 3 to 5mo, and was given tobramycin and dexamethasone eye drop and brinzolamide eye drop.After the treatment,the patient’s condition was alleviated.Two months later, the patient had swelling again in his left eye and IOP of 38 mm Hg,and was locally given tobramycin and dexamethasone eye drop, brinzolamide eye drop, and timolol maleate eye drop as well as mannitol intravenous drip.But his symptoms were not alleviated.After half a month, the patient had a measured IOP of 35 mm Hg in his left eye in our outpatient clinic and was additionally given methazolamide tablets.After the treatment,the patient’s symptoms were not relieved and still had an IOP higher than 30 mm Hg.Therefore, he was admitted to our hospital.The patient suffered repeated attacks of the above symptoms, which were slightly relieved after the medication,with the ⅠOP of the left eye fluctuating between 25 and 38 mm Hg.
Ethical ApprovalThis case report was approved by the Medical Ethic Review Committee of Chengdu Integrated TCM & Western Medicine Hospital (YJS No.012, 2023).The study was conducted in accordance with the principles of the Declaration of Helsinki.The informed consent was obtained from the subjects.
Examination on admission: visual acuity 0.3, and corrected visual acuity 1.0 (-1.00 DS) for the right eye, visual acuity 0.4, and corrected visual acuity 1.0 (-1.00 DS) for the left eye;IOP: 15 mm Hg in the right eye and 38 mm Hg in the left eye; left eye: clear cornea, posterior-inferior corneal muttonfat keratic precipitates (KP), normal anterior chamber depth,aqueous flare (AF) positive, round pupil with a diameter of about 3 mm and sensitive to light reflection, and clear lens.Right eye: clear cornea, normal anterior chamber depth, round pupil with a diameter of about 3 mm and sensitive to light reflection, and clear lens.Fundus: right eye cup to disc ratio(C/D)=0.5, and left eye C/D=0.5.Ultrasound biomicroscopy(UBM): right eye 3.27 mm, and left eye 3.22 mm in anterior chamber deepth.Spaeth classification of chamber angle: both eyes D40f1+ptm.Central corneal thickness (CCT): both eyes 516 μm.Axial length: right eye 23.97 mm, and left eye 23.90 mm.Ⅴisual field: paracentral scotoma in the left eye,and no obvious anomaly in the right eye (right eye MD: -0.92,and left eye MD: -2.74).Neither of the eyes showed abnormal OCT result in their optic disc or macular region.The 24-hour IOP monitoring: right eye 18 mm Hg (06:00) to 13 mm Hg(12:00), and left eye 38 mm Hg (08:00) to 25 mm Hg (22:00).Admission diagnosis: 1) PSS in the left eye, and 2) binocular ametropia.
Since the IOP of the left eye was difficult to control by conservative treatment, the patient underwent GATT in the left eye under local anesthesia.Intraoperatively, an infratemporal and supranasal clear corneal limbal auxiliary incision was made by a 15° scalpel, and a supratemporal clear corneal limbal main incision was made by a 1.8 mm scalpel.The 0.2 mL aqueous humor was sampled for cytomegalovirus and herpes simplex virus (HSⅤ) ⅠgG and PCR detection.The viscoelastic was injected into the anterior chamber after myosis.The position of the trabecular meshwork was observed under the gonioscope.Under the gonioscopy-assisted direct vision, a Zeng’s trabeculotome (Figure 1) was used to incise the trabeculae and the inner wall of the Schlemm canal by about 2 mm at the 7:30 position.An iTrack optical fiber was delivered to the anterior chamber through the supranasal auxiliary incision, and a pair of intraocular forceps was used to clamp the distal end of the optical fiber, insert it into the Schlemm canal from one cut end of the trabecular incision, and advance it anticlockwise.When the optical fiber was advanced to the 1 o’clock position, it was circled two turns, and the viscoelastic was injected.After 360 degrees advancement,the distal end of the optical fiber was seen out of the other cut end of the trabecular incision, and was clamped and pulled outwards to the anterior chamber.The optical fiber was pulled at the other end to perform 360° trabeculotomy and incision of the inner wall of the Schlemm canal (Figure 1).The uniform blood return was seen.The balanced salt solution was used to flush out the returned blood from the anterior chamber, and the balanced salt solution was injected to increase the IOP for 6 to 8 times.Positive episcleral venous fluid wave was seen in the nasal and subnasal regions.Postoperatively, the patient was administered prednisolone acetate eye drop, levofloxacin eye drop, diclofenac sodium eye drop, and sodium hyaluronate eye drop 4 times per day as well as ganciclovir ophthalmic gel 3 times per day in the left eye.
