Residual refractive errors in pseudophakic eyes and related factors: a population-based study
Hassan Hashemi, Alireza Jamali, Farhad Rezavn, Alireza Hashemi, Mehdi Khabazkhoob
1Noor Research Center for Ophthalmic Epidemiology, Noor Eye Hospital, Tehran 1968653111, Iran
2Noor Ophthalmology Research Center, Noor Eye Hospital,Tehran 1968653111, Iran
3Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences,Tehran 1968653111, Iran
Abstract
INTRODUCTION
Recent reports indicate that 295 million people worldwide suffer from moderate to severe visual impairment and 43.3 million are blind[1].Cataracts are the first leading cause of blindness and the second cause of visual impairment accounting for 45% and 38.9% of cases of blindness and visual impairment, respectively[2].Surgical removal followed by intraocular lens (IOL) implantation is the common treatment for cataracts, with the main goal of improving the patient’s visual acuity and achieving the desired refractive outcome[3].Cataract surgery has been associated with successful and acceptable results in recent years due to knowledge development in this field with the emergence of modern surgical techniques, well-functioning biometric devices as well as evolving IOL designs[4-5].Achieving post-operative refraction within ±1.00 diopters (D) has increased from 72% in the 1990s to about 99% in recent studies[3,6].According to the Royal College of Ophthalmologists, 85% and 55% of patients are expected to achieve refraction within ±1.00 and ±0.50 D of emmetropia after cataract surgery, respectively[7].
Among various parameters affecting cataract surgery outcome,the selected IOL power is a quantitative and traceable factor[8].Numerous studies have emphasized that accurate measurement of ocular biometric indices and selection of the appropriate IOL power calculation formula are key factors in reducing residual refractive error after cataract surgery[8-10].Erroneous axial length (AL) and corneal power measurements, errors in predicting the anterior chamber depth (ACD) after surgery or the IOL location, and fluctuation in pupil size have been suggested as the associated factors of a refractive surprise after cataract surgery among various studies[11-12].
Most previous studies on refractive errors after cataract surgery have evaluated the two parameters of mean absolute error(MAE) and mean numerical error (MNE), which indicate the difference between the predicted error (PE) of the ⅠOL power calculation formulas and the spherical equivalent (SE) obtained after surgery[13-14].Although these two parameters implicitly provide valuable information about the refractive results after cataract surgery, they are unable to accurately describe the prevalence of refractive errors.There are limited studies on refractive errors in pseudophakic individuals[15]; and the factors related to the refractive surprise were not evaluated in these studies.We’re in a transitional period toward using newergeneration IOL power calculation formulas; therefore, studying the pattern of refractive errors based on previous-generation formulas could provide valuable information.Considering the importance of residual refractive error after cataract surgery,Iran’s population aging and so the need for more cataract surgeries in the coming years, and the lack of population-based studies in this field, the present population‐based report aimed to investigate refractive error distribution by age, sex, and AL in pseudophakic individuals.
SUBJECTS AND METHODS
Ethical ApprovalInformed consent was obtained from all participants.The principles of the Helsinki Declaration were followed in all stages of the study.The study protocol was approved by the Ethics Committee of the National Institute for Medical Research Development (NIMAD).
This report is a part of the Tehran Geriatric Eye Study (TGES); a cross-sectional population-based study conducted on the urban population of Tehran, Iran from January 2019 to January 2020.The target population was all residents aged 60y and above in Tehran.The sampling was performed using a multi-stage stratified random cluster sampling method.For this purpose,the 22 municipality districts of Tehran were considered as strata.Then, block maps of districts were prepared and each block was defined as a cluster.A total of 160 clusters were selected proportionally to size from 22 strata of Tehran city.After identifying clusters, a sampling team was sent to the address of each cluster and the first house was selected as the cluster head after being located on the southwest side of the selected block.Then, by moving counterclockwise while selecting the next households, all individuals 60y and older were invited to participate in the study.If a person was willing to participate in the study, informed consent was obtained and an identification card was issued to the person.Ⅰf a household was not present during sampling, the interviewers returned at another time preferably in the evening.All study participants were transferred to the study site free of charge on a prearranged day.
