Predicting the prognosis of primary orbital lymphoma by clinical characteristics and imaging features
Jian-Bo Zhu, Bin Li, Hong-Mei Zhang, Ning-Li Wang
1Beijing Tongren Eye Center, Beijing Tongren Hospital,Capital Medical University, Beijing Key Laboratory of Ophthalmology and Ⅴisual Science, Beijing 100730, China
2Department of Diagnostic Radiology, Cancer Hospital,Chinese Academy of Medical Sciences, Beijing 100021, China
Abstract
INTRODUCTION
Lymphomas involving orbit include primary and secondary lymphomas, where the former refer to pathologically proven orbital lymphoma that is not accompanied by lymphoma of other sites or with no history of lymphoma before orbit involvement.Primary orbit lymphoma rarely occurs, accounting for approximately 5%-10% of all extranodal lymphomas[1-2].Non-Hodgkin’s lymphoma is the major pathological subtype of primary orbital lymphoma,whose dominant type is B-cell lymphoma[1-4].In recent years, primary orbital lymphoma has gradually increased,especially in people with immunosuppression or immune hyperfunction, and early diagnosis and standard treatments are major factors influencing the outcomes of those patients[3].Nevertheless, accurately diagnosing primary orbital lymphoma in the early stage is challenging due to the absence of typical clinical characteristics.In addition, studies on primary orbital lymphoma are still lacking, so certain treatment methods do not have adequate standardization levels in some institutes,which, in turn, influences the outcomes of these patients.The aim of this retrospective study was to summarize the clinical characteristics, imaging findings, and treatment strategies to explore their associations with the tumor prognosis.
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective study was approved by the Beijing Tongren Hospital Ethic Committee (No.TREC2023-KY019) with a waiver of informed consent.
PatientsPatients with histologically confirmed primary orbital lymphoma, were retrospectively recruited between January 2012 and May 2017 in our institute.The inclusion criteria were as follows: 1) those with histologically confirmed primary orbital lymphoma and those with a definite subtype of lymphoma; 2) those with no concurrent lymphoma at other sites and also without a history of lymphoma; 3) those with complete data of tumor diagnosis and treatment; 4) the data of enhancement computed tomography (CT) and/or magnetic resonance imaging (MRI) scanning before treatment were available.The exclusion criteria were: 1) residual tumor was still showing in imaging examinations after one month of the initial treatment completion; 2) lost to follow-up; and the data of 5-year disease-free survival (DFS) were not available.According to the different treatment scheme for different patients, completion of the tumor operation or the anticipated chemotherapy or radiotherapy was determined as the end of initial treatment.
Finally, 72 patients (including 43 males and 29 females) with a median age of 54 (20-78)y were included.
Imaging Examination
Magnetic resonance imagingAll patients underwent examination with GE Signa Excite 1.5T or GE Signa Excite HD 3.0Tsystem (GE Healthcare, Milwaukee, WI).An 8- or 32-channel phase array head coil was used.During imaging, patients were placed in the supine position, and MRI was performed with the following sequences: T1 weighted images (T1WI), TR/TE=340-400ms/8.4-11.4ms; T2 weighted images (T2WⅠ) matrix 384×256, slice thickness of 3‐5 mm,interslice of 0.3‐0.5 mm, a field of view of 24 cm×24 cm, TR/TE was 2590-3460ms/108-118ms, NEX, 1-2.Axial, coronal,and sagittal contrast-enhanced T1WI were also obtained after contrast media injection at the rate of 2.5 mL/s.TR/TE=440-700ms/11.1‐11.3ms, matrix, 512×512, NEX 2.
Computed tomography imagingContrast-enhanced CT was used by GE Lightspeed ultra 16 or 64 slices system (GE Healthcare, Milwaukee, WI, USA), 100 mAs, and 120 kⅤ.Briefly, 300 mgI/mL of contrast media (Ultravist, Bayer,Germany) were intravenously injected at the rate of 2.5 mL/s and the total dose of 100 mL.The slice thickness was 3 mm.
