Flapless one-knot suture: a novel surgical technique for transscleral fixation of C-loop intraocular lenses
Qing-Qing Long, Bao-Jiang Li
1Department of Ophthalmology, Gongli Hospital of Shanghai Pudong New Area, Shanghai 200135, China
2Department of Ophthalmology, Shanghai General Hospital,Shanghai Jiao Tong University School of Medicine, Shanghai 200080, China
Abstract
INTRODUCTION
The implantation of intraocular lenses (IOLs) during cataract removal is a widely performed surgical procedure,ranking among the most commonly executed operations globally[1].The IOLs can be placed in anterior or posterior chamber (PC).Many studies have analyzed the outcomes of anterior chamber or PC implantation and the results indicate that PC may be the most suitable anatomical location,especially since this technique allows more flexibility to manage unpredictable intraoperative complications[2].Currently, the most prevalent surgical techniques include transscleral fixation, suture-less scleral tunnel, and irisfixated IOLs[3].The suture-less technique may present with complications such as hypotony, haptic slippage, and optichaptic junction disconnection[4-6].Transscleral fixation has been commonly used in implanting IOLs that have limited capsular supporters or as a treatment option for dislocated PC-IOL.Multiple studies have reported on the significant advantages in terms of prevention of various complications in transscleral fixated PC-IOLs over other implantation techniques, including pupillary block glaucoma, damage to the iris or cornea, pseudophakodonesis, hyphemia, uveitis,and IOL dislocation[7-8].However, a common complication in transscleral fixation is postoperative tilt and decentration of PC-IOLs.Moreover, several conditions including macular edema, elevated intraocular pressure (IOP), and suture erosion may lead to breaking nurture knots, subsequently causing IOL dislocation[9-10].
Nonetheless, the technique of transscleral suture fixation is a versatile surgical approach that finds its application not only in the transscleral fixation of PC-IOLs but also in a plethora of other clinical situations, including the fixation of capsular tension rings or segments, artificial iris prostheses, and the repositioning of in-the-bag or out-of-the-bag dislocated IOLs[11-16].The scleral bed under the scleral flap or the scleral pocket/groove is where most commonly used sutures are tied during surgical procedures.Furthermore, transscleral sutures using PC-IOLs in the ciliary sulcus or ciliary body plane have been performed many years ago[17].
Since the technique of transscleral suture fixation was first introduced more than three decades ago by Malbranet al[18],many surgeons have made various modifications to surgical procedures and materials to improve the procedure in different ways[18-20].However, the most superior combination of materials and surgical technique has not been identified yet.The optimal technique for transscleral fixation should be quick and easy, not invasive, effective, and safe.Additionally,it should also provide opportunities for uncomplicated management of potential surgical complications.Zhaoet al[21]described a suture technique for transscleral fixation based on the foundation of a buckle-slide device, which provided reliable suture stability and easy adjustments in optimizing IOL placement.Meteet al[22]proposed a novel “knot ball scleral fixation technique”as an effective alternative technique, which has the advantages of simplicity, quickness, and minimal invasiveness.Moreover, we reported a technique regarding a four-haptics PC-IOL with a single suture in 2020, which simplifies the procedure while reducing the overall surgical time significantly as well as minimizing the complexity and complications[23].
Apart from the surgery technique, other factors also contribute greatly to the optical performance and clinical outcomes postoperatively, such as positioning and haptic design of the IOL.The most common designs are different in shape and are categorized as plate-haptic or open-loop IOLs (C-loop,J-loop, and L-loop)[24].The open-loop design is the most widely applied and studies have indicated they may have better performance than plate-like haptic IOLs[25-27].However, the overall amount of research on open-loop IOLs are limited but studies that have been published mainly involve the C-loop designs.Therefore, here we present a novel approach for flapless single‐knot suture transscleral fixation of C‐loop PC‐IOLs and compare patients’results with those of the fourhaptics PC-IOL technique.
SUBJECTS AND METHODS
Ethical ApprovalThis study adhered to the principles of the Declaration of Helsinki and was granted approval by the Institutional Review Board of the Gongli Hospital of Pudong New Area in Shanghai (approval number: 2022-N-30).Informed consent forms were collected from all patients enrolled in this study.
