Intranasal nerve growth factor for prevention and recovery of the outcomes of traumatic brain injury
Luigi Manni, Giorgio Conti, Antonio Chiaretti, Marzia Soligo,
Abstract Traumatic brain injury is one of the main causes of mortality and disability worldwide.Traumatic brain injury is characterized by a primary injury directly induced by the impact, which progresses into a secondary injury that leads to cellular and metabolic damages, starting in the first few hours and days after primary mechanical injury.To date, traumatic brain injury is not targetable by therapies aimed at preventing and/or limiting the outcomes of secondary damage but only by palliative therapies.Nerve growth factor is a neurotrophin targeting neuronal and non-neuronal cells, potentially useful in preventing/limiting the outcomes of secondary damage in traumatic brain injury.This potential has further increased in the last two decades since the possibility of reaching neurotrophin targets in the brain through its intranasal delivery has been exploited.Indeed,molecules intranasally delivered to the brain parenchyma may easily bypass the blood-brain barrier and reach their therapeutic targets in the brain, with favorable kinetics, dynamics, and safety profile.In the first part of this review, we aimed to report the traumatic brain injury-induced dysfunctional mechanisms that may benefit from nerve growth factor treatment.In the second part, we then exposed the experimental evidence relating to the action of nerve growth factor (both in vitro and in vivo, after administration routes other than intranasal) on some of these mechanisms.In the last part of the work, we, therefore, discussed the few manuscripts that analyze the effects of treatment with nerve growth factor, intranasally delivered to the brain parenchyma, on the outcomes of traumatic brain injury.
Key Words: intranasal delivery; nerve growth factor; pharmacology; traumatic brain injury
Introduction
Traumatic brain injury (TBI) is sudden damage to the brain resulting from external mechanical force, such as impact, severe acceleration/deceleration,and blunt force.The global highest incidence rates of TBI between 1990 and 2006 were in Central Europe, Eastern Europe, and Central Asia.Incidence,prevalence, and years of life lived with disability estimate for every cause of injury by age, sex, and location for 1990-2016 are available through the tool at http://ghdx.healthdata.org/gbd-results-tool.To date, there are no pharmaceutical therapies aimed at treating the multiple outcomes of TBI.Only palliative care are available that, according to the definition of the World Health Organization (https://www.who.int/health-topics/palliativecare), improves the quality of life of patients, facing the problem associated with life-threatening illness, through the prevention and relief of suffering by employing early identification, assessment and treatment of pain and physical, psychosocial and spiritual problems.
Nerve growth factor (NGF) is a neurotrophic peptide primarily discovered for its ability in regulating the growth and survival of peripheral sensory,sympathetic, and central cholinergic neurons.Fifty years of studies have then shown that NGF also targets non-neuronal cell populations in the central nervous system (CNS), modulating their behavior.This NGF peculiarity has laid the foundation for a broad line of pre-clinical and clinical studies aimed to investigate its pharmacological potential for the treatment of neurodegenerative and neurotraumatic diseases (Manni et al., 2021).This potential has further increased in the last two decades since it has been demonstrated the possibility of reaching neurotrophin targets in the brain through its intranasal delivery, which allows bypassing the blood-brain barrier and ensures rapid and extensive spreading of the drug through the brain parenchyma (Manni et al., 2021).
This review summarized the current knowledge about specific molecular mechanisms that are dysregulated in TBI and may be targeted and modulated by NGF treatment, highlighting the possible role that intranasal NGF could play in the prevention and/or recovery of acute and chronic TBI outcomes.
Search Strategy
The articles included in this review were retrieved by an electronic search of the PubMed database, up to 2021, for literature describing the role of NGF on TBI.Dozens of search sessions were conducted, using the phrases“traumatic brain injury” and/or “nerve growth factor” combined with one or more of following keywords (principal among others): neuroinflammation,microglia, astrocyte, beta-amyloid, tau, mitochondria, oxidative stress,excitotoxicity, energy metabolism, protein aggregation, protein misfolding,intranasal delivery, intra-cerebroventricular, intra-parenchyma, therapeutic target.Articles were included if they were deemed to contribute to the understanding of the link between TBI and NGF and the therapeutic potential of the latter in counteracting or overcoming the disabling outcomes of TBI.