Data Collection
Clinical and pathological characteristicsThe detailed clinical manifestations and disease duration were clearly recorded.Some patients had multiple manifestations, which were separately recorded.Other data, including pathological subtypes and involvement of one or both eyes, and systemic immune diseases were also collected.The lymphoma subtype was defined pathologically based on cell morphology,immunohistochemistry, and molecular diagnosis[5].
Imaging characteristicsFor those patients that performed MRI and CT, MRI were mainly used for evaluation since the resolution of MRI is superior to CT.The imaging characteristics were as follows: 1) single or multiple lesions,where a single lesion was defined as one lesion in unilateral orbit, and multiple lesions were defined as more than one lesion in unilateral orbit or single or multiple lesions in each of bilateral orbits.2) tumor location, where the orbital region was divided into 7 areas,i.e., eyelid, conjunctiva, lacrimal gland,eyeball, muscle cone, intra-muscle, and extra-muscle cone.The site of the main body of the tumor was recorded as the tumor location.For multiple lesions, the site of the main body of the largest tumor was recorded.3) tumor growth pattern,which included localized or diffuse pattern.4) MRI signal intensity, where muscles of the same level were used as the reference, so on T1WI, the signal was classified as hyper-, iso-, or hypointensity, and on T2WⅠ, the signal was classified as hyper‐,iso-, or hypointensity.5) contrast enhancement degree, where muscles of the same level were used as the reference, so the enhancement degree was classified as an obvious, moderate,or slight enhancement.6) contrast enhancement pattern, which was homogeneous or heterogeneous that may reflect the extent of the tumor malignancy.When the tumor enhancement was heterogeneous on either MRI or CT, this was considered as a heterogeneous enhancement.
TreatmentsThe treatment methods were different because of the different pathological types, including surgery,radiotherapy, or chemotherapy, were recorded.In addition, if one patient was treated with two or more treatment methods in combination, this was also recorded in detail.These treatment methods were determined based on the concurrent European Society of Medical Oncology clinical practice guidelines.
Follow-upThe follow-up data of the patients were mainly performed by reviewing the Inpatient Medical Record System,outpatient visiting, or telephone calls.For the patients who were followed-up by medical Record System or outpatient visiting, the follow-up was applied with physical and imaging examination for the whole body.For the patients who were followed-up by telephone call, the local hospital examination was also asked in order to get the reliable results.The images(CT/MRI) were used for evaluation of tumor remission or recurrence at three months after the end of treatment.The primary endpoint of the follow-up was 5-year DFS, which was defined as the time from the completion of surgical or other treatments, after which the disease was in complete remission to the first recurrence or metastasis.The final follow‐up time of the patients was May 31, 2022.
Statistical AnalysisSPSS 22.0 software was used for the data analysis.Quantitative data were described by means and standard deviations, and qualitative data were described by frequencies and percentages.A normality test was performed for all quantitative data, and then an independentt-test or Mann-WhitneyUtest was used for the statistical analysis according to the normality test results.Qualitative data were compared by the Chi-square test or Fisher’s exact test.Logistic regression was used for the multivariate analysis of the factors associated with DFS.All statistical analyses were two-sided,andP<0.05 was considered statistically significant.Kaplan-Meier test was used for the survival analysis of DFS.
RESULTS
Clinical and Pathological Characteristics
Clinical manifestationsFollowing clinical manifestations were observed: eyelid swelling (n=42), protopsis (n=35),ocular pain (n=25), conjunctivitis (n=23), self-perception of mass (n=20), visual acuity or field changes (n=18),blepharoptosis (n=15), and ophthalmoplegia (n=9).
The patient’s disease duration was 3-61d, with the median time, 35d.Two patients had Hashimoto’s thyroiditis, and one patient had IgG4-related disease.
Pathological subtypesThe pathological subtypes included extra-nodal marginal zone B-cell lymphoma (EMZL;n=56,77.8%), diffuse large B‐cell lymphoma (n=10, 13.9%), mantle cell lymphoma (n=3, 4.2%), follicular lymphoma (n=1, 1.4%),T-cell lymphoblastoma (n=1, 1.4%), and NK-T cell lymphoma(n=1, 1.4%).
Involvement of orbitsAmong patients included in this study,51 had lymphoma involving one orbit (70.8%, 51/72), while two eyes were involved in 21 patients (29.2%, 21/72).
