Manual and alternative therapies as non-pharmacological interventions for pain and stress control in newborns: a systematic review
Leva A. Shayani · Vera Regina F.da S. Marães
Abstract Background Supporting therapies that provide stress and pain control of preterm and term newborns infants contribute positively to the neuropsychomotor development.Non-pharmacological interventions that involve manual techniques are described,considering protocols that can be reproduced by physical therapists,with positive and negative outcomes reports.Data sources Systematic review follows PRISMA 2020 statements guidelines.Primary and specific health sciences databases(Science Direct,Pubmed,Scielo,Embase and Scopus) were consulted between October 2021 and May 2022.Articles considered were clinical trials,randomized or not,that included descriptions of the type of intervention as non-pharmacological and that studied the following outcomes: “pain” and “stress”.Results Fifteen articles were selected for analysis,reaching a methodological quality of at least 3 on the Jadad Scale for the Quality of Researched Sources.The non-pharmacological therapies most applied in isolation were massage,swaddling or wrapping,gentle touch and kinesthetic stimulation,and the combined therapies were non-nutritive sucking and swaddling,oral sucrose and swaddling,sensory stimulation and familiar odors,and sensory saturation.The outcomes found were relaxation,pain,and stress reduction after the application of painful procedures.The behavioral changes included crying,grimacing,yawning,sneezing,jerky arm or leg movements,startles,and finger flaring.The vital signs included heart rate,blood oxygen saturation level,and pulse respiration.Conclusions Combined techniques lead to better results in controlling neonatal pain when compared to isolated techniques.They can be applied both in preterm and term infants in a safe way and are reproducible in any health unit in a simple and economical way.
Keywords Newborn · Non-pharmacological interventions · Pain · Premature neonate · Stress
Introduction
The subject of pain and stress in neonates has begun to be explored in the last few years.It is known that the process of information of pain,which includes its path from local nociceptors,and its interpretation at cortical levels (prefrontal cortex,anterior cingulate cortex,insular cortex,and amygdala) as well as its efferent response,is present in preterm infants,even ifin an incompletely developed way.The selfregulation of pain will mature over the years and depends on the sum of lived experiences.Thus,the accumulation of stressful stimuli received by an infant will make it more hyper-responsive to pain in the future.Preventive measures should be taken to reduce acute pain to avoid future hyperreactivity [1,2].
Preterm birth and exposure to numerous painful procedures in the intensive care environment have harmful consequences for brain development.The constant submission to acute pain and stress caused by the hyperalgesia of daily routine procedures during a period characterized by brain development makes infants susceptible to chronic pain,especially in preterm infants that may remain hospitalized for long periods [3].Stress and pain control is done by the autonomic nervous system (ANS),still immature in preterm infants and directly influencing neurodevelopment,behavior,and long-term cognition [4].A therapeutic approach to provide adequate analgesia for brain protection is recommended [5].
Several non-pharmacological techniques are used to control pain and stress in preterm newborns (PTNB) and term newborns (TNB);these techniques may help in the maturation of the ANS and thus in self-regulation of pain management in the long term [6].Kinesiotherapeutic exercises,through passive movements [7],therapeutic massage of the trunk and extremities [8] and functional positioning simulating the uterine environment with the use of tissues and rollers are some techniques described for PTNB and TNB [2].These techniques have a great influence on neuropsychomotor development and on social,emotional and physical well-being,besides producing relaxation and pain and stress reduction effects [9].
Pain control through pharmacological interventions,such as opioids and alpha-2-agonists [5,10],has been growing in recent decades and implies high costs to health institutions.These inhibit pain afference at the medullary level and activate pain inhibiting descending cortical pathways.However,the disadvantages are side effects to the immature organism,especially when used for a prolonged time.In addition to analgesia,pharmacological interventions can cause respiratory depression,urinary retention,nausea,vomiting,different degrees of tolerance and physical dependence [11].Studies also indicate worse neurological prognostics,such as an increase in the frequency of peri-intraventricular hemorrhage,periventricular leukomalacia and/or death in preterm infants of extreme low birth weight [12].
Worldwide recommendations cite non-pharmacological measures to aid pain control,including interdisciplinarity in the identification and management of pain.The National Institute for Drug Abuse (NIDA) considers these measures necessary and the most appropriate for pain control.However,there is still a lack of evidence on the best management and best strategies [13].In 2021,the Joint Commission (TJC),considered the largest hospital organization in the USA,published a document reviewing the management of pain in patients through non-pharmacological measures,such as physiotherapy,muscle relaxation,and massotherapy,among others.This document aimed to reduce hospital costs,side effects and patients' dependence on drugs [14].