At the study site, a face‐to‐face interview was first conducted to collect complete demographic and case history information.Then, all study participants underwent a complete ocular examination and biometry.The uncorrected distance visual acuity (UCⅤA) was measured using an LED acuity chart(Smart LC 13, Medizs Inc., Korea) at 6 m.Then, objective dry refraction was performed using an auto-refractometer/keratometer (ARK-510A, Nidek Co.LTD, Aichi, Japan).The optimal distance optical correction was determined by the subjective refraction and the best-corrected distance visual acuity (BCⅤA) was recorded.Ⅰn the next step, a complete anterior and posterior segment ocular health examination was performed using a slit-lamp biomicroscope (B900, Haag-Streit AG, Bern, Switzerland) by an ophthalmologist.The posterior segment examination was undertaken using a +90 diopter (D)lens.The pseudophakia was diagnosed based on observing IOL through the slit-lamp biomicroscopy.Finally, all study participants underwent ocular biometry using IOL Master 500 (Carl Zeiss Meditec, Jena, Germany).Ocular biometry in pseudophakic eyes was performed using the device’s pseudophakic mode.All biometric measurements were performed according to the instrument’s standard protocol between 10a.m.and 4p.m.
Inclusion and Exclusion CriteriaEyes with a history of cataract surgery and IOL implantation (during the last 5y)were included in the analysis.Eyes with a history of ocular surgery except for uneventful cataract surgery, history of ocular trauma, pterygium, corneal opacity, severe meibomian gland dysfunction (MGD), and BCⅤA worse than 20/32 were excluded from the analysis.
Statistical AnalysisStatistical analysis was performed using the Stata software.If a person had two pseudophakic eyes,both eyes were analyzed and the correlation of the fellow eyes was considered in the analysis.Mean, standard deviation (SD),and interquartile range (IQR) of SE and absolute SE (based on objective refraction) were reported by age, sex, and AL groups.To assess predictability, SE within ±0.25, ±0.50, ±0.75, and±1.00 D of emmetropia were reported.Logistic regression was used to investigate the relationship between predictability and studied variables and odds ratios (OR) with 95% confidence intervals (CI) were reported.APvalue less than 0.05 was considered statistically significant.
RESULTS
Of the 3791 invitees, 3310 participated in the TGES (response rate: 87.3%).After applying the inclusion and exclusion criteria, 1677 eyes of 975 individuals were analyzed for this report.The mean age of the eligible subjects for this report was 71.95±7.17 (60 to 97)y and 540 (55.4%) of them were female.Of the analyzed eyes, 11.7% (n=193), 78.2% (n=1290), and 10.1% (n=167) had an AL shorter than 22 mm, 22 to 24.5 mm,and longer than 24.5 mm, respectively.
Table 1 shows the mean±SD and IQR of the SE and its absolute value by age, sex, and AL.As seen in Table 1, themean SE was -0.34±0.97 D and the mean absolute SE was 0.72±0.74 D with a median of 0.5 D.Figure 1 illustrates the distribution of SE in the whole sample.Figure 2 illustrates the box plot for the distribution of the absolute SE among different AL groups.As seen in Table 1, the mean SE was more negative(myopic) in females compared to males (P=0.011).However,there was no statistically significant difference in the mean absolute SE between males and females (P=0.509).The SE decreased with advancing age from -0.28 D in the age group 60-64y to -0.48 D in the age group 80y and above (P<0.001).The absolute SE increased significantly with age (P=0.002).There was a statistically significant difference in terms of SE and absolute SE among the AL groups (P<0.001).According to the posthoc test, the SE was significantly more hyperopic in the AL group lower than 22 mm compared to the AL group above 24.5 mm.Moreover, the absolute SE was significantly higher in individuals with an AL above 24.5 mm than in those with an AL lower than 22 mm (P<0.001).