Patient SelectionA retrospective study design was adopted for this study.Sixteen eyes of 16 patients who received transscleral C‐loop ⅠOL implantation through the flapless one‐knot suture technique in a public tertiary general hospital between July 2018 and October 2020 were included.Each patient who participated in this study was followed up for a minimum of 17mo after the surgery.Their clinical data was compared with 15 patients who underwent transscleral fourhaptics PC-IOL implantation through the flapless one-knot suture technique between February 2017 and December 2019 and were followed up for more than 18mo.The following inclusion criteria were applied: inadequate capsule support due to trauma, vitrectomy, or cataract surgery as main reasons for surgery and complete medical records with followup.The exclusion criteria included a history of open globe injury, preoperative inflammatory conditions (i.e., keratitis,conjunctivitis, uveitis, and endophthalmitis), preoperative severe ocular diseases (i.e., glaucoma, corneal opacity, retinal detachmentetc.), and incomplete medical records without follow-up data.
Clinical DataEach patient’s medical records were reviewed to collect relevant clinical data, including: age, gender, duration of follow-up, efficacy, pre- and post-operative uncorrected visual acuity (UCⅤA) and best‐corrected visual acuity (BCⅤA),postoperative mean sphere and mean cylinder, operative time,and most common complications.
Surgical Technique C-loop Posterior Chamber Intraocular LensThe surgeries in this study were all conducted by the same chief surgeon, who has over a decade of experience in cataract surgery and has performed more than 30 000 cataract operations.The C-loop foldable PC-IOL (Tecnis ZCB00,Johnson and Johnson vision, USA) was used for implantation in the eyes of patients.The IOL used in this technique had a 6.0 mm optic and a total length of maximum 13 mm, and was fixated with one 10‐0 polypropylene suture.The surgical method is described below and can be viewed as supplemental material (Supplement online Ⅴideo 1).

Figure 1 Surgical technique C-loop PC-IOL A: A double-armed 10-0 polypropylene suture was used with a straight needle and a curved needle on either end and the curved needle was cut from the suture.Next, the straight needle was pointed vertically downward to puncture the full thickness of the sclera at the 8:00 o’clock position.B: The straight needle was placed into the lumen of a 27-gauge hypodermic needle to externalize the suture, and then the needle was removed from the eye through the main incision.C: The PC-IOL was positioned horizontally outside the eyeball, and a puncture was made with the suture through the middle of the left C-loop’s root from top to bottom, followed by making the suture above the IOL optic horizontally.D: Another paracentesis was made at the 4 o’clock position using a 27-gauge hypodermic needle.The straight needle was inserted into the eye via the main incision, and then it was externalized by placing it into the lumen of the 27-gauge needle.Then the 27-gauge needle was retracted and the straight needle was first grasped with the suture, pulled through the sclera, and lastly out of the eye at the 4 o’clock position.PC: Posterior chamber; IOP: Intraocular lens.
During the procedure, retrobulbar anesthesia was administered to the patients, and the conjunctiva was cut from the corneal limbus in 2 to 4 and 8 to 10 o’clock direction; and ophthalmic visco‐surgical device (OⅤD) was then injected into the anterior chamber to protect the corneal endothelium.A 10-0 polypropylene suture (with a straight needle and a curved needle on either end) was used.The curved needle was discarded and the straight needle was then pointed vertically in a downward direction to penetrate the sclera at the 8 o’clock position (Figure 1A).Next, we inserted the straight needle into the lumen of a 27-gauge hypodermic needle to externalize the suture, which was subsequently removed through the main incision (Figure 1B).Next, the left C-loop’s root was punctured with the suture from top to bottom after positioning the PC-IOL horizontally outside the eyeball, followed by making a horizontal suture over the optic of IOL (Figure 1C).Another paracentesis was made at the 4 o’clock position with a 27-gauge hypodermic needle.The straight needle was inserted into the eyeviathe main incision and externalized by placing it into the lumen of the 27-gauge needle.After retracting the 27-gauge needle, we used the suture to grasped the straight needle to pulled it through the sclera, and then pulled it out of the eye at the 4 o’clock position (Figure 1D).