Molecular Mechanisms Involved in Primary and Secondary Traumatic Brain Injury
TBI is made up of two closely connected phases.Primary injury occurs at the moment of trauma and is directly induced by the force of the impact which mechanically destroys blood vessels and cellular membranes, produces axonal sharing, and may damage the blood-brain barrier and meninges.Secondary injury is the direct result of primary injury and leads to cellular and metabolic damages triggered in the first few hours and days by primary mechanical injury (Ng and Lee, 2019).
TBI excitotoxicity and neuroinflammation
The development of neuroinflammation is one of the main effects of secondary injury that encompass the activation of two types of glial cells,microglia (Eyolfson et al., 2020) and astrocytes (Zhou et al., 2020).These cells possess the peculiar characteristic of playing a role in both reparative and neurodegenerative processes (Kwon and Koh, 2020).This characteristic is due to the potential to assume different phenotypes, in response to environmental stimuli and the animal’s ability to adapt to the evolution of the early response to injury (Kwon and Koh, 2020).In acute post-damage phases, rupture ofmembranes results in the release of damage-associated molecular patterns,priming the brain resident microglia (Simon et al., 2017).Microglia cells are the primary mediators of the brain’s innate immune response and react to TBI within minutes (Mira et al., 2021).Microglia are highly plastic cells that can quickly switch from anti-inflammatory (M2-like) to pro-inflammatory (M1-like) phenotype and vice-versa depending on the different pathophysiological conditions of the microenvironment.Under physiological conditions, microglia exist in a surveillance state with branched morphology.In response to TBI,microglial cells are activated and assume the pro-inflammatory phenotype,with amoeboid morphology (Eyolfson et al., 2020), which has the primary function to eradicate cellular and molecular debris.In addition to proinflammatory cytokines (such as interferon-γ, tumor necrosis factor-α, and interleukin-1β), activated microglia also produce other neurotoxic products after an injury such as nitric oxide and superoxide free radicals that generate reactive oxygen species (ROS) and reactive nitrogen species (Mannix and Whalen, 2012).In microglia, ROS are generated primarily by NADPH oxidase 2 which is associated with damage-associated molecular pattern signaling,inflammation, and amyloid plaque deposition (Simpson and Oliver, 2020).Indeed, although microglia play a pivotal role in the clearance of amyloid-beta(Aβ)-plaque, after TBI it is involved in Aβ-plaque deposition both directly, as the active microglia exhibit increased expression of γ-secretase (Nadler et al.,2008), and indirectly, as the microglia-released pro-inflammatory cytokines can specifically stimulate γ-secretase activity, concomitant with increased production of Aβ (Liao et al., 2004).
In healthy individuals, astrocytes accomplish many structural and support functions.They regulate the cerebral perfusion, maintain the brain blood flow(Marina et al., 2020), preserve the blood-brain barrier integrity (Kadry et al.,2020), and regulate neurotransmitter homeostasis, uptaking and metabolizing synaptically-released neurotransmitters and releasing their precursors back to neurons (Mahmoud et al., 2019).Astrocytes respond to TBI by a process commonly referred to as reactive astrogliosis, which involves their structural and functional alterations, including hypertrophy and increased expression of the intermediate filaments (nestin, vimentin, and glial fibrillary acidic protein)(Zhou et al., 2020).In response to TBI, astrocytes not only proliferate but also increase their size and form an astroglial scar that is a protective physiological mechanism to avoid the spreading of secondary damage to other brain regions (Mira et al., 2021).However, astroglial scar often exacerbates negative outcomes such as excitotoxicity and neuroinflammation (Zbesko et al., 2018).Following TBI, astrocytes are responsible for spontaneous seizure and epileptiform activity (Shandra et al., 2019).They strongly contribute to the extracellular accumulation of excitatory amino acids, both by increasing their release due to cell breakdown and intracellular calcium accumulation and by decreasing the glutamate reuptake, which was found downregulated in postmortem astrocytes from TBI patients (van Landeghem et al., 2006)and TBI animal models (Goodrich et al., 2013).Glutamate accumulation also interferes with the physiologic neuronal function, which relies on the constant orchestration and integration of excitatory and inhibitory potentials.In astrocytes, glutamate is converted to glutamine and returned to its presynaptic cell or neighboring γ-aminobutanoic acid (GABA) interneuron for conversion back to glutamate and then to GABA, respectively (Guerriero et al.,2015).The TBI-induced impaired glutamine traveling to GABA interneurons may decrease GABA synthesis and impact local inhibition (Guerriero et al.,2015).Astrocytes also play a pivotal role in the dynamic regulation of cerebral circulation (Takahashi, 2022).Having processes whose ends surround blood vessels, astrocytes create contact with vascular smooth muscle and vessel endothelium and create a physical barrier known as the blood-brain barrier(Gollihue and Norris, 2020).Signaling between astrocytes and vascular smooth muscle controls the muscle tone regulating the cerebral blood flow while signaling between astrocytes and endothelium regulates angiogenesis,transport across the blood-brain barrier, and maintenance of tight junctions(Takahashi, 2022).
