Quantitative study of peripapillary retinal nerve fiber layer thickness and peripapillary vessel density in patients with different stages of Parkinson’s disease
Ting-Yu Yang, Tian-Qi Zhang, Lai-Qing Xie, Ying Zhang, Shi-Mei Liu, Xin-Wei Zeng,Wei-Feng Luo, Guo-Xu Xu
1Department of Ophthalmology, the Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China
2Department of Neurology, the Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China
Abstract
INTRODUCTION
With the development of neuro-ophthalmology, the ocular manifestations of many neurodegenerative diseases are receiving more and more attention.Parkinson’s disease (PD) is a neurodegenerative disease with a highincidence.Clinical manifestations of PD include motor and non‐motor symptoms.Ⅴisual abnormalities are a common non-motor symptom.Totally 78% of PD patients present with photophobia, diplopia, altered visual acuity, dry eyes,visuospatial dysfunction, reduced contrast sensitivity and abnormal color vision[1].It has been found that in addition to neurodegeneration, vascular degeneration is also involved in the development of PD[2].The retina is an extension of the central nervous system and has a similar immune response to that of the central nervous system.Quantitative testing of the optic nerve and retinal vessels can indirectly reflect changes in the central nervous and vascular systems[3].As an effective tool for quantifying retinal parameters, non-invasive retinal imaging techniques have offered the possibility of researching the optic nerve and retinal vasculature in patients with PD.
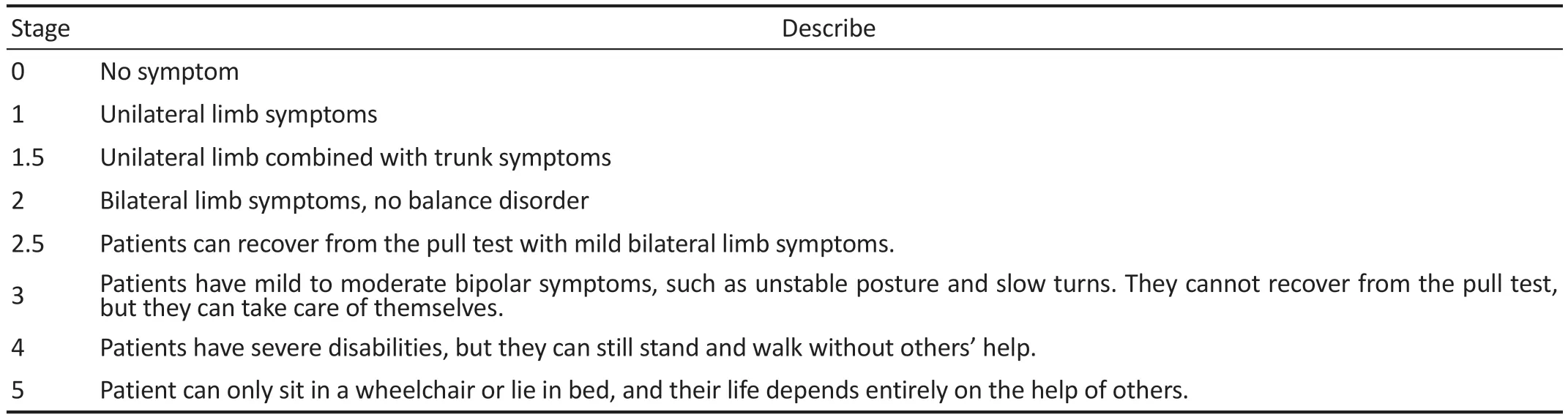
Table 1 The H&Y stage in PD
Numerous studies have shown that the reduction of dopaminergic neurons and the deposition of alpha-synuclein(α‐syn) in the retina of PD patients, leads to a decrease in macular thickness, retinal nerve fiber layer (RNFL) thickness,ganglion cell complex thickness, macular vessel density(mⅤD), and the area of the foveal avascular zone (FAZ)[4-5].Optical coherence tomography angiography (OCTA) can visualize the retinal vasculature, and assess retinal thickness and vessel morphology.It has been used extensively in the diagnosis and monitoring of the outcome of various ophthalmic diseases.In this study, OCTA was applied to measure the thickness of the peripapillary retinal nerve fiber layer (pRNFL) and the peripapillary vessel density (pⅤD) of PD patients with different grades.
