Multi-targeted anti-inflammatory drugs for the treatment of neurological disorders
Austin Lui, Omar Alzayat, Timothy Do, David Perekopskiy, Meghan Gann,Taiseer Saad Elgokhy, Jie Gao, DaZhi Liu
Inflammation and kinase pathophysiology in neurological disorders:
Inflammation is one of the common features of various acute and degenerative neurological disorders, such as stroke, traumatic brain injury (TBI), Alzheimer’s disease (AD), Parkinson’s disease (PD), and others.The inflammatory responses are manifested as the synthesis of inflammation mediators,recruitment of leukocytes, and other secondary injuries.Compelling evidence shows that a large number of inflammation mediators (e.g.,thrombin, reactive oxygen species, cytokines,chemokines, and other molecules) are implicated in the pathophysiological processes in neurological disorders (Liu and Ander, 2012) (Figure 1).These increased inflammation mediators stimulate their downstream transmembrane receptors (e.g.,protease-activated receptors, cytokine receptors,and others), and further activate the intracellular downstream effector kinases, such as Src family kinase, Rho-associated protein kinase, Jun N-terminal kinase, extracellular signal-regulated kinase, cyclin-dependent kinase (CDK), and others(Liu and Ander, 2012) (Figure 1).Aside from overlapping in different neurological disorders,numerous inflammatory molecules and multiple kinase-involved signaling pathways can be linked to a single neurological disorder such as AD(Heneka et al., 2015).Because of their pivot roles in the process of inflammation, kinases have been regarded as anti-inflammatory targets to improve outcomes of neurological disorders.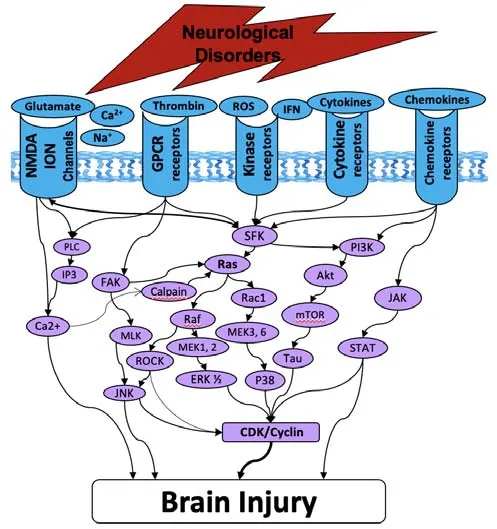
Figure 1|Diagrams of toxic upstream extracellular molecules, membrane receptors, and intracellular downstream kinases that are implicated in brain injury in neurological disorders.
An acute inflammatory response is typically seen in acute neurological disorders, just as chronic inflammation in neurodegenerative disorders.In acute brain injury, resident cells in the brain,such as astrocytes and microglia, are stimulated to produce proinflammatory cytokines, such as interleukin-1, interleukin-6, and tumor necrosis factor (Xiong et al., 2018).The blood-brain barrier then becomes more permeable, allowing peripheral immune cells, such as neutrophils and monocytes/macrophages, to enter, further exacerbating the initial neuroinflammatory response (Xiong et al., 2018).In chronic neuroinflammation, a similar cascade of events could also occur, while this is associated with the long-term release of inflammatory mediators from resident brain cells and peripheral immune cells,resulting in the perpetuation of neuroinflammation and chronic neurodegeneration (Chen et al.,2016).
In this perspective paper, we focus on the antiinflammatory efficacy of kinases inhibitors[particularly on the United States Food and Drug Administration (FDA)-approved multi-targeted kinase inhibitors], other than a large number of non-kinase anti-inflammatory drugs (e.g., nonsteroidal anti-inflammatory drugs, peroxisome proliferator-activated receptor antagonists, fatty acid amide hydrolase inhibitors, and others).