Thus,the objectives of this systematic review are to select the best non-pharmacological methods for pain and stress control in preterm newborns and term newborns,involving manual techniques,alone or in combination;to identify and describe care protocols that can be reproduced,while reporting positive and negative variables after their application;and to assess whether there have been changes in the methods used in recent studies,given that this is still a relatively unexplored subject.
Methods
The study followed a protocol based on the PRISMA 2020 check list (Preferred Reporting Items for Systematic Reviews and Meta-analyses) [15].This review was not registered.The criteria in the selection of articles for the assessment of manual techniques in newborns (NBs) were: (1) a wide search for articles,with a sensitive search strategy (descriptors of varied terms) in different recognized databases;(2) an assessment of the quality of the studies included by means of minimum variables (Jadad);(3) noting whether the search,selection,and extraction of data were made by two independent researchers;(4) if meta-analytical techniques were used adequately for data analysis [16].
Search strategy
The search for articles was conducted between October 2021 and May 2022.Primary and specific health sciences databases (Science Direct,Pubmed,Scielo,Embase,and Scopus) were consulted.The descriptors were based on the DeCS/MeSH (Health Sciences Descriptors) website: “motor stimulation”,or “tactile stimulation”,or “tactile-kinesthetic stimulation”,or “sensory stimulation” or “therapeutic touch”or “therapeutic massage” and “pain” or “stress” and “premature newborns”,or “premature infant”,or “extremely premature” or “preterm infant”,or “preterm birth” or “term baby” or “neonate”.The conjunctions “and” and “or” (or)were used to restrict or join the search descriptors.
Inclusion criteria
Preterm newborns [gestational age (GA) of less than 37 weeks] and term infants (between 37 and 42 weeks of life) of both sexes and hospitalized in a neonatal intensive care units (NICU) were included.Studies with a randomized or a non-randomized clinical trial design that correlate various forms of motor intervention with a “pain” or“stress” outcome,with a sample size of at least 10 NBs,were selected.The languages of the articles: English,Spanish,Italian,and Portuguese.Publication period is from January 2007 to May 2022.Exclusion criteria were case studies,quasi-experimental studies,qualitative articles,and animal studies because these may compromise the comparison between studies.
Selection process
The studies were selected taking into account the date of publication,the methodology,the type of intervention and the outcomes analyzed.One evaluator performed the first search,and a second evaluator consented to the choice.If there were differences of opinion regarding an article,it was not used.
Quality of the study
After the initial selection of scientific articles,the Jadad Scale for the Quality of Researched Sources was applied as an automation tool.It consists of scores given in response to three questions: (1) was the study randomized? (2) was there masking of the investigative process? (3) was there clarification as to the disposition of the patients included in the trial? Articles with a score greater than or equal to 3 in a rating of 0–5 were elected [16].A non-quantitative synthesis of the extracted data was performed.
Results
Selection of studies
Initially,97 articles were found.After refinement of the search among titles,abstracts and full texts,15 articles were selected for analysis because they met all inclusion criteria,being non-pharmacological methods of pain or stress control in NB (Fig. 1).