The human brain is a high-energy consuming organ that uses glucose as its main source of energy.Glucose reaches different brain areas through facilitated diffusion and can be metabolized in the glycolytic pathway or stored as glycogen.The anatomical peculiarities and the direct access to the vasculature make the astrocytes prone to the uptake of glucose directly from the bloodstream supporting energy supply to neurons under conditions of a high-energy demand (Deitmer et al., 2019), especially since astrocytes represent the major glycogen stores (Deitmer et al., 2019).The final product of the glycolytic pathway is pyruvate which is metabolized in the citric acid cycle when oxygen is present and alternatively converted to lactate when oxygen is lacking.According to the “Astrocyte-to-Neuron Lactate Shuttle”hypothesis, lactate is primarily produced by astrocytes in a manner sensitive to excitatory neuronal activity.Following TBI, the lactate concentration increases in the brain extracellular fluid due to high glycolytic activity indicative of hypoxia or mitochondrial dysfunction (Carpenter et al., 2015).Furthermore, the injured neurons early following severe TBI are unable to pick up and metabolize the increased lactate, resulting in a lactate storm in the environment that can be toxic and incompatible with life (Lama et al.,2014).
TBI and energy metabolism
Mitochondria are important organelles in the life-death balance.Mitochondria not only synthesize adenosine 5′-triphosphate (ATP) supporting cellular energy needs but also play an important role in cellular calcium buffering,ROS regulation, and activation of the apoptotic cascade.Mitochondria are dynamic organelles capable of changing shape, size, and organization in response to external stimuli (Simmons et al., 2020).A growing body of literature from both clinical and experimental brain injury research has shown that structural and functional damage to mitochondria is an early event after TBI that contributes to cell death and poor cognitive outcome (Fischer,2017) and that TBI is characterized by altered mitochondrial dynamics and bioenergetics pattern (Simmons et al., 2020).In a physiological system, the loss of mitochondrial functions triggers a selective neuroprotective mitophagy process, which ensures the clearance of the dysfunctional mitochondria through the lysosomal pathway.In neurodegenerative diseases, the mitophagy process is hindered by a defective autophagosomal/endosomal/lysosomal system (Simmons et al., 2020).TBI results in alternate equilibrium among mitophagy and increased ROS production, calcium accumulation,and release of cytochrome C that can start, drive, or accelerate the cell death process (Zhu et al., 2022).The morphological changes of mitochondria ensure tethering and joining of two mitochondria through the mechanism known as fusion and division and cleavage of mitochondria in the process of fission.Functional fusion/fission processes ensure normal mitochondrial homeostasis maintaining cell stability and survival.Fission is essential to maintain the number and location of mitochondria in case of altered cellular energy requirement and clearance of dead mitochondria and is mediated by dynamin-related proteins, in particular Drp1, that trigger a signaling pathway resulting in mitochondria fragmentation.TBI causes a decrease in mitochondrial size and increased Drp1 translocation to mitochondria,indicating an increase in fission events (Simmons et al., 2020).Mitochondrial fusion requires both outer and inner mitochondrial components, such as mitofusin 1 and 2 and optical atrophy protein 1 (Opa1).TBI brains are characterized by reduced fusion marker Opa1 (Zakarya et al., 2020).Di Pietro et al.(2017) deepen this evidence by showing that mild TBI is characterized by increased fusion and concomitantly decreased fission and mitophagy processes, while severe TBI is more prone to activate fission and mitophagy,paralleled to a remarkable downregulation of fusion.
