Association between cardiovascular implantable electronic devices and tricuspid regurgitation: a casecontrol study
Yuan-yuan Zhang ,Yan Cheng ,Liang-rong Zheng ,Zhe-lan Zheng
1 Department of Cardiovascular Ultrasonic Center,the First Affiliated Hospital,Zhejiang University School of Medicine,Hangzhou 310003,China
2 Department of Cardiology,the First Affiliated Hospital,Zhejiang University School of Medicine,Hangzhou 310003,China
Cardiovascular implantable electronic devices (CIEDs)are widely used in the modern era.Every year,about 730,000 permanent pacemakers and 330,000 CIEDs are implanted worldwide.CIEDs have been known to increase the life expectancy of millions of people and improve their quality of life by controlling the heart rate and atrioventricular and interventricular synchronization and preventing sudden cardiac death.The tricuspid valve consists of the annulus,leaflets,chordae tendineae,and papillary muscles.Interaction between the endocardial lead and any component of this structure can lead to tricuspid valve dysfunction,thereby resulting in tricuspid regurgitation (TR).CIED-related TR has been shown to be an independent predictor of hospitalization for heart failure.
In this study,we reviewed the records of patients who had a CIED inserted in our hospital and used three-dimensional(3D) echocardiography to locate the relative position of the endocardial lead to the tricuspid valve,in order to investigate the factors and mechanisms influencing device lead-related TR.
METHODS
Study design
This study included patients who experienced moderate or severe TR following CIED implantation in our hospital from January 2018 to December 2021.Ethical approval was obtained from the research ethics committee of the hospital.
All eligible patients had indications for CIED placement.Patients were excluded for any of the following reasons:cardiogenic shock or those scheduled for cardioversion within 24 h after the procedure;patients with a history of pulmonary embolism,heart surgery,dialysis,acute coronary artery syndrome,or revascularization.After applying similar inclusion criteria,controls who experienced mild TR following CIED implantation were matched (1:3) to cases according to age,sex,and index year.
Data collection
Patient demographic data and device information were collected from the electronic medical records using a standardized form.All the echo assessments were performed by a single investigator,and the acquired data were reanalyzed by another operator (blinded to the patients’ former results).TR was quantified in three grades (mild,moderate,and severe) using the classical variables of regurgitant volume calculated using the proximal isovelocity surface area method.The device lead position at the level of the tricuspid annulus was identified using 3D images obtained from the apical 4-chamber view.
Statistical analysis
Continuous data are presented as the mean±standard deviation (SD),while categorical variables are shown as frequencies (percentages).Differences between two groups were assessed using Student’s-test for continuous variables and Chi-square test for categorical variables.Logistic regression was used to estimate the association between CIEDs and TR and to calculate the odds ratios (s) and 95% confidence intervals (s).The kappa (κ) coefficient was calculated to determine interobserver agreement.Statistical significance was set at a-value <0.05.All statistical analyses were performed using SPSS version 20 (SPSS Inc.,USA).
RESULTS
Clinical and two-dimensional (2D)echocardiographic features
Overall,35 patients (the moderate and severe TR group)and 105 controls (the mild TR group) were included in the analysis.The baseline clinical characteristics of the study sample were presented in supplementary Table 1.Most patients exhibited New York Heart Association (NYHA) class II symptoms,and approximately half of the patients had sinusnode dysfunction.
The 2D echocardiographic characteristics were compared in supplementary Table 2.No significant differences between pre-and post-implantation echocardiograms were observed in the mild TR group,indicating preservation of cardiac structure and function following CIED implantation.Nevertheless,structural parameters,including the left atrium area,right atrium area,right ventricular diameter,and subsequent pulmonary artery systolic pressure,were significantly increased in the moderate and severe TR group.Perfect interobserver (=0.93) agreement was achieved for echocardiography measurements.
Device information and 3D echocardiographic characteristics
Device information and 3D echocardiographic characteristics were presented in supplementary Table 3.The majority of patients in the moderate and severe TR group received ventricular pacing or implantable cardioverter defibrillator (ICD) implantation,whereas most patients in the mild TR group received dual-chamber pacing (<0.01).Furthermore,3D echocardiography revealed that patients with moderate or severe TR had a significantly greater incidence of interfering leads than those with mild TR.Approximately 65.7% of patients who developed moderate or severe TR had lead-leaflet interference,while this rate was only 10.5%in patients with mild TR.The posterior leaflet was most commonly affected,followed by the septal leaflet.In both groups,the anterior leaf let was the least affected.Representative images were shown in Figure 1.Notably,the location of the lead tip did not differ significantly between the groups.

Figure 1. Three-dimensional echocardiography depicts the location of the device lead (A to D: representative images from the mild TR group;E to G: representative images from the moderate and severe TR group) and lead tips (H and I: representative images of lead tips from the mild TR group;J: representative image from the moderate and severe TR group).M: device lead in the middle of the valve;AP: device lead in the anteroposterior commissure;AS: device lead in the anteroseptal commissure;PS: device lead in the posterior-septal commissure;A: anterior leaf let impingement;S: septal leaf let impingement;P: posterior leaf let impingement;IVS: interventricular septal;RVOT: right ventricular outflow tract.