Fig.1 Selection of studies for inclusion in the systematic review
Characteristics of the study
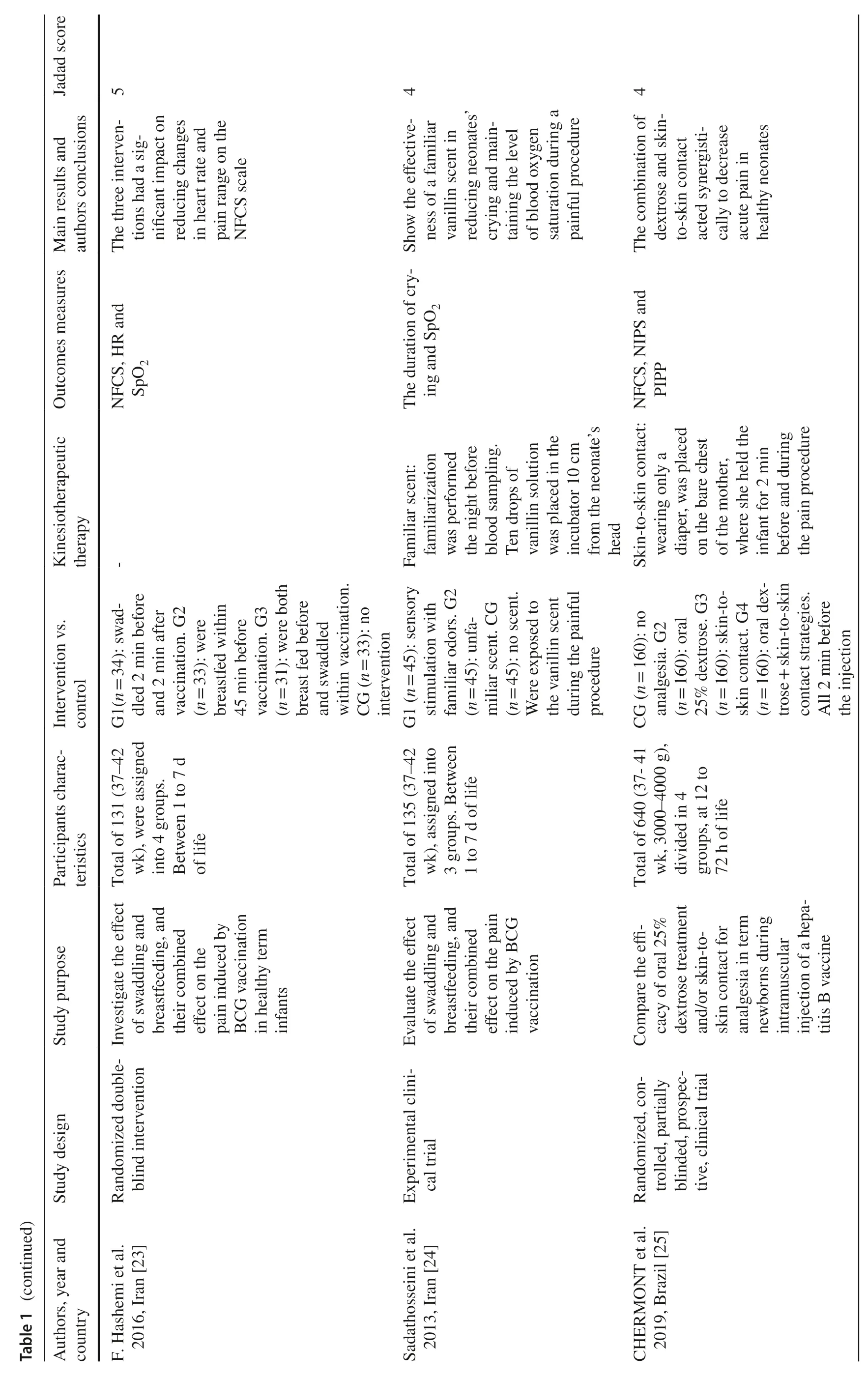
Totally 15 articles were selected,including 13 randomized clinical trials,1 clinical trial,and 1 experimental study,9 with control groups.The studies were conducted in six countries between 2007 and 2021.In the introduction and objectives of the articles,we sought a description of the short-and long-term benefits.Therapies were evaluated before and after the painful procedure to assess their effi-cacy.The articles selected used manual therapies aimed at relaxation [17,18] and reduction of pain and stress[19–29] during painful procedures.The painful procedures mentioned were heel puncture [17,26],venous puncture[21,22,24,27],and vaccination [23,25].A meta-analysis was not performed because the included studies did not follow the same statistical criteria and were not sufficiently homogeneous.
Non-pharmacological therapies assessed
The most widely used non-pharmacological therapies were massage [19,30,31],varied neuropsychomotor stimuli[21,22,24,25],swaddling in cloth [17,18,23,26],electrostimulation [32],and a combination of techniques [17,21,27–29].
Pain assessment instrument
The main behavioral alterations observed in this review were crying;facial expressions,such as grimaces,yawns and sneezing;body movements,such as flexion and extension of limbs;and muscle tone [30].The main vital signs assessed were heart rate,respiratory rate,peripheral oxygen saturation,and blood pressure [17,18,24,31–33].The main behavioral scales were Preterm Infant Pain Profile (PIPP) [18,22,27,28,32],introduced by Stevens et al.,1996 [34];Neonatal Facial Affect Coding System (NFACS) [17,33],first described by Grunau et al.,1998 [35];Neonatal Facial Coding System (NFCS) [25];Children's Revised Impact of Event Scale (CRIES) [21],first described by Krechel &Bildner,1995 [36];Neonatal Infant Pain Scale (NIPS) [25,26],first described by Lawrence et al.,1993 [37];Comfort scale [18,26];Newborn Stress Scale (NSS) [29];and Neonatal pain agitation sedation scale (N-PASS) [28].Hormones were used as stress markers,such as cortisol [19,26,27] and melatonin [26].