TBI and protein aggregation
TBI is characterized by the rapid and long-term accumulation of proteins which probably reflects the disruption of axonal transport following extensive axonal damage (Smith et al., 2003).Although many proteins are found accumulating after TBI, amyloid precursor protein and its proteolytic products, Aβ peptides, neurofilament proteins, and synuclein proteins have aroused greater interest as their accumulation highlights the role of TBI as an adjuvant factor in the development of neurodegenerative disorders, such as Alzheimer’s disease (AD) and Parkinson’s disease (Smith et al., 2003).Tau is a microtubule-associated binding protein that, under physiological conditions,provides cytoskeletal support allowing axonal transport dependent on its post-translational phosphorylation state.Hyper-phosphorylated tau (hptau) molecules dissociate from microtubules in the axon, translocate to the cell body and proximal dendrites, and aggregate into intracellular inclusions termed neurofibrillary tangles that are considered the pathological hallmark of tauopathies including AD and chronic traumatic encephalopathy among others (Edwards et al., 2020).After TBI, hp-tau, and neurofibrillary tangles can be detected as early as 6 hours (Smith et al., 2003), especially in the brain areas close to the impacted region (Edwards et al., 2020).
Alpha-synuclein (α-Syn) aggregation is a hallmark of Parkinson’s disease but is also a common feature in patients and animal models experiencing the outcomes of TBI (Brown and Goldman, 2020; Delic et al., 2020).Physiological functions of α-Syn are poorly understood, but evidence has suggested its role in synaptic plasticity, dopamine regulation, and membrane trafficking.A strict interplay and relationship between aggregated α-Syn and hp-tau has been reported and related in general to the establishment of a deleterious feed-forward loop responsible for the development and spreading of neurodegeneration (Moussaud et al., 2014; Yan et al., 2020), through mechanisms such as the generation of severe mitochondrial dysfunctions(Feng et al., 2021).
Extracellular Aβ deposits in the brain are a hallmark of AD.Autopsies of young TBI patients show diffuse Aβ plaques similar to those found in AD patients close to the impacted region in both grey and white matter regions(Ramos-Cejudo et al., 2018).Aβ is released by sequential cleavage in the cell membrane of the amyloid precursor protein (APP), physiologically involved in synaptogenesis and synaptic plasticity.First, β-secretase removes the ectodomain of APP, and then γ-secretase cleaves the remaining C-terminal fragment of APP’s transmembrane domain, favoring the translocation of Aβ from the cellular membrane to the extracellular space.Aβ plaques enhance inflammation, oxidative stress, and the development of cerebral microvascular disease, also promoting the loss of microglial cells and the senescence of neural stem/progenitor cells by affecting forebrain and hippocampal neurogenesis and eliciting a senescence response in associated astrocytes(Johnson et al., 2010).Microglia play a central role in Aβ accumulation after TBI (Mannix and Whalen, 2012), contributing to the phagocytic clearance of Aβ but can also promote its formation through the activation of γ-secretase,boosted by the microglial secretion of inflammatory cytokines (Mannix and Whalen, 2012).