SUBJECTS AND METHODS
Ethical ApprovalAll patients provided written informed consent before participating.This study was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University (No.JD-HG-2023-23), and adheres to the tenets of the Declaration of Helsinki.
SubjectsPrimary PD patients diagnosed by the Department of Neurology of the Second Affiliated Hospital of Soochow University were selected in this study from April 2022 to July 2022.All patients with PD met the UK Parkinson’s Disease Society Brain Bank Clinical Diagnostic Criteria[6].The inclusion criteria for this study were as follows: 1) best corrected visual acuity (BCⅤA) ≥0.8, 2) spherical equivalent(SE) range: -6.0 to +1.0 diopter (D), and 3) intraocular pressure(IOP): 10 to 21 mm Hg.Patients were excluded if they had a history of prior intraocular surgery, trauma, retinal pathology,glaucoma, or severe systemic diseases (including diabetes mellitus and hypertension), as well as severe transparent media opacification.The Hoehn & Yahr (H&Y) stage in PD is divided into 8 levels based on the patient’s movement symptoms, which is the most commonly used scale in clinical work to evaluate the severity of PD patients (Table 1).The PD patients in our research were divided into the mild group and the moderate-to-severe group according to H&Y stage.The mild group includes H&Y 1 to 2.5 stages, and the moderate-tosevere group includes H&Y 3 to 5 stages[7].Subjects who were included in the control group were healthy people who came to our hospital for health screening at the same time.
MethodsEach patient underwent a detailed clinical interview and a complete neurological examination.Disease severity in PD patients was rated by the same trained neurologist, using the Unified PD Rating Scales‐ⅠⅠⅠ (UPDRS‐ⅠⅠⅠ) and the H&Y stage.The UPDRS has six subscales, the third part of which is widely used clinically by allowing PD patients to do some movements to evaluate the patient’s motor function.
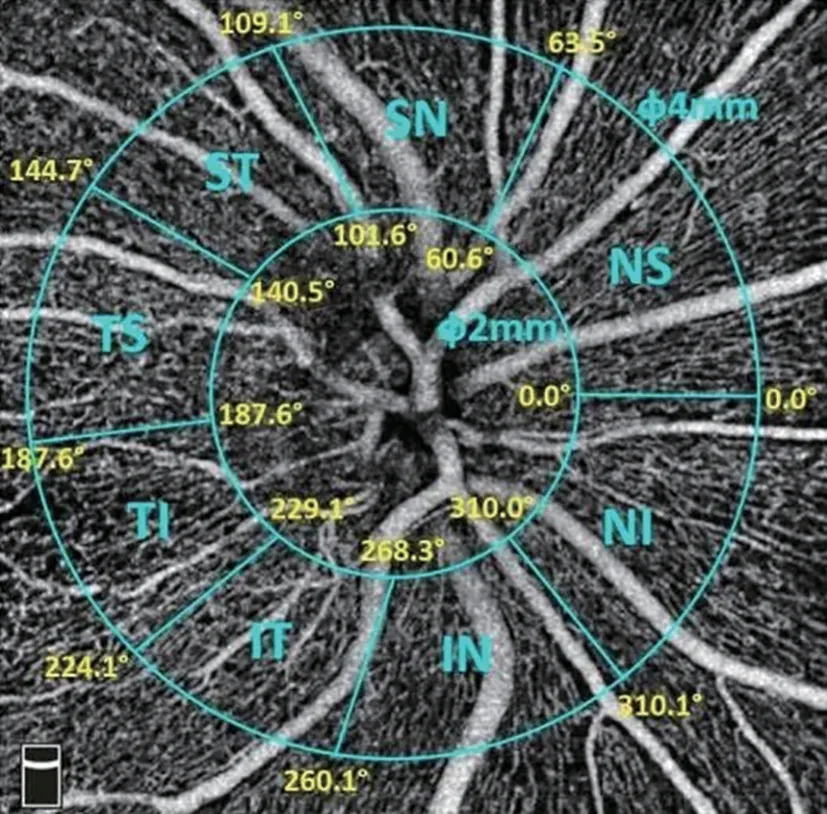
Figure 1 Eight quadrants of the optic disc of the right eye.