Characteristics of the infants
A total of 2316 infants were included in this review: 771 preterm infants (ranging from 27 to 36 weeks of GA) and 1607 term infants (37 weeks or more of GA).Interventions began between 24 hours of life and seven days of life.
Effects of non-pharmacological therapies on pain in neonates undergoing painful procedures
The main effects reported in the studies were the reduction of pain and stress through non-pharmacological techniques performed before painful procedures,such as venous puncture,heel puncture,injections,and bath.It was noted that,in general,these interventions offer warmth to the baby and comfort it during pain-causing interventions,which was observed through the application of behavioral and pain scales.The variation of vital signs with the application of these non-pharmacological techniques is not yet significant when compared to the control groups (Table 1).



Discussion
Pain management in preterm newborns and term infants is a growing subject in recent decades.This includes from understanding neurobiological pain processing to identifying techniques for its control.Chronic pain,initiated from birth,is known to influence sensory processing and long-term pain sensitivity.In addition,it has a negative impact on quality of life,resulting in social and emotional consequences for the child and his/her family [38].
The aim of this systematic review was to find in the most recent literature on non-pharmacological techniques involving manual techniques,alone or in combination,to reduce pain and stress in newborns.Although there is no universal systematization of described techniques,it is possible to identify several interventions with positive effects.Generally,the technique chosen by a research group is based on the experience and routine in the sector itself.Table 2 represents the techniques identified in the study based on the selected literature.

Table 2 Techniques with positive effects in reducing stress and pain in newborns
Strategies described 15 years ago,as in the systematic review by E.Cignacco et al.,which had better results in hemodynamic variables (heart rate and blood oxygen saturation level) and included analyses of pain and stress scales,identified the following main techniques: swaddling (involving newborns in cloth),wrapping (positioning of the baby with restrained limbs),non-nutritive and nutritive sucking,music therapy,prone positioning,olfactory and multisensory stimulation,kangaroo,and maternal touch [39].Other methods,such as massage and motor stimulation through different forms of touch and joint movements,were introduced through randomized studies with positive results in the analysis of the same variables.
A comparison between massage and gentle touch showed that both techniques reduce stress levels in preterm infants,which was detected through cortisol levels in urine.This same study showed better outcomes in the massage group [19].The effects of the massage seem to last beyond the time when it is performed.M.Hernandez-Reif et al.showed that massaged preterm infants were less active and showed lower stress behavior from the first to the last day,suggesting that,over time,therapeutic massage has a stress-reducing or pacifying effect [30].In the study by Suna Dağ et al.,one notes that massage can be performed safely for relaxation and stress control in preterm infants,provided physiological variables are kept stable after its performance [31].
A review by Alvarez et al.evaluated the application of therapeutic massage;numerous benefits were reported,where stress reduction is the point most evidenced by the authors [8].In the systematic review by Fitri et al.,positive data were presented on reducing pain intensity with the application of massage in neonates submitted to procedural pain.However,there are various opinions as to the part of the body defined as ideal for massage application.The most cited are legs,trunk,back,arms,and nape [40,41].The intensity is from mild to moderate [42],where moderate is mostly preferred.The duration varies,from 2 to 30 minutes,with the predominance of 2 minutes [43,44] and 15 minutes [33,45].Massage can also be combined with another technique,such as non-nutritive sucking [33,46].
Electrostimulation at acupuncture points is a method introduced by Yates et al.for pain control in painful procedures in NB term infants.The study assessed the safety of this procedure and concluded that it can be used as an alternative for pain control [32].
Some authors attempt combinations of various methods of pain reduction during painful procedures.Leng et al.showed that more superficial punctures caused greater discomfort than deeper venous punctures,and the combination of sucralose,non-nutritive sucking and the swaddling of the newborn with cloths significantly reduces the pain variables assessed [17].Nasim et al.showed that multisensory stimulation,including cuddling,talking,touching,kissing,and eye-to-eye contact with the infant before bath reduced stress level when compared to the control group [29].Sharma and Samuel also found the same result while comparing two groups [multisensory stimulation (MSS) and soft tissue therapy (STT)] [28].The same effect was observed by Gomes et al.,who used an association of dextrose and skin-to-skin contact during a vaccination procedure and who observed a significant reduction in pain scores in infants [25].The combination of breastfeeding and swaddling during vaccination also led to significant results when compared to a control group [33].