Nerve Growth Factor for Traumatic Brain Injury Management
The delivery of NGF in clinical studies has been pursued since 1980 for the treatment of diseases such as peripheral neuropathies or AD, to provide trophic support to damaged, NGF-responsive neurons of the peripheral and central nervous system (Aloe et al., 2012).Despite the relative failuresof these attempts, mainly related to the invasiveness of pharmacological delivery methods and the development of potentially harmful side effects,NGF has been studied, in more recent times, for its pharmacological potential,first on ophthalmic pathologies (Eftimiadi et al., 2021), and therefore on the outcomes of neurotraumas (Manni et al., 2021).For the latter, the rationale for the development of NGF-based treatment protocols was founded on: the action of NGF on cellular targets in the CNS other than central cholinergic neurons (i.e.glial cells, immune cells, and the vascular endothelium) (Manni et al., 2021); preclinical and clinical evidence for a neuroprotective action of endogenous NGF after TBI (Da Silva Meirelles et al., 2017; Lin et al., 2021);the possibility of using delivery methods, namely intranasal inoculation, for targeting of CNS structures, which guarantees low invasiveness associated with satisfactory safety profiles (Manni et al., 2021).
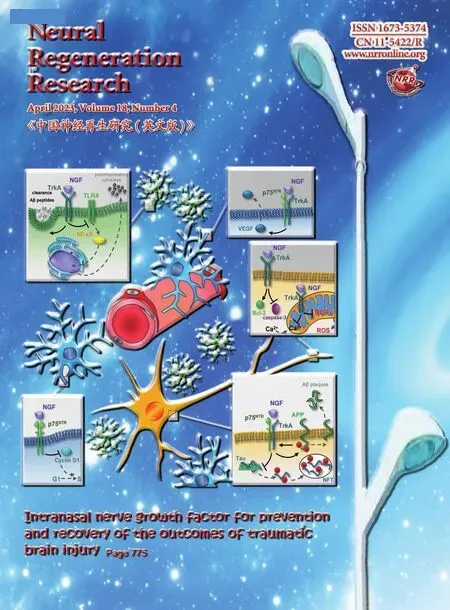
There is both preclinical and clinical evidence, which indicates how treatment with NGF can positively influence the evolution of clinical pictures secondary to TBI (Manni et al., 2021).In recent years, the intranasal route of NGF administration has become increasingly important, so much so that it is currently the subject not only of preclinical studies but also of clinical trials in patients suffering from the outcomes of TBI (EudraCT N.2019-002282-35, https://www.clinicaltrialsregister.eu/ctr-search/trial/2019-002282-35/IT; NCT01212679, https://www.clinicaltrials.gov/ct2/show/NCT01212679?term=intranasal+NGF&draw=2&rank=2) (Chiaretti et al., 2017).Table 1 summarizes all the manuscripts in which the effect of intranasally delivered NGF on the outcomes of TBI has been studied.These data have been discussed in the successive chapter “Intranasal NGF and TBI”.NGF administered intranasally effectively diffuses into the brain parenchyma,via an anterior pathway following the olfactory nerve and a posterior pathway through the trigeminal nerve.For details regarding the pharmacological characterization of intranasal NGF, the reader is referred to the seminal work of the Thorne and Frey group and to a more recent review of our group (Thorne and Frey, 2001; Manni et al., 2021).Recent studies have already shown how through the intranasal delivery of NGF it is possible to act effectively on some of the molecular dysfunctions described up to now and related to the progression of brain damage after trauma (Cattaneo and Capsoni, 2019; Manni et al., 2021; Figure 1).For some others, it is still necessary to develop an adequate preclinical research path, which however is founded on solid rational assumptions that will be exposed immediately below.