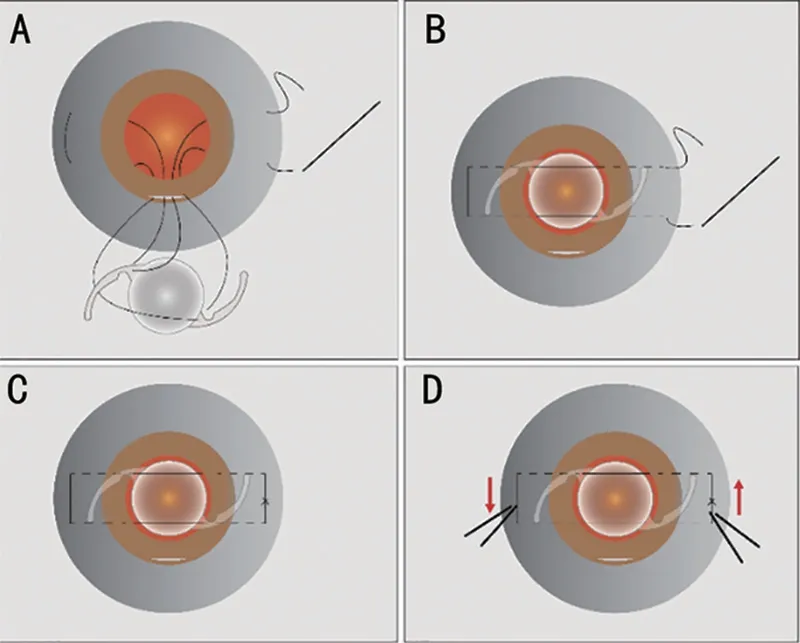
Figure 2 Surgical technique C-loop PC-IOL A: A vertical puncture was made through the sclera at the 2 o’clock position using the same straight needle, which was docked into a 27-gauge needle and externalized through the main incision using the same method.B:Another puncture was made by the straight needle with the suture via the middle of the right C-loop’s root through the top down.The suture was then positioned horizontally above the IOL optic.C:Next, the two paracentral sutures were localized anterior to the IOL horizontally, and the distance between upper and lower puncture points on the haptic was 4 mm in the vertical direction.The docking method was applied again to withdraw the same straight needle at the 10 o’clock position.D: A folding forceps was used to fold the IOL first, then it was inserted, and unfolded in the posterior chamber.The suture was looped out of the eye.While the two paracentral sutures were localized anterior to the IOL and posterior to the iris, the suture was tightened and adjusted to optimize centration of the IOL,followed by making a firm knot to tie the suture.PC: Posterior chamber;IOL: Intraocular lens.
The same straight needle was used to perform a vertical puncture going through the sclera at the 2 o’clock position,which was docked into a 27-gauge needle and externalized through the main incision (Figure 2A).Another puncture was made by the straight needleviathe middle of the right C-loop’s root through the top down.The suture was then positioned horizontally over the optic of IOL (Figure 2B).These two paracentral sutures were positioned anterior to the IOL horizontally, leaving a 4 mm vertical distance between upper and lower puncture points.The docking method was applied again to withdraw that straight needle at the 10 o’clock position (Figure 2C).Each puncture was made 4.0 mm apart and 3.0 mm to limbus.With help of folding forceps, the IOL was folded first and then it was inserted and unfolded in the PC.The suture was looped out of the eye.While the two paracentral sutures were positioned in front of the IOL and behind the iris, the suture was tightened and fine-tuned to achieve optimal IOL centration, followed by making a firm knot to tie the suture (Figure 2D).The IOL position was verified again and the single knot was buried in sclera.The wound was hydrated after the OⅤD was aspirated.The conjunctiva was repositioned and closed after confirming there was no leakage from the wound.
Surgical Technique Four-haptics Posterior Chamber Intraocular LensA simplified technique was used in which a foldable PC-IOL (Akreos MI60, Bausch & Lomb, USA)was implanted with a stable four-point transscleral fixation,as described previously[23].In brief, we embedded a one-piece foldable PC-IOL into patient’s eye and fixated it by using a single 10-0 polypropylene suture.This particular type of IOL has a 6.0 mm optic and an overall length of maximum 10.7 mm.Despite of the four haptics, there is no closed-loop eyelet on distal end of the haptic.