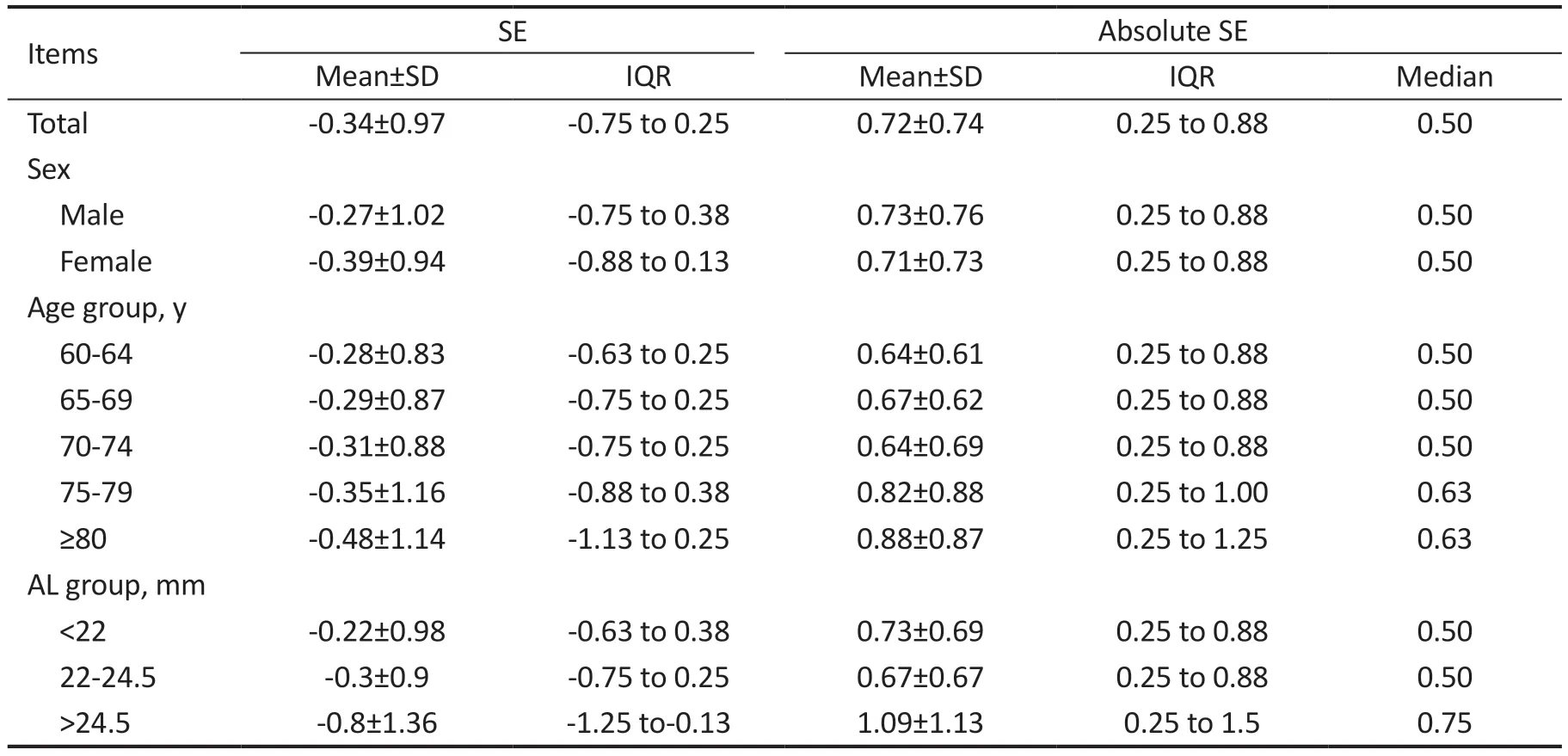
Table 1 Mean±SD, IQR of the SE and its absolute value by age, sex, and AL in pseudophakic eyes
The mean corneal astigmatism was 1.2±0.80 D (0 to 3.98 D)in the studied eyes.Our findings showed that 18.9% (n=306),31.7% (n=512), and 49.4% (n=798) of the studied eyes had corneal astigmatism lower than 0.50 D, 0.50 to 1.00 D, and higher than 1.00 D, respectively.