Imaging characteristicsA total of 61 patients underwent contrast-enhanced MRI examination, and 35 patients underwent contrast-enhanced CT scanning.
1) The single lesion was found in 42 patients (58.3%) and multiple lesions in 30 patients (41.7%).2) The main body of the tumor was in the conjunctiva, eyelid, muscle cone, intramuscle cone, extra-muscle cone, lacrimal gland, and eyeball regions in 25 (34.7%), 15 (20.8%), 10 (13.9%), 10 (13.9%), 5(6.9%), 5 (6.9%), and 2 (2.8%) patients, respectively.3) The mass showed localized growth in 21 patients (29.2%) and diffuse invasive growth in 51 patients (70.8%).4) Among 61 patients who underwent MRI scanning, all the tumors showed hypointensity on T1WI.Also, on T2WI, the tumors showed isointensity in 13 patients (21.3%) and hyperintensity in 48 patients (78.7%).Obvious, moderate, and slight enhancement were found in 41 (67.2%), 15 (24.6%), and 5 (8.2%) patients,respectively (Figure 1).5) Homogeneous enhancement was found in 67 patients (93.1%), while heterogeneous enhancement was found in 5 of them (6.9%).
Among 35 patients who underwent CT scanning, obvious,moderate, and slight enhancement were found in 25 (71.4%), 6(17.1%), and 4 (11.4%) patients, respectively (Figure 2).
Treatment strategySurgical treatments included total or partial resection.Patients received a total dosage of 30-46 Gy, with a single dose of 1.8-2 Gy and 15-23 fractions during radiotherapy.The CHOP or R-CHOP regimen was used for the chemotherapy, and the patients received 4-8 cycles of treatment according to their conditions.In this study, 9 patients (12.5%) received only surgical treatment,10 patients (13.9%) were treated by radiotherapy, 5 (6.9%)were treated by chemotherapy, 22 (30.6%) were treated by surgery and radiotherapy, 15 (20.8%) were treated by surgery and chemotherapy, 8 (11.1%) were treated by surgery and chemoradiotherapy, and 3 patients (4.2%) were treated by chemoradiotherapy.
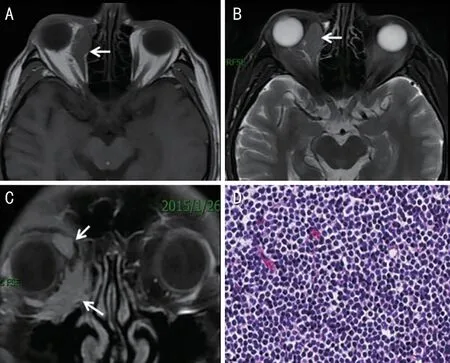
Figure 1 A male 47 years old patient suffered from right eyelid swelling for two months A: MRI axial T1-weighted image (T1WI);B: Axial T2-weighted image (T2WI); C: coronal contrast-enhanced T1 weighted image (T1WI); D: Photomicrograph (hematoxylin-eosin stain; x100).The tumor is located at the right rectus medialis and extra-muslecone with multiple lesions (A-C, arrows).The tumor showed hypointensity on T1WI, hyperintensity on T2WI referenced to the muscle at the same level, and homogeneous and obvious enhancement after contrast-media injection.The pathological finding is extra-nodal marginal zone B-cell lymphoma (EMZL; D).Radiotherapy was performed after surgery, and no tumor recurrence was found through 68mo of the follow-up period.

Figure 2 A male 54 years old patient suffered from bilateral ocular pain for one month A-C: Contrast-enhanced computed tomography(CT) images.The invasive tumor involved the left muscle cone, intramuscle cone (black arrows), and right eyelid (white arrow).D: The photomicrograph (hematoxylin-eosin stain; ×100) showed diffuse B-cell lymphoma.Clinical complete remission was obtained after 6 cycles of chemotherapy.The tumor recurrence occurred 18mo later.