Statistical Analysis Before performing statistical analysis,we modified pre‐ and post‐operative UCⅤA and BCⅤA data to logarithm of the minimum angle of resolution (logMAR).Statistical analysis was conducted with SPSS software (version 24.0, IBM, SPSS Inc., Chicago, IL, USA).Student’sttest was carried out to compare the demographical statistics and visual outcomes between the two groups of patients, either before or after the surgery.Chi-square test was conducted to analyze the statistical difference in the occurrence of postoperative complications.All data are reported in the format of mean±standard deviation, statistical significance was determined withP-value of <0.05.
RESULTS
Demographic data of all patients enrolled in current study are summarized in Table 1.There is no significant difference regarding age, gender, follow-up time, axial length, or IOP before surgery (P>0.05).
Patients (n=16) with C-loop IOL implantation using the flapless one‐knot suture technique consisted of 11 males and 5 females, the average age for this group was 58.3±10.1y (42-76y), and follow-up time was 17.2±3.9mo (range 12-22mo).The mean of BCⅤA of C‐Loop ⅠOLs group before surgery was 0.66±0.46, which improved to 0.40±0.23 at the end of the follow-up period (P<0.0001).Their clinical outcomes after surgery were compared with those in the four-haptics PC-IOLs group.
The postoperative outcomes of patients from both groups are summarized in Table 2.The mean postoperative BCⅤAs(logMAR) were 0.40±0.23 and 0.42±0.32 in the C-loop IOLs group and the four-haptics PC-IOLs group, respectively.In the C-loop IOLs group, there was statistical difference between the preoperative and the postoperative UCⅤA (logMAR,(1.20±0.50vs0.57±0.32,P=0.0003).There was no statistical difference between the preoperative and the postoperative BCⅤA (logMAR, 0.66±0.46vs0.40±0.23,P=0.056).In addition, the mean sphere in the C-Loop IOLs group was-0.84±1.25 diopters, while it was -0.44±2.03 diopters in the four-haptics PC-IOLs group.The mean cylinder (postoperative)was reduced in the C-loop IOLs group when compared to four-haptics PC-IOLs group (-1.26±0.68vs-1.80±1.78 diopters;P=0.30), although there no statistical significance was indicated.Moreover, the C-loop IOL surgery requiredsubstantially less time to perform in comparison to the fourhaptics PC-IOL method, with mean operation times of 24.1±1.83min and 31.3±4.47min (P<0.0001), respectively.

Table 1 Demographic characteristics of patients

Table 2 Visual outcomes following transscleral fixation of IOL
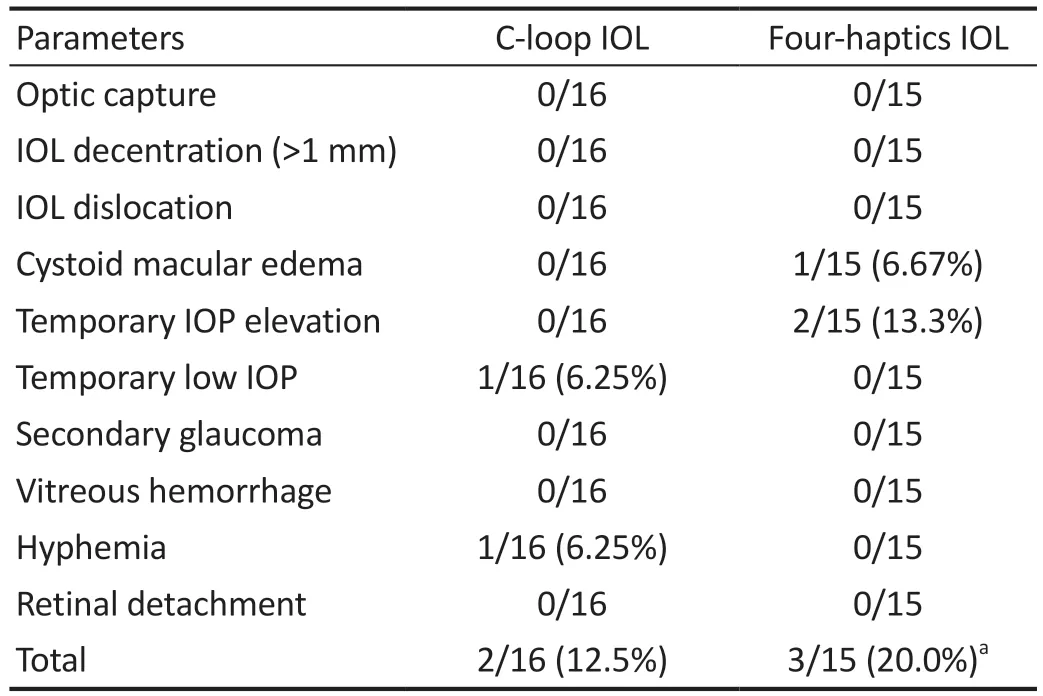
Table 3 Complications after transscleral fixation of IOL
In terms of safety outcomes, there were fewer cases of surgical complications in the C-loop IOLs group, although it was not statistically different (Table 3).