Table 2 shows the residual refractive error based on different cut points.As seen in Table 2, 32.68% (n=546, 95%CI: 30.27%-35.08%), 53.67% (n=900, 95%CI: 51.23%-56.1%), 68.99%(n=1157, 95%CI: 66.96%-71.02%), and 79.73% (n=1337,95%CI: 77.69%-81.76%) of the studies eyes had a residual SE within ±0.25, ±0.50, ±0.75, and ±1.00 D of emmetropia,respectively.The prevalence of predictability based on different cut points was not significantly different between males and females.However, predictability based on all cut points significantly decreased with advancing age (P<0.001).The prevalence of predictability based on the cut point of 0.25 D decreased from 72.33% in the age group 60-64y to 53.27% in the age group ≥80y.The predictability prevalence based on the cut point of 1.00 D was 84.88% in the age group 60‐64y which decreased to 70.38% in the age group ≥80y.The highest and lowest prevalence of predictability was observed in individuals with an AL between 22 and 24.5 mm and those with an AL above 24.5 mm, respectively.Table 2 shows that the highest frequency of residual refractive errors within 0.25 and 1.00 D was related to the AL groups 22 to 24.5 mm and above 24.5 mm, respectively.The prevalence of predictability based on the cut points of 0.25 and 1.00 D in the AL group 22-24.5 mm was 34.57% and 81.63%, respectively which was higher than in other AL groups.

Figure 1 The distribution of SE in pseudophakic eyes SE: Spherical equivalent.

Figure 2 The distribution of SE in pseudophakic eyes according to the AL SE: Spherical equivalent; AL: Axial length.

Table 2 The percentage of eyes within ±0.25, ±0.5, ±0.75, and ±1 D of emmetropia according to age, sex, and AL
Table 3 shows the relationship between predictability based on different cut points of residual refractive error with age,sex, diabetes, and AL according to the simple and multiple logistic regression models.According to the multiple logistic regression model, advancing age was associated with a statistically significant decrease in predictability for all cut points.Moreover, the prevalence of predictability based on all cut-points was significantly lower in individuals with an AL>24.5 mm compared to those with an AL between 22 to 24.5 mm.Based on the cut-point of ±0.25 D, individuals with an AL<22 mm also had worse predictability compared to those with an AL between 22 to 24 mm.
DISCUSSION
The quality of vision and post-operative residual refractive error are important considerations in cataract surgery.In this report, we investigated in detail the refractive outcomes in pseudophakic eyes through a population-based study.Our main goal was to determine the accuracy of IOL power calculation in Tehran.In the present study, individuals were randomly selected from all over Tehran city, and therefore the study results cover a wide range of surgeons, private and public centers as well as different biometric and IOL power calculation methods.Although our findings may not have high internal validity, they could be well generalized to the whole of Tehran city, even the whole of Iran, and other communities considering the above points.Therefore, our results are valuable from the public health point of view.The findings of the present study indicate that most errors in calculating the IOL power occurred under what conditions in recent years and these results can be used as a basis for using newergeneration formulas.One of the most important limitations of this report is that slight changes in refractive error over time may be due to factors other than the IOL power calculation,which should be taken into account; however, this limitation does not seem to significantly affect results due to the large sample size.