Table 1 |Traumatic brain injury and intranasal nerve growth factor
NGF and neuroinflammation
The first possible benefit deriving from the delivery of NGF to the brain for the therapy of TBI entails the reduction of neuroinflammation.NGF itself is an anti-inflammatory molecule, capable of modulating the synthesis of inflammation mediators and the phenotype of immune cells, during chronic inflammation in the peripheral field (Minnone et al., 2017).In the central nervous system, it partakes in the regulation of the metabolism and function of astrocytes and microglia, both cell populations being involved in the generation and deleterious maintenance of neuroinflammation (Colombo and Farina, 2016; Kwon and Koh, 2020).NGF regulates the phenotypes and functions of astrocytes and microglia (Pӧyhӧnen et al., 2019).In vitro
studies have shown that NGF stops the cell cycle of astrocytes in the G1 phase, inhibiting the induction of cyclins and the activation of cyclindependent kinases (Cragnolini et al., 2012; Figure 1), an effect that limits the phenomenon of astrogliosis and the formation of the glial scar.Intranasal administration of NGF in patients with TBI outcomes induces a significant increase in energy metabolism, as demonstrated by the increased uptake of the fluorodeoxyglucose tracer shown in the PET-CT scans (Chiarettiet al., 2017).Thus, an effect of NGF in the regulation of the metabolic interplay between astrocytes and neurons, dysregulated after TBI (Carpenter et al., 2015), should not be excluded, even if not yet directly demonstrated.Furthermore, the prevalent expression of the p75but not of TrkA was demonstrated in the primary culture of astrocytes (Cragnolini et al., 2012).Exogenous NGF could therefore compete with endogenous proNGF for the activation of this receptor on astrocytes, positively modulating astrocytic functions related to neuroreparative processes (Pӧyhӧnen et al., 2019).Additionally, NGF directs microglia toward a neuroprotective phenotype (Rizziet al., 2018).Its regulation of the inflammatory response of primary mouse microglia was obtained via the activation of the high-affinity receptor TrkA(Fodelianaki et al., 2019).In thisin vitro
model, NGF downregulates LPS-induced production of pro-inflammatory cytokines and nitric oxide, inhibits TLR4-mediated activation of the NF-κB and JNK pathways, and reduces microglial glycolysis (Fodelianaki et al., 2019; Figure 1).In primary microglia cultures, the regulation of the neuroprotective microglial phenotype by NGF also pertains to the increase in membrane dynamics and macropinocytosis and the increase in motility (De Simone et al., 2007; Rizzi et al., 2018).Moreover, NGF intranasal treatment in AD transgenic mice modulates inflammatory proteins such as the soluble tumor necrosis factor-α receptor II and the chemokine CXCL12 (Capsoni et al., 2017; Figure 1).
Figure 1|Intranasal NGF for TBI management.
NGF and protein aggregation
A further mechanism through which the acute and chronic outcomes of TBI can benefit from treatment with NGF pertains to the action of neurotrophin on the metabolism, misfolding, and aggregation of proteins such as Aβ,tau, and α-Syn.NGF, dampening pro-inflammatory cytokine production by microglia in the injured brain, is effective in reducing Aβ accumulation and cytotoxic effects by promoting its clearance by microglia (Capsoni et al., 2017).Furthermore, a direct interaction between APP and TrkA was demonstrated,which may route APP metabolism toward a non-amyloidogenic fate.TrkA receptor binding to APP relies on a 20 amino acids long portion of APP,located in the juxtamembrane/extracellular domain and comprised between β- and α-secretase cleavage sites (Canu et al., 2017a, b).This interaction occurs in the plasma membrane, endoplasmic reticulum (ER), Golgi, and endocytic vesicles where NGF controls the level of APP/TrkA association, by regulating the phosphorylation state of APP (Canu et al., 2017a, b; Figure 1).Thus, increasing NGF concentration and TrkA activation in the injured brain may shift the balance between amyloidogenic and non-amyloidogenic metabolism of APP toward the latter, as has been already described in a mouse model of AD (Cattaneo and Capsoni, 2019).