On day 1 postoperatively, the patient’s left eye showed a visual acuity hand motion (HM)/30 cm, IOP 13 mm Hg,mild conjunctival congestion, mild corneal edema, blood cell attachment on the posterior corneal surface, posterior corneal pulverulent KP (++), acceptable anterior chamber depth, anterior chamber filled with hemic aqueous humor,with a few blood clots in the inferior anterior chamber and white filamentous exudation in the anterior chamber, AF(+; Figure 2A).On day 3 postoperatively, the patient’s left eye showed a visual acuity counting finger (CF)/30 cm, IOP 15 mm Hg, mild conjunctival congestion, clear cornea, a few blood cell attachment on the posterior corneal surface,posterior corneal pulverulent KP (+), anterior chamber depth is nomal, somewhat absorption of blood clots in the inferior anterior chamber, complete absorption of white filamentous exudation in the anterior chamber, and AF (+; Figure 2B).At 1mo postoperatively, the left eye showed a visual acuity 1.0,IOP 12 mm Hg, 3 central corneal KP, a few needle-tip-like KP,AF (+), no hyphema, and slight posterior capsule opacification.The ocular hypotensive agent and prednisolone acetate eye drop were withdrawn, and the diclofenac sodium eye drop and ganciclovir ophthalmic gel were still administered to the left eye 3 times per day.Aqueous humor test results showed herpes simple virus (HSⅤ), cytomegalovirus and rotavirus antibodies positive.
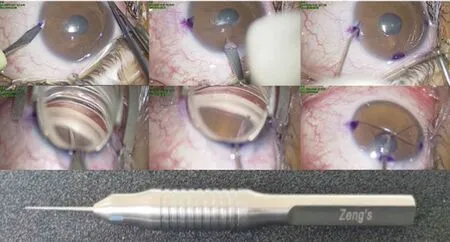
Figure 1 The patient’s intraoperative photography and Zeng’s trabeculotome.

Figure 2 Postoperative eye image of the patient A: The patient’s eye image on day 1 postop.; B: The patient’s eye image on day 3 postop.
At 6mo postoperatively, the patient’s left eye showed a visual acuity 1.0, IOP 12 mm Hg, clear cornea, and KP (-).Gonioscopy: Spaeth classification of chamber angle: right eye D40f1+ptm, left eye C30f0+ptm, patent trabecular incision,and blood return observed at the anterior chamber angle.The administration of diclofenac sodium eye drop and ganciclovir ophthalmic gel in the left eye 3 times per day continued.The prednisolone acetate eye drop was not used.
At 1y postoperatively, the patient’s left eye showed an uncorrected visual acuity 1.0, IOP 14 mm Hg, complete absorption of blood return, KP (-), andC/D=0.5.The left eye was regularly administered diclofenac sodium eye drop,levofloxacin eye drop, and ganciclovir ophthalmic gel 3 times per day.In this paper, GATT was used to make a 360 degrees incision into the inner wall of the Schlemm canal and the trabecular meshwork to reduce the resistance against the outflow of the aqueous humor at the inner wall of the Schlemm canal and the trabecular meshwork to a greater extent, thus lowering the IOP effectively.In this way, the advantage of the internal drainage over the trabeculectomy was preserved while lowering the IOP more powerfully.This case was followed up for 1y postoperatively, during which the IOP was controlled well without using the ocular hypotensive agents,and fluctuated between 12 and 15 mm Hg.The complications such as low IOP, shallow anterior chamber and choroidal detachment were not observed postoperatively either, and no transient IOP rise occurred.Mild hyphema was observed at the early stage postoperatively.When the hyphema occurred at the incised trabeculae and inner wall of the Schlemm canal, it represented the blood reflux of the episcleral vein, which meant that the aqueous humor drainage system behind the Schlemm canal was patent.The patient’s aqueous humor test indicated HSⅤ, cytomegalovirus and rotavirus antibodies were positive,and cytomegalovirus infection was considered to be the most possible cause of PSS.Local use of the ganciclovir eye drops is somewhat useful for controlling the recurrence of PSS and reducing the use of other drugs[1].Currently, ganciclovir is the clinically preferred anti- cytomegalovirus drug and can be administered in many ways, such as by oral administration,topical eye drop or intravitreal injection.It can inhibit the synthesis of the virus DNA and prevent the replication of the herpesvirus[2].Therefore, adding the ganciclovir ophthalmic gel postoperatively may reduce the recurrence of PSS[3].A study have shown a high prevalence of ocular cytomegalovirus infection in patients with PSS.Comparison of cytomegaloviruspositive and cytomegalovirus-negative PSS patients showed that the former had significant loss of corneal endothelial cells and the density was significantly lower than the latter,which may be associated with