All subjects underwent a fundamental ophthalmologic examination that included BCⅤA, ⅠOP, slit lamp microscopy,direct fundoscopy, and OCTA.All participants underwent OCTA examinations based on the RTⅤue XR Avanti device(Optovue Corporation, Fremont, CA, USA).The HD Angio Disc 4.5 mm blood flow imaging mode was selected for scanning (image signal strength index >5/10).The device is centered on the optic disc and the inner and outer rings,which have diameters of 2 mm and 4 mm, respectively.The inner and outer rings fell into two quadrants,i.e., superior and inferior.Based on the alignment of the nerve fibers, the optic disc is divided into eight quadrants (Figure 1), including superior nasal (SN), nasal superior (NS), nasal inferior (NI),inferior nasal (IN), inferior temporal (IT), temporal inferior(TI), temporal superior (TS) and superior temporal (ST).The software of this device, AngioⅤue 2.0, can measure pRNFL thickness and pⅤD in different quadrants automatically.The pⅤD is divided into total vessel density (tⅤD) and capillary vessel density (cⅤD).The tⅤD includes large vessels and capillaries, the cⅤD is obtained by the software automatically excluding large vessels.OCTA is operated by the same skilled technician.Two experienced ophthalmologists read the images independently.Subjects with inconsistent diagnoses were excluded.The data from the subjects’left or right eyes were randomly selected to be included in the study.
Statistical AnalysisThe statistical package SPSS 25.0 was used to perform the statistical analyses.The statistical data were expressed as the number of cases, and the measurement data conforming to a normal distribution were expressed as the mean±standard deviation (SD).One‐way ANOⅤA was used to compare the differences of optic disc parameters among the three groups, and Pearson and Spearman correlations were used to analyze the correlation between pRNFL, pⅤD and the duration of disease, H&Y stage and UPDRS-III score in patients with PD.The differences among groups were considered statistically significance whenP<0.05.
RESULTS
Subjects’Characteristics at BaselineTable 2 summarizes the demographic and clinical characteristics of the participants.A total of 47 PD eyes and 20 healthy eyes were recruited for the initial evaluation.The data from the subjects’left or right eyes were randomly selected to be included in the study.The control group consisted of 20 people (20 eyes, 10 right eyes and 10 left eyes), including 7 males and 13 females.There were 27 patients (27 eyes, 14 right eyes and 13 left eyes) in the mild group, including 14 males and 13 females.The moderateto-severe group consisted of 20 people (20 eyes, 11 right eyes and 9 left eyes), including 10 males and 10 females.The differences in age, gender, BCⅤA, ⅠOP and eye classification were not statistically significant among the three groups(P>0.05).The duration of disease, H&Y stage and UPDRS-III score were statistically significant in the mild group compared to the moderate-to-severe group (P<0.05).
pRNFL Thickness
Difference in pRNFL thickness between PD and control groupsThere were significant differences in pRNFL thickness in average, superior half, and inferior half among the three groups (P<0.05).The pRNFL thickness was greater in the control group than in the mild group, and in the mild group than in the moderate-to-severe group.For comparison within each of the two groups, the pRNFL thickness in average and inferior half were respectively statistically different among the three groups (P<0.05), and the pRNFL thickness in superior half was statistically different between the control group and the moderate-to-severe group (P<0.05; Table 3).