The mean SE was -0.34±0.97 D in the present study, which is more negative than the values reported in the studies by Broganet al[3](-0.19±0.99 D), Rementería-Capeloet al[16](-0.16±0.48 D), and Aristodemouet al[15](-0.06±0.84 D) and is more positive compared to the value found in the study by Nangiaet al[17](-0.89±1.08 D).Residual refractive error after cataract surgery can be evaluated implicitly by the MAE,which represents the absolute difference in the postoperative SE and the prediction error of the IOL power calculation formula.It has been shown that the lower MAE, the higher the uncorrected visual acuity after the surgery[14].In the present study, we evaluated the postoperative absolute value of the SE as we had no access to preoperative data including biometry data, and the type of formula used for IOL power calculation.The average postoperative absolute SE was 0.72±0.74 D in the present study (undoubtedly, not considering the prediction error has affected this value), which is significantly higher than the values observed in various studies.Table 4 presents the results of different studies in this regard[18-28].
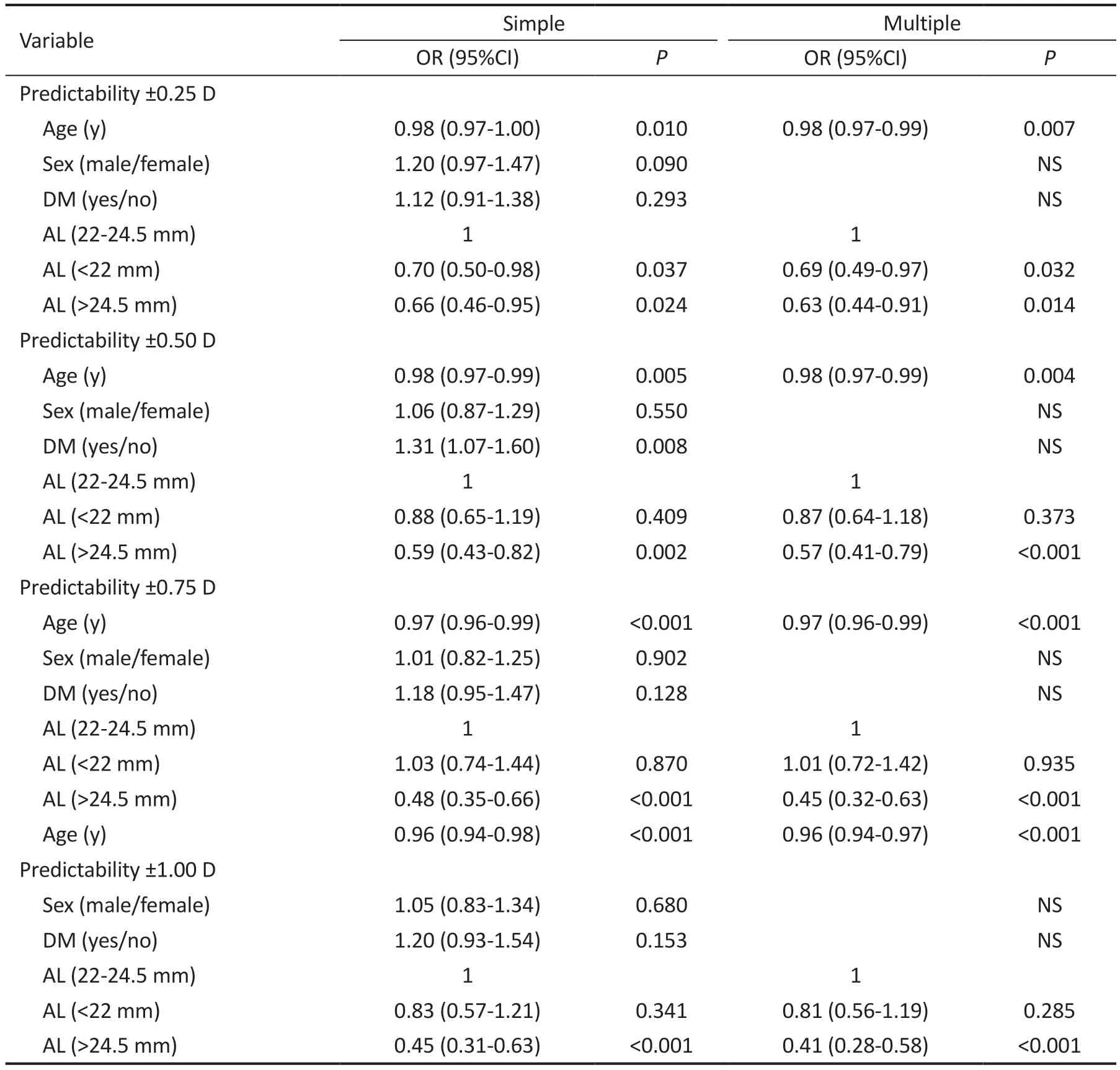
Table 3 The association of residual refractive errors with age, sex, and AL using simple and multiple logistic regression models
The results of the present study indicated a lower percentage of individuals having residual refraction within ±0.25 D of emmetropia compared to most previous studies.Looking at Table 4, it can be seen that most of the studies that used oldergeneration IOL power calculation formulas obtained a lower percentage of ±0.25 D postoperative refraction.For example,the results of the study by Kaneet al[23], are not significantly different from the present study.Ⅰt should be noted that some studies reported a lower percentage than the present study[24].However, this finding was reported to be 78% in the study by Iijimaet al[27]; that study used the Barret Universal 2 formula indicating the high accuracy of this formula for IOL power calculation.
The frequency of postoperative refraction within ±1.00 D of emmetropia has been reported up to 99% in previous studies[28].In general, recent studies reported better results and this could be attributed to the use of newer and better IOL power calculation formulas and even the use of more advanced biometric devices.However, the optimization of IOLs and their constants in recent decades should not be overlooked.It should also be noted that the present study included a heterogeneous sample of cataract surgery candidates.In this sample, there may be individuals with challenging conditions for IOL power calculation, such as those with