A combination of therapies was applied by Qiu et al.2017,who compared stress levels in a venous puncture procedure among two groups,among which one received music therapy associated with gentle touch and the control group received only the painful stimulus.The combination of stimuli decreased the pain response of preterm newborns,improving the concentration of β-endorphin,but there was no change in cortisol concentration in the blood [27].
Studies have shown that sensory stimulation with familiar smells that recall their mothers or fetal life can reduce stress and bring calming effects by resolving responses,such as crying,and motor activity of neonates during painful procedures,such as heel puncture,or when separated from their mothers [24].These findings were confirmed by other authors,who describe that the baby already at birth is familiar with the odor of its mothers' milk.Breastfeeding itself can be considered during painful events [47].
Another proposed concept was sensory saturation,defined as a set of interventions done simultaneously to compete with pain during a painful procedure.The technique consists of performing tactile,auditory,olfactory,vestibular,visual and gustatory stimuli to increase the analgesic effect during a moment of pain.Positive results were observed both in preterm infants and in term infants,with similar effects when compared to the use of sedoanalgesia with drugs [21].This concept was confirmed by Locatelli and Bellieni,2018 [48].
Some examples of sensory saturation use were described by Bernardini et al.: auditory stimulus can come from the mother’s voice or the soft music of a music box;tactile stimulus can come from massage;visual stimulus from eye-to-eye contact with the mother by showing the infant contrasting colors (e.g.,black/white chessboard);olfactory stimulus from the smell of the mother's skin or from special creams and oils (e.g.,almond oil);gustatory stimulus from a glucose solution;and for vestibular stimulus,swinging the infant’s arms or hammock therapy [22].These techniques are easily reproducible in NICUs because they do not require sophisticated equipment or materials.
We note that most studies are conducted in preterm infants.This may be attributed to longer length of stay in hospitals because these infants have a lower pain threshold caused by a less effective modulation due to immaturity of the nociceptor paths and a more vigorous expression of pain[49].The expression of pain in NB can be seen through behavioral alterations (measured by pain scales) and physiological changes (measured through vital signs) [50].
The small number of controlled randomized and doubleblind trials make it difficult to conduct systematic reviews and meta-analyses,which becomes a limitation of the study.Such criteria are often not used due to inherent ethical concepts when involving human beings.Still another reflection among researchers is excluding control groups,which bring benefits already mentioned in the literature,to studies of therapies.
In this way,supporting therapies that provide stress and pain control of preterm infants contribute positively to the neuropsychomotor development.This acquired knowledge about non-pharmacological therapies is important for advances in areas of manual therapy in preterm infants.
In conclusion,the pain felt by neonates while hospitalized generates expectations regarding the solution of the problem in the entire multidisciplinary team,including physical therapists.Therefore,several non-pharmacological interventions,such as manual techniques,appear to offer comfort to these infants.This study was able to identify that combined techniques bring better results for the control of neonatal pain and stress compared to isolated techniques.They can be applied both in preterm and term infants in a safe way and are also reproducible in any health unit in a simple and economical way.Future studies that compare different combinations of techniques will help to standardize a global consensus.
Author contributionLAS: concepualization,data curation,formal analysis,writing–original draft,writing–review and editing.VRFdSM: concepualization,data curation,formal analysis,writing–review and editing.
FundingThis research did not receive funding.
Data availabilityData sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approvalNot necessary–systematic review.
 World Journal of Pediatrics2023年1期
World Journal of Pediatrics2023年1期
- World Journal of Pediatrics的其它文章
- Innovative treatments for congenital heart defects
- Perioperative extracorporeal membrane oxygenation in pediatric congenital heart disease: Chinese expert consensus
- Role of ultrasound in the treatment of pediatric infectious diseases:case series and narrative review
- Vitamin D therapy in pediatric patients with inflammatory bowel disease: a systematic review and meta-analysis
- Assessment of compatibility of rhIGF-1/rhIGFBP-3 with neonatal intravenous medications
- Development of necrotizing enterocolitis after blood transfusion in very premature neonates