Follow-upThere were 4 patients that were lost in the study.The lost visit rate was 5.3% (4/72+4), which was lower than 10% for satisfying the statistical demands.The median followup time was 66mo (2-105mo).Fifty patients (69.4%) achieved 5-year DFS, and tumor recurrence or metastasis occurred in 22 patients (30.6%) within the 5-year follow-up period.
Statistical FindingsUnivariate analysis showed that involvement of orbits (uni- or bilateral), single or multiple lesions, treatment strategies, and homo- or heterogeneous enhancement significantly differed when predicting 5-year DFS (P=0.022, 0.042, <0.001, and 0.028, respectively), while the other indicators were not significantly different.Further multivariate analysis showed that involvement of orbits (unior bilateral), treatment strategies, and homo- or heterogeneous enhancement were statistically significant for predicting 5‐year DFS (Table 1).Figure 3 shows the survival curve of the total 5-year DFS, as well as curves of 5-year DFS of involvement of orbits (unilateral or bilateral), treatment strategies, and homoor heterogeneous enhancement, respectively.
Taking into consideration the findings of this study, the previous literature, and the poor treatment effects of only surgery for lymphoma, the treatment methods in this study were categorized into 4 groups,i.e., only surgery group,radiotherapy or surgery + radiotherapy group, chemotherapy or surgery + chemotherapy group, and chemoradiotherapy or surgery + chemoradiotherapy group.
DISCUSSION
B-cell lymphoma is the dominant primary orbital lymphoma type, accounting for more than 90% of all primary orbital lymphomas[1-3,6-7].In the present study, there were 70 patients with B-cell lymphoma, accounting for 97.2% of all tumors.EMZL was found in 56 patients, diffuse large B‐cell lymphoma in 10 patients, while other patients were with mantle cell lymphoma (n=3) or follicular lymphoma (n=1).A previous study reported a slightly higher prevalence of orbital lymphoma in males than females,i.e., the male-to-female ratio of 1.25:1[4], which is consistent with our results revealing the ratio of 1.48:1.The tumors mainly occurred in middle-aged or elderly subjects.The median age of patients in this study was 54y, which was in accordance with previous studies[1-3,8].

Figure 3 A 5-year disease-free survival (DFS) curve (A), DFS curves at uni- or bilateral orbital involvement (B), treatment schemes (C), and enhancement pattern (D) Bilateral orbital involvement, surgery only,and heterogeneous enhancement predicted lower 5-year DFS (blue lines; P<0.001).
In the present study, we found that the variables of involvement of orbits (uni- or bilateral), treatment strategies,and homo- or heterogeneous enhancement were the three important indicators influencing the 5-year DFS.Unilateral orbital involvement, a combination of multiple therapies, and homogeneous enhancement of lesions were all associated with better outcomes.Unilateral orbit involvement was commonly found in the primary orbital lymphoma, especially for EMZL and diffuse large B‐cell lymphoma, while patients with bilateral orbits involved were mainly with mantle cell lymphoma[1,9].In this study, 21 patients had bilateral orbits involved, accounting for 20.2% of all patients, which was higher than reported by previous studies.The difference could be that our patients were treated for more complex conditions than those in those other studies.Of the 3 patients with mantle cell lymphoma, 2 were with bilateral orbits involvement, which was in agreement with the findings of previous studies.Bilateral orbits involvements have been associated with higher tumor burden and more advanced clinical stage of the lesion, which may predict poorer outcomes than unilateral involvement.Lesions in patients with involved bilateral orbits were mainly at the conjunctiva, which affected 13 patients (61.9%) in this study and was consistent with previous studies[1,10].
Surgical treatment is generally performed for patients with unclear preoperative diagnosis or for alleviating tumorderived symptoms.However, surgical treatment alone is insufficient for improving the outcomes of lymphomas[1,10-12].In this study, among 9 patients who received only surgical treatment with no subsequent treatments, tumor recurrence occurred 2-30mo after the operation.For low-grade lymphoma such as EMZL, a moderate dose of radiotherapy has good treatment efficacy[10-14], while for tumors with relatively highgrade malignancies, such as diffuse large B-cell lymphoma,chemotherapy or chemoradiotherapy is generally needed[14].In this study, chemoradiotherapy or combination therapy by two or more methods was associated with higher DFS.