a history of refractive surgery or vitrectomy, keratoconus, and long/short eyes.On the other hand, some studies have reported optimal outcomes due to strict exclusion criteria, such as the absence of any ocular disease other than cataracts (study by Hahnet al[29]or the inclusion of individuals with only normal AL (between 22 and 24.5 mm)[30]; so, their results could not be generalized to the general population.
Factors associated with residual refractive error after cataract surgery are generally divided into two groups; unplanned and surgeon decision-dependent[31].The most important factor that is common between the two groups is the lack of appropriate IOL selection according to the patient’s ocular conditions.The errors in measuring ocular biometric parameters have been greatly reduced by providing modern accurate biometryinstruments; however, IOL power calculation remains an important issue in cataract surgery, which significantly affects UCⅤA and refractive status postoperatively[13].In the present study, only factors related to the reduction of refractive predictability after cataract surgery were investigated regardless of the type of implanted IOL.Most IOL calculation
formulas work well in eyes with AL between 22 and 24.5 mm[13];the AL outside this range could cause significant differences in the IOL power values obtained by different formulas[32].The results of the present study showed that 27% of eyes with short AL, 34.5% with normal AL, and 25.75% with long AL had a postoperative residual refractive error within ±0.25 D of emmetropia.Moreover, 79%, 82%, and 66% of these eyes had a postoperative SE within ±1.00 D of emmetropia,respectively.

Table 4 Summary of previous studies
According to the results of the present study, the best predictability results were observed in the eyes with normal AL followed by eyes with short, and long ALs, respectively.A look at previous studies also confirms this finding.The errors of optical biometry seem to be higher in measuring long ALs due to more vitreous contribution[33].Moreover,ocular comorbidities are more common in eyes with long ALs.For this purpose, the effect of AL is adjusted in the newergeneration formulas to reduce postoperative errors[34].It is expected that residual refractive errors after cataract surgery especially in eyes with long ALs, will be reduced in the coming years as newer-generation formulas become more widespread.In addition, the biometry and IOL power calculation errors are significantly higher in short eyes than in eyes with normal AL.According to the literature, 17% to 54% of the errors in IOL power calculation could be attributed to the incorrect AL measurement[11,35].