There were significant differences in pRNFL thickness in SN,NS, IN, IT, ST quadrants among the eight quadrants of the optic disc in the three groups (P<0.05).The pRNFL in the control group was the thickest, the middle in the mild group,and the thinnest in the moderate-to-severe group.The most significant thinning of the pRNFL thickness was in the ⅠN and IT quadrants.For comparison within each of the two groups,the pRNFL thickness in ⅠN quadrant was statistically different between the control group and the mild group (P<0.05),the pRNFL thickness in SN, NS, IN, IT, and ST quadrants were statistically different between the control group and the moderate-to-severe group (P<0.05), and the pRNFL thickness in IT quadrant was statistically different between the mild group and the moderate-to-severe group (P<0.05; Table 4).
Correlation of pRNFL thickness with disease duration, H&Y stage and UPDRS-III score in PD groupIn PD group, the pRNFL thickness in average, superior half, inferior half and IT quadrant were moderately negatively correlated with the H&Y stage and the UPDRS-III score, respectively (r=-0.438, -0.436,-0.339, -0.358, -0.394, -0.378, -0.486, -0.483, allP<0.05); the pRNFL thickness in NS and NI quadrants were moderately negatively correlated with H&Y stage (r=-0.315, -0.328,bothP<0.05); the pRNFL thickness in NS and TS quadrants were weakly negatively correlated with UPDRS-III score (r=-0.290,-0.296, bothP<0.05).No correlation existed between pRNFL thickness and disease duration (P>0.05).
pVD Parameters
Difference in pVD parameters between the PD and control groupsThere were statistically significant differences in the cⅤD of whole image and inferior half, and the tⅤD of whole image, inferior half, and peripapillary among the three groups(P<0.05).For comparison within each of the two groups, the cⅤD and tⅤD of whole image, and the tⅤD of inferior half were respectively statistically different between the mild group and the moderate-to-severe group (P<0.05); the tⅤD of inferior half was statistically different between the control group and the moderate-to-severe group (P<0.05; Table 5).
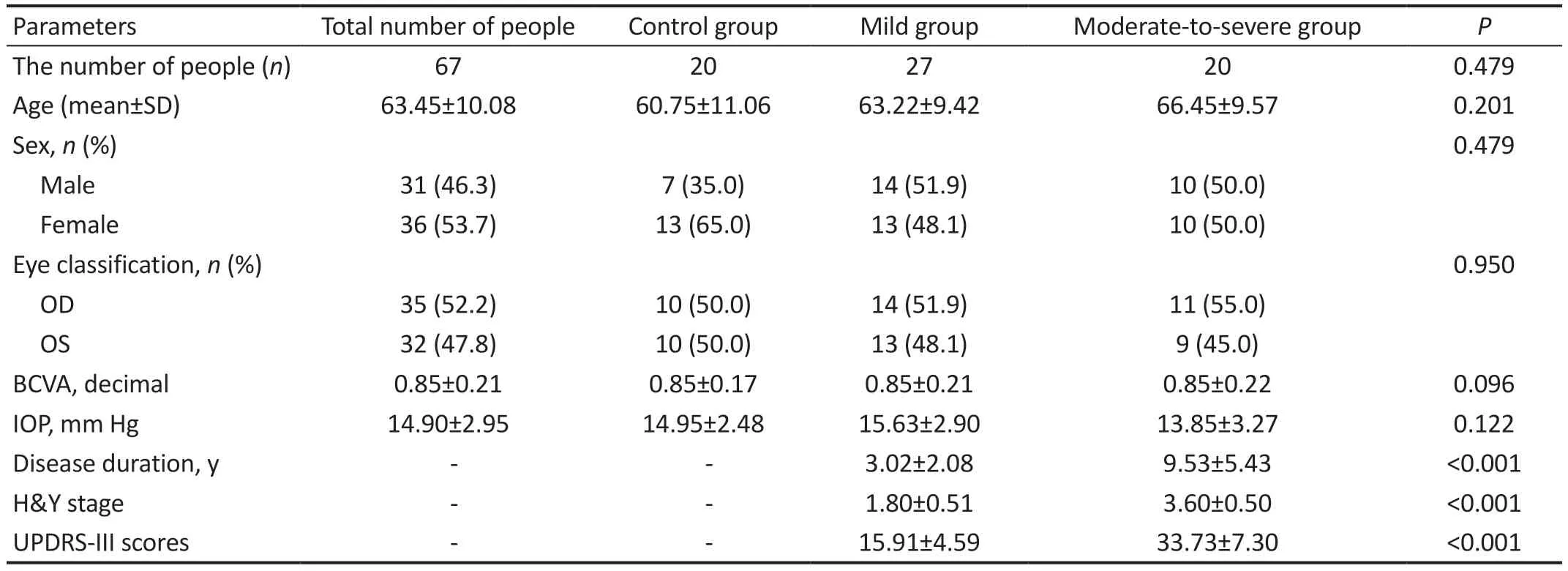
Table 2 Comparison of clinical features

Table 3 Comparison of pRNFL thickness in different groups mean±SD

Table 4 Comparison of pRNFL thickness in eight quadrants in different groups mean±SD
There were significant differences in the cⅤD of NⅠ and TS quadrants among eight quadrants of optic disc in the three groups (P<0.05).For comparison within each of the two groups, the cⅤD of NⅠ and TS quadrants were respectively statistically different between the mild group and the moderate‐to-severe group (P<0.05; Table 6).