As is well known, the pathological subtypes of lymphoma are associated with the patients’outcomes.The patients with EMZL have a relatively good prognosis due to the moderately low-grade malignancy[15-18].However, in this study, thepathological subtypes were not significantly associated with 5-year DFS, which could be attributed to the fact that 7 patients with EMZL were treated only by surgery and experienced tumor recurrence within 5y, therefore influencing the statistical results.Previous studies reported that after standard, systemic treatment, the 5-year DFS of patients with EMZL could reach as high as >90%, making it one of the lymphomas with the best outcomes[4,19].

Table 1 Correlation of clinical and imaging characteristics and 5-year DFS in primary orbital lymphomas
The tumors with heterogeneous enhancement on images generally occur because of the rapid tumor growth but insufficient blood supply, resulting in tumor necrosis.Therefore,this imaging feature indicates a tumor with relatively highgrade malignancy[20-21].In this study, heterogeneous tumor enhancement was found in 5 patients who were diagnosed with diffuse large B‐cell lymphoma or mantle cell lymphoma,which usually have high-grade malignancy, and are indicative of relatively poor outcomes.
Univariate analysis showed that the influences of single versus multiple lesions on outcomes were statistically significant; however, they lost their predictive potential after multivariate analysis.It is possible that this indicator had a certain relationship with the indicator of uni- or bilateral orbit involvements, while the latter had a stronger correlation with the DFS of patients.
The clinical manifestations of patients varied substantially in this study, and they mainly included eyelid swelling, protopsis,and orbital pain.Previous studies suggested that protopsis of one eye could be used as a specific clinical characteristic of lymphoma, so imaging examinations such as MRI or CT are required for those patients[4,22-23].Lymphoma affects all orbit regions and is mainly found in the eyelid, conjunctiva,and peri-muscle cone regions.Namet al[10]reported that patients with lymphoma at the lacrimal gland had relatively poor outcomes, with 5-year DFS of only 57.1%.Svendsen and Heegaard[24]reported that patients with lymphoma at the eyeball had relatively poor outcomes.In this study, no significant correlation was found between the tumor location and DFS.
The incidence of primary orbital lymphoma has increased in recent years; however, the causes of this disease remain unclear.Several investigators suggested that the development of lymphoma, especially EMZL, may be associated with longterm chronic infections of the patients, such as chlamydia infection, helicobacter pylori infection, and chronic hepatitis[25-28].The immune status was also considered to be associated with the development of orbital lymphoma[29-30].Nuttinget al[31]reported that thyroid eye disease caused by Hashimoto’s thyroiditis could be the reason for developing orbital EMZL.In the study, two patients had Hashimoto’s thyroiditis, and one patient had IgG4-related disease.
The present study has some limitations.First, this is a retrospective analysis with inherent selection bias.Second,The patients included in this study is from a single center in China, and the number of cases was limited because of the low incidence of primary orbital lymphoma.Thus, multicenter,prospective studies with larger sample sizes are required in the future.Third, since this study focused on the 5-year DFS,the patients who were treated before 2018 were recruited.Some information such as tumor TNM stage or pathological immunohistochemistry could not be available for all the patients.Furthermore, some treatment methods at that time may be not very optimal from the perspective of the present.
In conclusion, B-cell lymphoma, especially EMZL, is the dominant type of primary orbital lymphoma.The uni- or bilateral orbital involvement, tumor enhancement pattern, and suitable treatment methods according to pathological subtypes resulted as essential factors affecting the patients’outcomes.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhu JB,None;Li B,None;Zhang HM,None;Wang NL,None.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Analysis of retinal arteriolar and venular parameters in primary open angle glaucoma
- ldentification and functional analyses of a novel FOXL2 pathogenic variant causing blepharophimosis, ptosis,and epicanthus inversus syndrome
- Protective effects of ferulic acid against ionizing radiation-induced oxidative damage in rat lens through activating Nrf2 signal pathway
- Novel homozygous ADAMTS17 missense variant in Weill-Marchesani syndrome
- Cost analysis of childhood glaucoma surgeries using the US Medicaire allowable costs
- Guidelines from an expert panel for the management of diabetic macular edema in the Malaysian population