Kinase inhibitors in pre-clinical tests on neurological disorders:
Our recent study showed that combined inhibition of two Src family kinase subtypes (e.g., Src, Fyn) can improve pathological and neurological outcomes after TBI in rats, while inhibiting individual subtype Src or Fyn failed to do so (Ye et al., 2022).It is thought that Src and Fyn either directly or indirectly activate Rhoassociated protein kinase, which then directly or indirectly inhibits the cell cycle in neurons and ultimately prevented further neuronal cell death.These findings suggest that inhibiting multiple kinases have more robust efficacy than inhibiting a single kinase subtype.In addition to Src family kinase inhibitors, there is an extensive list of kinase inhibitors that have been reported to be experimentally effective on various neurological disorders (Liu and Ander, 2012).In terms of effective kinase inhibitors in TBI models, the kinase Rho-associated protein kinase inhibitor Y27632 was shown to improve the motor performance in mice after TBI, possibly by preventing neuronal cell death via indirectly arresting the cell cycle in neurons.Similarly, the Jun N-terminal kinase inhibitor SP600125 substantially reduced amyloid precursor protein expression level and amyloidbeta production after TBI in mice, possibly due to Jun N-terminal kinase’s role in amyloid precursor protein expression via BACE1 expression regulation and its role in also regulating secretase expression(Rehman et al., 2018).SP600125 also prevented inflammatory response (via decreasing expression of tumor necrosis factor, interleukin-1β, along with other inflammatory mediators), blood-brain barrier breakdown, neurodegenerative apoptosis(supported by attenuation of levels of Bcl2,extracellular signal-regulated kinase and protein kinase B), and protein loss in implicated synapses such as PSD95, SNAP23, and synaptophysin(Rehman et al., 2018).More evidence includes the extracellular signal-regulated kinase inhibitor PD98059 and CDK inhibitor CR8, which downregulated C-C motif chemokine ligand 2 and C-X-C motif chemokine ligand 1 expression in astrocytes, decreased neuronal apoptosis, and protected against neurodegeneration after TBI(Aubrecht et al., 2018; Huang et al., 2021).Translation failures of experimentally effective drugs from animal models to clinical trials:
In the drug development for neurological treatments(e.g., stroke, TBI, AD), hundreds of compounds that are effective in animal models have not led to any FDA-approved drugs, other than tissue plasminogen activator for stroke and aducanumab for AD under the accelerated FDA approval pathway.Nevertheless, tissue plasminogen activator benefits only a small portion of ischemic stroke patients, while aducanumab remains controversary mostly because of severe side effects (e.g., brain edema and headache) that pose a barrier in human use (Tampi et al., 2021).Since aducanumab was approved on the basis of reduction of the surrogate biomarker amyloid in the brain but not on the evidence of efficacy on clinical outcomes, Biogen, the company manufacturing this medication, has been required to conduct a new randomized control trial to verify the drugs clinical benefit (Dunn et al., 2021).In a multicenter randomized clinical trial of 159 participants with mild Alzheimer dementia,saracatinib (AZD0530) treatment showed evidence for slowing the rate of decrease in hippocampal volume and entorhinal thickness (van Dyck et al.,2019).However, there was no difference from placebo in slowing cerebral metabolic decline(van Dyck et al., 2019).Additionally, there were no treatment effects on the rate of change in cognition, function, and other biomarkers (van Dyck et al., 2019).The data of this clinical trial suggested that saracatinib can barely improve outcomes for AD patients.
Potential reasons for translational failures:
Regardless of acute or degenerative, most neurological disorders (e.g., stroke, TBI, AD)are heterogeneous with numerous molecules(including kinases) and pathways involved in their pathological processes (Figure 1).These have been supported by increasing genomic data,showing that numerous inflammatory genes are significantly increased in the blood and brain in neurological disorders.However, most current drug development efforts are based on the“receptor theory” of one ligand-one receptor binding style, which focuses on small molecules,with each molecule targeting a single gene,protein, or enzyme.Since injured tissue might die via many parallel pathways in neurological disorders, blocking just one target or pathway may not be effective.Moreover, it is uncertain which of those inflammatory kinases are increased in each patient with a certain type of neurological disorder, and thus the drugs developed based on the ligand-receptor module would lose efficacy in clinical trials when the drug-targeted molecule does not change as expected in a certain patient.Therefore, multi-targeted anti-inflammatory drugs would produce more robust therapeutic efficacy and could increase the success of clinical translation, as compared to those that only block a single target.Developing multi-targeted anti-inflammatory drugs for neurological treatment:
Developing multi-targeted anti-inflammatory drugs seems probably to be a solution for neurological treatment, as a single drug can simultaneously inhibit multiple kinases-involved pathologies of neurological disorders.Since every patient may have a different genomic profile for a certain type of neurological disease, the individual kinases that are abnormally activated may not be the same in all individuals.Therefore, to achieve maximal therapeutic results for each patient, a genomic screen will be needed for each individual with that disease.Personalized multi-kinase inhibitors can then be manufactured for each patient.This process appears extremely difficult and expensive at this time, but it is a vision of precision medicine.Putting cost considerations aside, genomic tailored medicine might be suitable for neurodegenerative diseases (e.g., AD), but not for acute neurological disorders (e.g., stroke, TBI) that typically require acute treatments within 3- or 6-hour therapeutic window after acute brain injury.Repurposing FDA-approved multi-targeted kinase inhibitors:
One cost-efficient approach is to repurpose FDA-approved multi-targeted kinase inhibitors for neurological treatment.The FDA has approved 74 kinase inhibitors by the end of 2021, with tens of them being multi-targeted.Imatinib is an example of a multi-targeted kinase inhibitor, as it has broad target coverage,including kinases of Abl, Kit, and PDGFR.In a phase 2 randomized trial (NCT03639922) for the treatment of ischemic stroke, it was found that administration of imatinib restored the bloodbrain barrier, reduced inflammation, and retained nutritional supply to the ischemia in question via the restriction of the invasion of cells from nearby blood vessels (Wahlgren et al., 2017), though there were no significant differences between the treatment groups regarding the absolute number of hemorrhagic transformations that occurred(Wahlgren et al., 2017).Unlike acute brain injury in which a single acute drug administration could improve outcome measures, neurodegenerative disease (e.g.,AD) often requires repeated and chronic drug administration.In a small phase 2 trial(NCT02947893), amyloid accumulation was slowed in the frontal lobe of the AD patients after six months of treatment with nilotinib (a specific kinase inhibitor on Abl), but no differences were observed in exploratory clinical, cognitive,functional, or behavioral measures.In another randomized phase 2 study (NCT00976118),masitinib (a multi-targeted kinase inhibitor of Kit, Lyn, and PDGFR) showed a positive trend to reduce cognitive decline at 24 weeks in patients with mild to moderate AD compared to placebo.It seems that the use of kinase inhibitors to treat neurological disorders in the past clinical trials has yielded a limited improvement in cognitive outcomes, but we can extrapolate that efficacy limitations in clinical outcomes may predominantly be due to the high selectivity of certain kinases of these drugs.Even though there are multitargeted kinase inhibitors, their target spectrum might not be broad enough for the treatment of neurogenerative disorders.
Combination therapy can achieve broad inhibition of multiple inflammatory factors.There are several ongoing clinical trials of combination therapy for AD.One is a phase 3 clinical trial (NCT01872598),using a combination of masitinib with a cholinesterase inhibitor (donepezil, rivastigmine,or galantamine) and/or memantine.Another is a phase 2 clinical trial (NCT04685590), testing a combination of dasatinib (an FDA-approved kinase inhibitor of c-Src, Abl, c-Kit) with quercetin(a powerful antioxidant that people sometimes take as a supplement).However, there exist some challenges in combination therapy, such as drug interaction (which can affect the pharmacokinetics of each drug and have interactive toxic effects),economic, legal, and regulatory challenges(intellectual property and logistical obstacles), and others.
Conclusions:
In our perspective, repurposing a single FDA-approved multi-targeted kinase inhibitor would probably lead to new treatments for acute brain injury.The combination of two or three anti-inflammatory drugs would be a practicable alternative for the treatment of neurodegenerative diseases such as AD, before any new chemical entities that have broad-spectrum coverage on kinases and other inflammatory factors are developed.This work was supported by NIH/NINDS grants,No.R01NS089901 (to DZL) and No.R01NS114061(to DZL).
Austin Lui, Omar Alzayat, Timothy Do,David Perekopskiy, Meghan Gann,Taiseer Saad Elgokhy, Jie Gao,DaZhi Liu
Department of Neurology, University of California at Davis, Sacramento, CA, USA (Lui A, Alzayat O,Do T, Perekopskiy D, Gann M, Elgokhy TS, Liu D)Department of Neuroscience, The Ohio State University, Columbus, OH, USA (Gao J)
*Correspondence to:
DaZhi Liu, PhD,dzliu@ucdavis.edu.https://orcid.org/0000-0002-3934-9651(DaZhi Liu)
Date of submission:
May 4, 2022Date of decision:
June 27, 2022Date of acceptance:
July 12, 2022Date of web publication:
September 16, 2022https://doi.org/10.4103/1673-5374.353489
How to cite this article:
Lui A, Alzayat O, Do T,Perekopskiy D, Gann M, Elgokhy TS, Gao J, Liu D(2023) Multi-targeted anti-inflammatory drugs for the treatment of neurological disorders.Neural Regen Res 18(4):805-806.
Open access statement:
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License,which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- Potential physiological and pathological roles for axonal ryanodine receptors
- Roles of constitutively secreted extracellular chaperones in neuronal cell repair and regeneration
- Melatonin, tunneling nanotubes, mesenchymal cells,and tissue regeneration
- MicroRNAs as potential biomarkers in temporal lobe epilepsy and mesial temporal lobe epilepsy
- Notice of Retraction
- Emerging roles of GPR109A in regulation of neuroinflammation in neurological diseases and pain