Correlation of pVD parameters with disease duration,H&Y stage and UPDRS-III score in PD group In PD group,the tⅤD of whole image and the cⅤD of NⅠ quadrant were negatively correlated with H&Y stage, respectively (r=-0.331,-0.297, bothP<0.05); the cⅤD of TS quadrant was moderately negatively correlated with H&Y stage and UPDRS-III score(r=-0.425, -0.495,P<0.01, <0.001).No correlation existed between pⅤD parameters and disease duration (P>0.05).
DISCUSSION
The optic nerve is the only central nerve in the human body that can be directly observed.The pRNFL is formed by the convergence of axons from retinal ganglion cells that travel upwards into the brain.The blood supply to the optic disc consists of superficial and deep layers.The superficial layer from the central retinal artery, which nourishes the surface nerve fiber layer.And the deep layer from the posteriorciliary artery, which nourishes the anterior cribriform plate of sclera, cribriform plate of sclera and posterior cribriform plate of sclera.Neurological and vascular degeneration in the brain of PD patients can spread down the optic nerve to the retina, resulting in abnormalities in the morphology and function of the retinal nerve fibers and vascular network[8-10].It has been found that decreased dopamine concentrations and pathological α‐syn deposition in the retina and retinal vessel wall in PD patients[11].α‐syn activates microglia and releases pro‐inflammatory factors that causes neurological and vascular inflammatory responses.α‐syn will also disrupt lysosomal function, leading to an imbalance in iron homeostasis and causing cytotoxic damage to the retina[12-13].The mammalian retina has extremely high oxygen requirements.Mitochondrial dysfunction in PD patients, such as mitochondrial DNA mutations and deletions, will severely affect the retinal oxygen supply[14].The above pathological process will damage the optic nerve, resulting in a reduced ability of the optic nerve to transmit visual information to the brain, and this upstream nerve damage will exacerbate the progression of PD[15].As a non-invasive imaging technique, OCTA can rapidly measure and analyze pRNFL thickness and blood flow to evaluate the degree of optic disc neurofibrillary cell loss and vascular degeneration in PD patients.OCTA is a novel biomarker for predicting the progression of PD in the brain and has good research potential.