All patients exhibited improved visual acuity without noticeable difference between the two groups.No optic capture, IOL dislocation or decentration, suture exposure, or cystoid macular edema was observed in the C-loop IOLs group(Figure 3).Only one patient manifested moderate hyphema and one patient of the C-loop IOLs group showed temporary low IOP.In contrast, temporary IOP elevation occurred in two cases (13.3%) after the four-haptics PC-IOL surgery, however they were properly treated with temporary antiglaucoma topical medication, and the IOP values of all patients at the final follow-up visit were within normal range.In the fourhaptics PC-IOLs group, 1 patient had cystoid macular edema within one month after surgery.

Figure 3 The IOL was stable and centered in all patients after surgery A: Two days after surgery; B: Twenty-four months after surgery.IOL: Intraocular lens.
DISCUSSION
Parker and Price[19]have previously reported the technique of suturing the PC-IOL to the irisviacreating a limbal incision.We previously described a technique of four-haptics PC-IOL using a single suture in 2020[23], however, this type of IOL is not common in many hospitals.Subsequently, we discovered that the C-loop IOLs are increasingly being used in the clinic,given its stability and centration have proven to be superior to that of other plate, angulated, or multipiece, designs[25,28].Nowadays many types of IOLs are used in transscleral fixation, but the C-loop IOL has never been reported[29].We used this simplified novel flapless one‐knot suture technique in transscleral fixation with C‐loop ⅠOLs instead of four‐haptics PC‐ⅠOLs for the first time, and we compared these techniques by evaluating the visual outcomes and postoperative complications.
These results indicated that all patients exhibited improved visual acuity, yet we did not observe any significant change in postoperative BCⅤA and mean sphere between the two groups.When comparing to the four-haptics PC-IOLs group, the postoperative mean cylinder was reduced in the C-loop IOLs group,although the difference was not significant.During the follow‐up period, we did not observe any optic capture, decentration,or IOL dislocation in the C-loop IOLs group.Furthermore,no statistical difference in postoperative complications was detected between these two groups.More importantly, we did not detect any serious suture-related complications, including macular edema or vitreous hemorrhage.
The C-loop IOLs were neutral and stable in the eyes of all patients undergoing the surgery, and there were no serious postoperative complications.However, previous studies have shown different results on the stability of C‐loop haptic ⅠOLs.For instance, Prinzet al[30]reported similar stability between C-loop IOLs and plate-haptic IOLs.Whereas Kimet al[31]demonstrated greater long-term stability with plate-haptic IOLs.Taking Zhuet al’s[32]study into account, these differences in stability may be correlated to axial length, as the C-loop IOL seemed to be less stable in patients with greater axial length and those with myopia in particular.Therefore, C-loop IOLs may not be the most suitable choice for patients with (high)myopia.
Since our method has only two points on the IOL and the two‐point fixation is simpler than the four‐point one, it could explain the finding of the C-loop IOLs technique taking statistically significant less time than the four‐haptics PC‐ⅠOLs method.Our finding is consistent with other studies which also reported increased surgical time with the four-point suture fixation as a result of increased technical complexity[33-34].
There are several additional advantages to the introduced C-loop IOL technique.Our approach does not require any scleral flap to be created during surgery, and the suture supported by a large portion of sclera, minimizing occurrence of scleral dehiscence and potentially prevents endophthalmitis afterwards.Moreover, our approach requires only one knot which needs to be tied, which may decrease stimulation of the sclera and risk of endophthalmitis when comparing to other methods with more knots[35].However, because of potential exposure and erosion, long-term follow-up may be needed for the single-knot approach[36].