According to the results, a more negative SE was found in participants with long AL compared to those with normal AL as well as in participants with normal AL compared to those with short AL.Meanwhile, the IOL power is usually calculated lower than the required power in eyes with long ALs, leading to hyperopic results after surgery; one of the possible influential factors for this observation is the effect of corneal astigmatism on SE calculation.The mean corneal astigmatism was 1.2 D in the present study and part of the observed residual SE is related to this astigmatism.The refractive error will not be completely corrected when there is significant corneal astigmatism not corrected by a toric ⅠOL[36]or relaxed incision[37]or if an implanted toric IOL rotates over time[38].Achieving the postoperative SE near Plano is the basis for calculating spherical IOL power by most IOL power calculation formulas if astigmatism correction is not planned.However, lack of access to adequate spherical power or calculation error leads to undesirable SE after cataract surgery.Therefore, the presence of corneal astigmatism and its lack of correction include both unplanned and surgeon decisionrelated factors.
The postoperative ACD or in other words, the effective lens position was reported to be the most important factor influencing the accuracy of ⅠOL power calculation in a study by Norrby[11].Roessleret al[39], also introduced the AL and postoperative ACD as two important factors influencing the IOL power calculation.In the present study, it was not possible to evaluate the accuracy of the effective IOL position due to the lack of knowledge of the preoperative ACD and agerelated changes in corneal power.Therefore, we were not able to evaluate some parameters despite the possibility of their influence on the IOL power calculation.Overall, it can be concluded that the error in the effective lens position is probably another unintended factor that may have influenced the findings of the present study.
Our findings showed increasing refractive errors in pseudophakic individuals with advancing age.Since the information about the exact time of the surgery was not available in the present study and the surgeries were performed by different surgeons during different years, several factors can be involved.First, ocular comorbidities in the elderly may cause refractive errors after cataract surgery[40].In addition, factors such as fixation errors and unwanted shifts in gaze direction may compromise the accuracy of biometric measurements in older ages.On the other hand, the age cohort effect should not be overlooked.Older people probably underwent cataract surgery years ago when biometric devices and IOL power formulas were less accurate than in recent years[41].Therefore, it is reasonable to see higher residual refractive errors in older ages.
According to the results, the mean SE was more negative in females than in males.The sex-related differences in ocular biometry and the prediction error of the IOL power calculation formulas[42]make one expect the error to be higher in women which confirms our findings.However, Behndiget al[43]stated that the residual refractive error has decreased compared to the past with increasing use of newer-generation IOL power formulas (especially Haigis) in eyes with shorter AL and steeper cornea (like women’s eyes).It should be noted that a lower amount of MAE has been reported in the newly introduced Kane formula which considers sex as an effective factor in determining IOL power[44].
In conclusion, we observed that the mean SE in Iranian pseudophakic individuals was higher than reported in other populations.Subgroup analysis by AL showed that the ALs outside the range of 22 to 24.5 mm were associated with a higher post-operative residual refractive error.However, other factors such as post-operatice ACD, sex, increasing age, and error in choosing the right formula can also affect the outcome of the surgery.
ACKNOWLEDGEMENTS
Foundation:Supported by National Institute for Medical Research Development (NIMAD) affiliated with the Iranian Ministry of Health and Medical Education (No.963660).
Conflicts of Interest:Hashemi H,None;Jamali A,None;Rezavn F,None;Hashemi A,None;Khabazkhoob M,None.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Analysis of retinal arteriolar and venular parameters in primary open angle glaucoma
- ldentification and functional analyses of a novel FOXL2 pathogenic variant causing blepharophimosis, ptosis,and epicanthus inversus syndrome
- Protective effects of ferulic acid against ionizing radiation-induced oxidative damage in rat lens through activating Nrf2 signal pathway
- Novel homozygous ADAMTS17 missense variant in Weill-Marchesani syndrome
- Cost analysis of childhood glaucoma surgeries using the US Medicaire allowable costs
- Predicting the prognosis of primary orbital lymphoma by clinical characteristics and imaging features