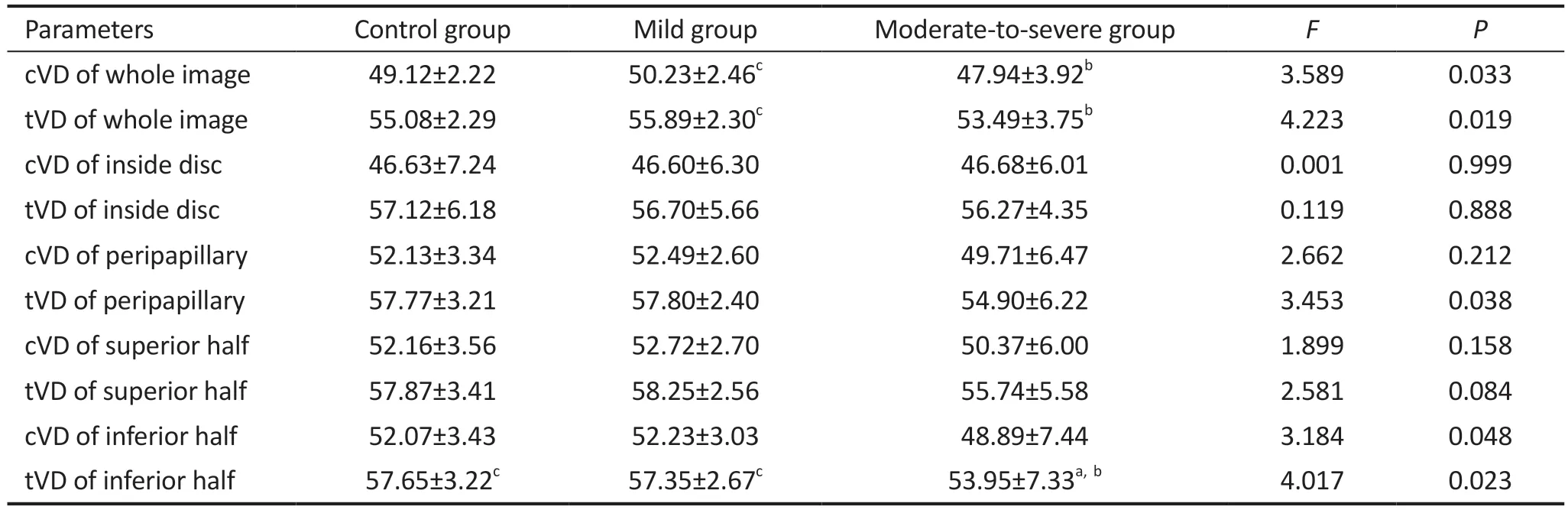
Table 5 Comparison of pVD parameters in different groups mean±SD

Table 6 Comparison of pVD parameters in eight quadrants in different groups mean±SD
Our study initially investigated the changes in pRNFL thickness and pⅤD in mild group and moderate‐to‐severe group of PD patients based on H&Y stage.There were significant differences in pRNFL thickness in average, superior half, inferior half, SN, NS, IN, IT, and ST quadrants among the three groups.It showed a tendency for the pRNFL thickness to become progressively thinner as the condition worsened.In PD group, the pRNFL thickness in average, superior half, inferior half, NS, and IT quadrants were negatively correlated with the H&Y stage and the UPDRS-III score, respectively.The pRNFL thickness in IT quadrant had the highest correlation with H&Y stage and UPDRS-III scores.