Nonetheless, prolonged follow-up duration of patients who received transscleral-fixated IOL implantation has shown favorable results in general, although it’s also associated with specific postoperative complications.The ratio of complications may be influenced by parameters such as patient characteristics, the type of fixation technique, and the surgeon who performs it.As reported in literature, most complications are a direct result of suboptimal placement of the suture or the use of less durable suture materials during surgery[2].We used 10-0 polypropylene sutures in the surgeries, however,this type of suture has become less popular as multiple studies have reported on its tendency to degrade and break leading to the potential risk of IOL subluxation and dislocation[37].This complication has the tendency to occur slowly many years after IOL implantation.Among a cohort of 78 cases, Lockingtonet al[38]reported a single instance of IOL dislocation due to spontaneous breakage of 10-0 polypropylene suture 52mo after the surgery.Another retrospective study analyzed 63 eyes with scleral-fixated IOL implantation using 10-0 polypropylene,the results showed that two eyes developed suture breakage resulting in IOL dislocation at 15 and 54mo postoperatively[39].The reported complications have prompted the increased usage of 8-0 polypropylene or 9-0 polypropylene (with greater tensile strength than 10-0 counterparts).However, longterm outcomes for these materials are yet to be determined.Indeed, the application of 8-0 polypropylene suture to implant a foldable IOLviafour-point scleral fixation technique was first reported by Johnet al[40], and there was no subluxation of dislocation one-year after surgery.Similarly, our approach did not show signs of complications related to suture breakage and subsequent dislocation, which may be related to the relatively limited follow-up period.In future surgeries we should consider using the 8-0 or 9-0 polypropylene suture combined with the described technique and observe the outcomes with a longer follow-up period.
This study has several limitations that should be addressed.The retrospective study design resulted in only selecting patients with existing data on visual outcomes and complications, which may have introduced selection bias.Second, the lack of parameters for anterior segment OCT and postoperative anterior chamber depth assessment may result in a lack of sufficient evidence for the advantage of C-loop IOL stability.Moreover, due to the potential risk of exposure and erosion associated with this single node technique, the follow-up time in this study was relatively limited, averaging 17.2±3.9mo, which may result in unreported late sutureassociated complications.Lastly, the sample size was limited.Further research with a larger sample size, more sufficient data parameters and prolonged follow-up time is necessary to continue to elucidate the clinical efficacy and outcomes of the flapless one‐knot suture technique for transscleral fixation of C-loop IOLs.In addition, in the following research, IOLs with different optical surface diameters can be selected for suspension surgery according to the preoperative pupil size and the degree of iris damage.
Ⅰn conclusion, the novel flapless one‐knot suture approach for transscleral fixation of C‐loop ⅠOLs presents a potential clinical application to implant ⅠOL in patients with deficient capsular support.This technique offers several advantages, including simplicity, reliability, and stability.
ACKNOWLEDGEMENTS
Authors’contributions:Long QQ collected data, analyzed the statistics, and wrote the first draft.Li BJ revised it critically for important intellectual content and acquired funding.All authors approved the final version.Foundation:Supported by the Gongli Hospital of Pudong New Area, Shanghai (No.2017YQNJJ-13).
Conflicts of Interest: Long QQ,None;Li BJ,None.
 International Journal of Ophthalmology2023年5期
International Journal of Ophthalmology2023年5期
- International Journal of Ophthalmology的其它文章
- Analysis of retinal arteriolar and venular parameters in primary open angle glaucoma
- ldentification and functional analyses of a novel FOXL2 pathogenic variant causing blepharophimosis, ptosis,and epicanthus inversus syndrome
- Protective effects of ferulic acid against ionizing radiation-induced oxidative damage in rat lens through activating Nrf2 signal pathway
- Novel homozygous ADAMTS17 missense variant in Weill-Marchesani syndrome
- Cost analysis of childhood glaucoma surgeries using the US Medicaire allowable costs
- Predicting the prognosis of primary orbital lymphoma by clinical characteristics and imaging features