On the other hand, both endogenous and exogenous NGFs have been proven effective in regulating tau metabolism and post-translational modifications.Exogenous NGF regulates tau turnover in PC12 cells (Sadot et al., 1996) and its deprivation induces hp-tau (a prodromal of its aggregation in neurofibrillary tangle) in the samein vitro
model (Nuydens et al., 1997).Pharmacological stimulation of endogenous NGF or exogenous NGF delivery was effective in reducing tau phosphorylation in the brain of animal models of AD (Congdon and Sigurdsson, 2018).Interestingly, the relationship between proNGF and NGF in the nervous system plays a central role in the regulation of tau metabolism.ProNGF induces hp-tauin vitro
, challenging p75and activating glycogen synthase kinase-3β (Shen et al., 2018).The increased production of proNGF by reactive astrocytes after trauma in the nervous system has been demonstrated (Cheng et al., 2020).Moreover, the interaction between proNGF and p75participates in the development of the secondary brain damage after trauma (Sebastiani et al., 2015), while counteracting the activation of p75or blocking proNGF provides neuroprotection and preserves sensorimotor function in a mouse model of cortical impact(Montroull et al., 2020).Thus, it is conceivable that the exogenous delivery of NGF in TBI may shift the proNGF/NGF balance in favor of the mature form of neurotrophin, attenuating, among others, the effects of proNGF on hp-tau.Less is known about the relationship between NGF and α-Syn in TBI.The gene expression and protein production of the rat homolog of human α-Syn is upregulated after NGF treatment of PC12 cells (Stefanis et al., 2001), indicating a possible mechanism for NGF participation in presynaptic plasticity.An indirect relationship between normal NGF production in the brain and α-Syn metabolism is suggested by the evidence that NGF gene expression, as well as NGF-TrkA signaling, are reduced in diseases, such as Parkinson’s disease and dementia with Lewy bodies, characterized by the neurotoxic accumulation of α-Syn aggregates (Tong et al., 2009).However, to the best of our knowledge,a direct relationship between NGF/NGF-signaling deficiency and the pathological aggregation of α-Syn has not yet been demonstrated.
NGF and energy metabolism
NGF regulates several mitochondrial functions, thus it can positively affect the mitochondrial dysfunction generated by TBI (Simmons et al., 2020).NGF receptors are expressed in the mitochondrial compartment and TrkA activation protects isolated mitochondria of rat brain cortex from mitochondrial permeability transition induced by [Ca] (Carito et al., 2012).Moreover,NGF activates glutathione redox cycling and suppresses mitochondrial ROS production in cultured neurons (Kirkland et al., 2007).Continuous infusion of NGF in a rat model of TBI stimulates the activity of antioxidant enzymes in brain tissues, attenuating the neuronal damage induced by oxygen-free radicals, reducing the severe overload of [Ca], and stabilizing its homeostasis(Zhou et al., 2003; Figure 1).NGF also protects against neuronal death caused by mitochondrial toxins, regulating the gene expression of the transcriptional coactivator PGC-1α, a modulator of mitochondrial-related gene expression(Chen et al., 2012).Furthermore, a disruption of the cAMP response elementbinding protein activity, such as that described in rat brain after TBI (Atkins et al., 2009), decreases the expression of a subset of mitochondrial genes and down-regulate mitochondrial respiration (Lee et al., 2005).Improving NGF-signalling induces, in turn, the phosphorylation of cAMP response elementbinding protein (Sofroniew et al., 2001) with a subsequent decrease in the intracellular content of ROS and increased expression of the mitochondrial antioxidant enzyme manganese superoxide dismutase (Bedogni et al., 2003).It is also worth noting that NGF boosts mitochondrial remodeling in PC12 cells, inducing higher levels of fission (P-Drp1) and fusion (Opa1 and Mfn2)proteins and upregulating Sirt3 and the transcription factors mtTFA and PPARγ, which in turn regulate mitochondria biogenesis and metabolism,sustaining mitochondrial mass, potential, and bioenergetics (Martorana et al., 2018).Such a mechanism, whether active after NGF delivery to the brain,may effectively counteract the TBI-induced dysfunctions in mitochondrial remodeling (Zakarya et al., 2020).