Predictors of CIED-related TR
The associations between CIEDs and TR were shown in Table 1.An increase in risk was observed with atrial fibrillation involving forward rotation (1.814,95%1.731-1.897).In addition,we investigated the associations with device information.A modest increase in risk was observed who underwent single-chamber pacemaker (1.811,95%1.732-1.890) and ICD implantation (1.790,95%1.713-1.867).The association between device lead location and TR was examined.Reduced risks were observed for the presence of inter-leaf let lead (0.440,95%0.298-0.582).
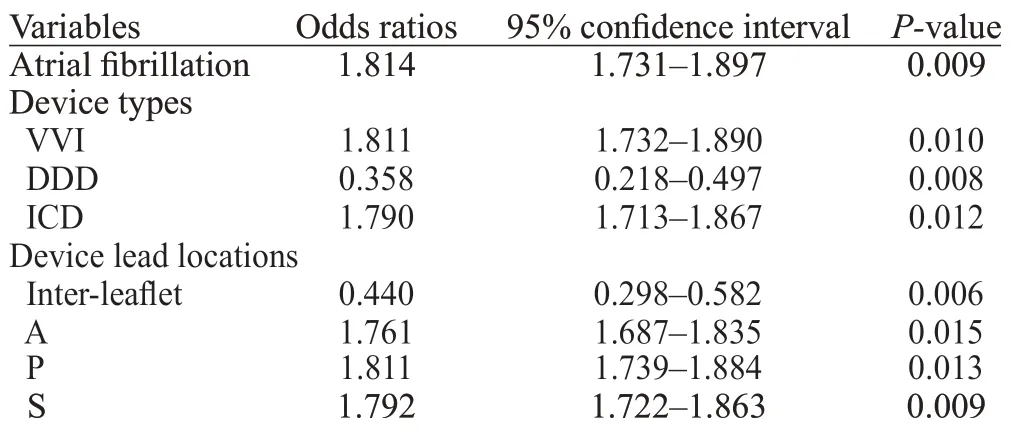
Table 1. Association between the cardiovascular implantable electronic devices and tricuspid regurgitation
DISCUSSION
In this retrospective study,we evaluated the presence of TR following CIED implantation by using 3D echocardiography.Our results indicated that atrial fibrillation,device type,and interfering leads were associated with postimplantation TR.We did not observe any difference in TR severity in relation to the lead tip location.
The present study showed the useful application of 3D transthoracic echocardiography in the identification of device lead-related TR.By allowing a more detailed assessment of the tricuspid valve and its subvalvular apparatus,3D was found to be superior to 2D echocardiography in the evaluation of tricuspid valve pathology.Anview of the tricuspid valve leaflets from both the atrial and ventricular aspects can be obtained by 3D echocardiography,allowing the evaluation of all three leaf lets from the base to the tip,including the posterior leaf let.
We also found that interfering lead was a major contributor to post-implantation TR.The posterior and septal leaflets were most likely impinged on by device leads,resulting in insufficient valve closure.A previous study indicated that the presence of an interfering lead was the most important factor associated with worsening TR,increasing the likelihood of developing moderate or severe TR by 15-and 11-fold,respectively.As lead positions can be identified with 3D echocardiography,it could be an effective tool for detecting device lead-related TR in patients with CIEDs.
Patients with ventricular pacing and ICD implantation were more likely to develop considerable TR than those with dual-chamber pacing.These results agree with a prior study showing that dual-chamber pacing was superior to ventricular pacing in potentially attenuating electromechanical dyssynchrony and long-term cardiac function decline.ICD leads to more fibrosis and hence more interference with the tricuspid valve results in higher TR.Meanwhile,the transvalvular lead of the ICD may generate additional weight and rigidity to the tricuspid valve due to its calibre.
Our findings revealed that preimplantation atrial fibrillation was involved in the presence of post-implantation TR.Some studies have reported that atrial fibrillation is associated with annular dilation and results in TR even in the absence of device leads.
CONCLUSIONS
Preimplantation atrial fibrillation,device type,and interfering leads are associated with post-implantation TR.To better detect device lead-related TR,3D echocardiography is recommended for patients with CIEDs.
This work was supported by grants from the Planned Science and Technology Project of Zhejiang Province,China(2020KY216);Hangzhou City Health Science and Technique Program(OO20190126).
All these cases provided informed consent,and the study was approved by the Ethics Review Committee of the First Affiliated Hospital,Zhejiang University School of Medicine.
None.
LRZ designed the study.YYZ and YC collected the patient data.YYZ wrote the article.All authors read and approved the final manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World Journal of Emergency Medicine2022年5期
World Journal of Emergency Medicine2022年5期
- World Journal of Emergency Medicine的其它文章
- Intestinal microcirculation dysfunction in sepsis:pathophysiology,clinical monitoring,and therapeutic interventions
- Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study
- Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study
- Analysis of imaging characteristics of blunt traumatic aortic dissection: an 8-year experience
- Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial
- Arctigenin attenuates paraquat-induced human lung epithelial A549 cell injury by suppressing ROS/p38 mitogen-activated protein kinases-mediated apoptosis