cytomegalovirus attacking the trabecular meshwork endothelial cells and corneal endothelial cells, resulting in increased IOP and corneal endothelial cell loss.The high possibility of rotavirusopen angle glaucoma (OAG)in cytomegalovirus-positive PSS patients in the future should not be ignored, and regulation of IL-8 and IL-6 levels may be a new intervention to prevent OAG secondary to PSS[4].Murataet al[5]treated 14 cases of PSS with trabeculectomy, and the surgical success (IOP <20 mm Hg) rate was up to 85.7%.In addition, the trabecular ablation and deep sclerectomyetc.have also been used among the PSS patients.Pahlitzschet al[6]performed trabecular ablation for 7 PSS patients with positive cytomegalovirus (cytomegalovirus) results.Postoperatively,their average IOP decreased from 40 to 13 mm Hg, and no patient experienced recurrence during the 12-month observation period.For the affected eyes in the inflammatory state, the deep sclerectomy, a non-penetrating surgery, is considered to have a lower postoperative complication rate.Dupaset al[7]observed 1 patient receiving the deep sclerectomy for up to 7y and found that the patient’s IOP was well controlled with neither complications nor obvious optic nerve injury.As compared with the trabecular ablation, the trabeculectomy has a higher success rate in controlling the IOP.The deep sclerectomy shows a comparable success rate to trabeculectomy, but requires higher patient compliance and more postoperative adjustments[8].A study enrolling 91 PSS patients who underwent filtering surgeries and were followed for at least one year.The conclusion is Ahmed glaucoma valve(AGⅤ) and Ex‐PRESS performed better than trabeculectomy in PSS patients in terms of IOP and success rate.Iris abnormalities might influence the postoperative ⅠOP and this may be valuable in guiding filtration strategies[9].
Considering that the study performed by Tanet al[10]showed that the treatment with selective laser trabeculoplasty (SLT)could significantly lower the IOP of the PSS patients at recurrence, it can be speculated that the effect of lowering the IOP at attack may be achieved after the GATT by eliminating the factors causing the trabecular meshwork dysregulation and reducing the resistance against the outflow of the aqueous humor at the trabecular meshwork to increase the discharge of the aqueous humor.In addition, after GATT, the excretion of the inflammatory mediators such as prostaglandin in the aqueous humor at attack is increased to reduce the effect of the prostaglandin on increasing the production of the aqueous humor and the impact of other inflammatory mediators on the coefficient of aqueous outflow facility, so that the IOP is easier to control upon attack[3].Currently, this case is still being followed up, and more studies are required to demonstrate above speculation.In conclusion, the treatment outcome of this case shows that GATT played a role in significantly lowering the IOP when used to treat this patient with PSS.Though the surgeries cannot prevent the attack of PSS, they can lower the peak IOP at attack, slow down the visual field progress, and possibly reduce the frequency of postoperative recurrence.However, more researches are still needed to support this.
ACKNOWLEDGEMENTS
The authors thank the patient who generously agreed to participate in this report.
Authors’contributions:Tang X: Patient interaction, drafting manuscript; Zeng LZ, Tang X, Wu JJ, Ding XN, He HJ, Zhou XQ, He Y, Jing L: Editing the manuscript, including analysis and interpretation of data and drafting and revising the work for intellectual content.All authors read and approved the final manuscript.Zeng LZ: Patient interaction, diagnosis, treatment,modification of manuscript.
Conflicts of Interest:Tang X,None;Wu JJ,None;Ding XN,None;He HJ,None;Zhou XQ,None;He Y,None;Jing L,None;Zeng LZ,None.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Analysis of retinal arteriolar and venular parameters in primary open angle glaucoma
- ldentification and functional analyses of a novel FOXL2 pathogenic variant causing blepharophimosis, ptosis,and epicanthus inversus syndrome
- Protective effects of ferulic acid against ionizing radiation-induced oxidative damage in rat lens through activating Nrf2 signal pathway
- Novel homozygous ADAMTS17 missense variant in Weill-Marchesani syndrome
- Cost analysis of childhood glaucoma surgeries using the US Medicaire allowable costs
- Predicting the prognosis of primary orbital lymphoma by clinical characteristics and imaging features