Positive effects on brain perfusion have been observed after administration of NGF to the brain of both laboratory animals and humans (Chiaretti et al.,2017, 2020; Manni et al., 2021).It is known that NGF has a pro-angiogenic activity, regulating the production of vascular endothelial growth factor(Manni et al., 2005), a growth factor expressed either by neurons, glia and endothelial cells (Ogunshola et al., 2000; Nag et al., 2002) and promoting the proliferation and migration of endothelial cells (Graiani et al., 2004; Salis et al., 2004; Figure 1).Intranasal NGF is effective in stimulating neo-angiogenesis following cerebral infarction in rats, an effect linked to the activation of PI3k/Akt signaling (Li et al., 2018).Moreover, NGF stimulates the production of vasodilating agents, such as nitric oxide (Nizari et al., 2021), promotes the innervation of the cerebral vasculature (Isaacson et al., 1990), and affects the glial regulation of brain perfusion and metabolism (Rasband, 2016).At least some of these possible mechanisms may reasonably be activated after intranasal administration of NGF to the brain parenchyma, underlying the observed positive effects on brain perfusion, reported after NGF delivery to the human brain (Chiaretti et al., 2017, 2020; Manni et al., 2021).
Intranasal Nerve Growth Factor and Traumatic Brain Injury
Intranasal administration of NGF (IN-NGF) in preclinical models of TBI(Table 1) indicates that through this pharmacological tool it is possible to alter the course of the disease and probably avoid the development of the disabilities and suffering that afflict not only patients but also their families and caregivers.As summarized in Table 1, only one out of four preclinical studies find that IN-NGF is not effective in ameliorating TBI-induced deficits(Young et al., 2015).Conversely, IN-NGF in rats subjected to TBI can improve Aβ deposition, locomotor activity, and spatial memory (Tian et al., 2012), to attenuate the formation of cerebral edema, simultaneously decreasing both the production of inflammatory cytokines and the apoptosis mediated by the mitochondrial response to trauma (Lv et al., 2013), as well as to counteract the hyper-phosphorylation of tau through the inhibition of glycogen synthase kinase-3β activity (Lv et al., 2014).In all of these studies, NGF is administered in proximity to (immediately before or after) the trauma.The clinical data reported up to now (Chiaretti et al., 2017) are instead obtained by treating a stabilized and chronic picture, several months after the trauma.The study in question highlights how IN-NGF can improve parameters of perfusion,metabolism, and brain function (measured by analyzing the EEG), even after the chronicization of brain damage and the development of severe disabilities.It is however desirable that future NGF-based pharmacology for TBI will be developed as a tool for intensive care units, where the neuroprotective potential of NGF can be exploited to avoid the spread of injury from trauma and the consequent development of severe disabilities.The clinical data published so far show how IN-NGF can restore brain perfusion, as well as reactivate the metabolic activity of brain cells, which was blunted following trauma (Chiaretti et al., 2017).Despite these promising data, mere metabolic reactivation may not be sufficient for the recovery of the connectivity and therefore the functions of the circuits involved in the damage.It is, therefore,necessary to explore the effect of the association between intranasal NGF and therapies aimed at activating circuits that connect specific cortical areas with their sub-cortical counterparts (among others the cortical-striatalthalamic-cortical loop), to avoid or recover the loss of motor and/or cognitive functions.Currently, stimulation through electrical currents (transcranial direct current stimulation) or magnetic currents (transcranial magnetic stimulation) appear to be promising, capable of modifying and/or stimulating the recovery of connectivity between the cortex and specific subcortical areas(Polanía et al., 2012; Carmi et al., 2018), an effect that could be facilitated by the recovery, promoted by NGF, of brain metabolism and perfusion,mitochondrial functions, glial phenotypes, and activity.
Author contributions:
LM and MS wrote the first draft of the manuscript.All authors contributed to manuscript revision and approved the submitted version.
Conflicts of interest:
The authors declare no conflicts of interest.
Availability of data and materials:
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Open access statement:
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:
Maria Jose Bellini, Universidad Nacional de La Plata,Argentina.
Additional file:
Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- Neural and Müller glial adaptation of the retina to photoreceptor degeneration
- Agomelatine: a potential novel approach for the treatment of memory disorder in neurodegenerative disease
- MicroRNAs: protective regulators for neuron growth and development
- In vivo astrocyte-to-neuron reprogramming for central nervous system regeneration: a narrative review
- Altered O-GlcNAcylation and mitochondrial dysfunction,a molecular link between brain glucose dysregulation and sporadic Alzheimer’s disease
- Signaling interactions among neurons impact cell fitness and death in Alzheimer’s disease