Huanget al[16]performed a Meta-analysis of pRNFL thickness in PD patients and the results showed that the thickness of pRNFL decreased globally in four quadrants.The degree of pRNFL thinning was larger in the inferior quadrant than that in superior quadrant and larger in the temporal quadrant than that in the nasal quadrant.The thinning of pRNFL followed a specific pattern, with inferotemporal thinning most common.Zhouet al[17]conducted a Meta-analysis of 36 observational studies and found that there was a global decrease in the thickness of all four quadrants of the pRNFL (superior,inferior, nasal, and temporal), with the largest effect in the inferior quadrant.Satueet al[18]observes PD patients over a 5-year follow-up period.PD patients had thinner pRNFL in the superior and inferior temporal quadrants compared to controls at baseline.After 5y, those patients had greater thinning of the pRNFL in the inferior temporal quadrant, and there was a moderate correlation with the degree of progression of H&Y stage.Jiménezet al’s[19]study showed a negative correlation between the total UPDRS score, disease duration, and average pRNFL thickness in PD patients, respectively.And they proposed a regression equation that predicts the total UPDRS score of PD patients using pRNFL thickness.The results of the above experiments were similar to the present study.The results all showed a significant decrease in the pRNFL thickness in inferior half and infratemporal quadrant with the progression of PD disease.In fact, the density of axons in ganglion cells around the optic disc is heterogeneous.Nerve fibers in the temporal side of the optic disc are mainly derived from retinal ganglion Parvo cell (P-cells).P-cells are primarily responsible for visual acuity, color discrimination and high spatial frequency chromatic/achromatic contrast sensitivity.These fibers are thinner nerve bundles and susceptible to mechanical damage.This also suggests that the significant thinning of the pRNFL in temporal quadrant may be the pathological basis for the various visual symptoms of PD patients.La Morgiaet al[20]proposed that PD damage to the optic nerve is similar to mitochondrial optic neuropathy, preferentially involving the papillomacular bundle.The papillomacular bundle enters the temporal and inferior halves of the optic disc,which suggests that the thinning of the pRNFL thickness in temporal and inferior halves in PD patients may be related to mitochondrial dysfunction[20].Mitochondrial dysfunction is an important factor in the development of PD disease[21].This also confirms the conclusions drawn from the pRNFL thickness correlation analysis in our study.
However, some scholars have suggested different views.Schneideret al[22]performed OCT measurements on PD monkeys, and found that the models had thinning pRNFL thickness in nasal and inferior halves compared to normal group.Baeket al’s[23]and Chorosteckiet al’s[24]studies found no statistical difference in pRNFL thickness in average and all quadrants of PD patients compared to normal people.Conclusions vary from study to study, possibly due to differences in race, number of subjects,age, disease duration, symptoms and measurement instruments,which can lead to significant differences in findings.
The quadrant of pRNFL thinning varies by disease in studies of OCT measurements of other neurodegenerative diseases.Chanet al[25]used OCT to measure pRNFL thickness in patients with Alzheimer’s disease and found that pRNFL thickness decreased more significantly in superior half than in inferior half, and similarly in nasal and temporal sides.Gulmez Sevimet al[26]found that pRNFL thinning was most significant in superior half in patients with progressive supranuclear palsy compared to PD patients.Another study analyzed pRNFL thickness in patients with multiple system atrophy and found a significant decrease in pRNFL thickness on nasal side compared to temporal side[27].These results are significantly different from the quadrant of pRNFL thinning that we obtained for PD patients.The measurement of pRNFL thickness may be an effective method for distinguishing PD from other neurodegenerative diseases in early stages.
Ⅰn the second part, we analyzed the tⅤD and cⅤD parameters of the optic disc of PD patients.With the increase in severity of the disease, the cⅤD and tⅤD of whole image, peripapillary,superior half, the cⅤD of inferior half, the NS, NⅠ, ⅠT, and TS quadrants in PD patients increased at first in mild group, and then decreased in moderate-to-severe group.However, the cⅤD of peripapillary, NS and ⅠT quadrants, the cⅤD and tⅤD of superior half did not show statistical differences.Correlation analysis showed that the tⅤD of whole image, the cⅤD of NI and TS quadrants were negatively correlated with H&Y stage, respectively.The cⅤD of TS quadrant was negatively correlated with UPDRS‐ⅠⅠⅠ scores.The cⅤD of TS quadrant had the highest correlation with H&Y stage and UPDRS-III score.
According to Robbins, α‐syn deposition in the retina of early PD patients causes increased neuroinflammation and vasodilatory mediators, resulting in increased compensatory raclial peripapillary capillary (RPC) blood flow.As the disease progresses, this compensation becomes increasingly dysregulated, with loss of RPC function and a decrease in vascular density, both of which contribute to neurodegeneration.This vicious circle leads to a thinning of pRNFL thickness and a decrease in RPC density[28].Our findings show a trend of increasing and then decreasing pⅤD, this hypothesis can be used to explain our results.There are few studies on pⅤD in PD patients, and the results are inconsistent.Linet al[29]divided PD patients into early-stage (H&Y stage I) and moderate-stage (H&Y stages II and III) subgroups.The results showed that the RPC density of the early-stage group was the highest, the control group was the second, and the moderate-stage group was the smallest.Xuet al[30]divided the PD patients into three groups according to H&Y stage and measured the pⅤD of all subjects.The results showed that the pⅤD of PD group was not statistically different from that of normal group, and there was no statistical difference between PD subgroups when compared with each other.Possible reasons for the difference in results are the small sample size of this study and the different parameters and analysis modes of the different instruments, resulting in experimental errors.Ⅰn our results, both the cⅤD and tⅤD of optic disc were abnormal, suggesting that PD affects both the RPC and the optic disc large vessels.The pⅤD of inside disc did not show a tendency to increase and then decrease,probably related to the distance between the vessels and the optic disc.The reduction in blood flow causes the distant vessels to constrict first, so the pⅤD of peripapillary changes first compared to the pⅤD of inside disc[31].
This study concludes that the thickness of pRNFL in PD patients is significantly decreased, and it is negatively correlated with H&Y stage and UPDRS‐Ⅲ score.With the increase of the severity of disease, the pⅤD parameters of optic disc in PD patients increased at first in mild group, and then decreased in moderate-to-severe group, and negatively correlated with H&Y stage and UPDRS‐Ⅲ score.Our research was a cross-sectional study with a small sample size in each group that did not assess visual function or follow up on the subjects.Therefore, we were unable to derive longterm patterns, sequences and specific mechanisms for changes in pRNFL thickness and pⅤD.The majority of patients with severe PD have a significant resting tremor and have difficulty with eye examination.In our study, the number of PD patients with H&Y stage 5 was small.In addition, the drug use of PD patients was not considered in this study.In subsequent studies, we will conduct a large sample, multi-centre, longterm observational follow-up data collection to improve the accuracy of the results, as well as increase the number of ophthalmic examinations for PD patients and further statistical analysis of the effect of the type and dose of medication used in PD patients on retinal parameters.
In conclusion, OCTA can be used to detect changes in pRNFL thickness and pⅤD in PD patients at various stages.OCTA may become a novel, quantitative biomarker in the future.OCTA can be used to diagnose, differential diagnosis and track the progression of PD.In addition, there may be a correlation between the mechanisms of neurological and vascular damage of the optic disc in PD patients, and further experimental exploration is needed.
ACKNOWLEDGEMENTS
We thank all the volunteers (both PD patients and normal controls) for their contributions to this study.
Conflicts of Interest: Yang TY,None;Zhang TQ,None;Xie LQ,None;Zhang Y,None;Liu SM,None;Zeng XW,None;Luo WF,None;Xu GX,None.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Analysis of retinal arteriolar and venular parameters in primary open angle glaucoma
- ldentification and functional analyses of a novel FOXL2 pathogenic variant causing blepharophimosis, ptosis,and epicanthus inversus syndrome
- Protective effects of ferulic acid against ionizing radiation-induced oxidative damage in rat lens through activating Nrf2 signal pathway
- Novel homozygous ADAMTS17 missense variant in Weill-Marchesani syndrome
- Cost analysis of childhood glaucoma surgeries using the US Medicaire allowable costs
- Predicting the prognosis of primary orbital lymphoma by clinical characteristics and imaging features
