Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study
Gan-nan Wang ,Zhong-man Zhang ,Wen Chen ,Xiao-quan Xu ,Jin-song Zhang
1 Department of Emergency,the First Affiliated Hospital of Nanjing Medical University,Nanjing 210029,China
2 Department of Radiology,the First Affiliated Hospital of Nanjing Medical University,Nanjing 210029,China
BACKGROUND: To assess the association between relevant brain computed tomography (CT)parameters at different time and neurological prognosis in adult comatose survivors after cardiac arrest (CA).METHODS: A total of 94 CA patients who underwent early and late CT scans (within 24 h and 24 h to 7 d respectively after CA) between January 2018 and April 2020 were enrolled in this retrospective study.According to the Cerebral Performance Category (CPC) score at hospital discharge,the patients were divided into either a good outcome (CPC 1-2) group or a poor-outcome group (CPC 3-5).The grey-to-white matter ratio (GWR) and the proportion of cerebrospinal fluid volume (pCSFV) were measured.In predicting poor outcomes,the prognostic performance of relevant CT parameters was evaluated,and the comparison analysis (expressed as the ratio of parameters in late CT to those in the early CT) of different CT time was conducted.RESULTS: Totally 26 patients were in the good-outcome group,while 68 patients were in the poor-outcome group.The putamen density,GWR,and pCSFV in late CT were significantly lower in the poor-outcome group (P<0.05).The ratios of GWR and pCSFV in the poor-outcome group were significantly decreased according to comparison analysis of different CT time (P<0.05),while there was no significant difference in the ratio of putamen density.GWR-basal ganglia <1.18 in late CT showed the best predictive value.The ratio of pCSFV <0.98 predicted unfavorable neurological outcomes with a sensitivity of 65.9% and a specificity of 93.8% (P=0.001).CONCLUSIONS: Brain CT performed >24 h after CA may be a good choice as a neuroimaging approach to evaluating prognosis.To predict neurological prognosis,comparison analysis of different CT time can be used as another promising tool in comatose CA survivors.
KEYWORDS: Cardiac arrest;Brain computed tomography;Cerebral edema;Coma;Prognosis
INTRODUCTION
Sudden cardiac arrest (CA) is critical for its high morbidity and mortality worldwide.Although recent advances in resuscitation strategies such as extracorporeal life support have increased the ratio of CA survivors,only 10.4% of CA patients survive hospitalization,and 8.2% are discharged with good cerebral performance status.Post-CA patients are highly likely to face survival in unresponsive wakefulness or even death resulting from hypoxicischemic brain injury (HIBI).Severe HIBI leads to diffuse cerebral edema and delayed neuronal death.Thus,early prognostication of neurological outcomes may be helpful in making therapeutic decisions and in deciding the proper withdrawal of life-sustaining treatment.
Immediate cerebral computed tomography (CT) is conducted after return of spontaneous circulation (ROSC)for evaluating neurological causes of CA.A previous study has already shown the value of brain CT in predicting unfavorable outcomes.Lopez Soto et altook CT within 24 h after CA into consideration and demonstrated low prediction sensitivities.Few studies have involved CTs from a later time point.The disappearance of the boundary between grey and white matter is the main CT finding in severe HIBI patients,which can be quantified by calculating the grey-towhite matter ratio (GWR) through Hounsfield units (HU).GWR is lower in patients with unfavorable outcomes.In addition,as another objective CT indicator,the proportion of cerebrospinal fluid volume (pCSFV) in the volume of the intracranial component,which is correlated with cerebral edema,can be analyzed using quantitative techniques.A lower pCSFV has suggested more severe brain swelling.
Most retrospective research assessing the predictive value of brain CT concentrates on the post-CA hyperacute period,with images obtained during the first 24 h.However,little is known about the importance of CT performance time and the corresponding changes in GWR and pCSFV in CA survivors.In this study,we aimed to assess the association between relevant brain CT parameters(GWR and pCSFV) at different time and neurological prognosis in adult comatose survivors after CA.
METHODS
Study population
This was a retrospective observational study recruiting patients with CA from January 2018 to April 2020 at the First Affiliated Hospital of Nanjing Medical University.Patients with persistent coma,defined as a Glasgow Coma Scale (GCS) score ≤8 more than 24 h after ROSC,were eligible for inclusion.All eligible patients underwent two rounds of brain CT scans,including early CT (within 24 h after CA) and late CT (24 h to 7 d after CA).Patients under 18 years of age,with terminal malignancy or with baseline neurological disorders were excluded.Furthermore,patients with CT images that indicated parenchymal abnormalities,or that were technically insufficient to determine cerebral density,or that were unavailable for assessment were all excluded.The flow chart of patient enrollment is shown in Figure 1.In total,94 patients were enrolled in this study.According to the Utstein style,data were systematically collected,including age,gender,comorbidities,CA location,bystander cardiopulmonary resuscitation (CPR),etiology of CA,initial rhythm,and time duration from the beginning of CPR to ROSC.The s tudy protocol was granted approval by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2018-SR-356) with a waiver of informed consent.

Figure 1. Flow chart of patient enrollment.
GWR determination and pCSFV analysis
The GWR was determined using the method described in our previous report.All CT scans with a slice thickness of 5 mm were performed using a GE Optima 520Pro scanner (GE Healthcare,Japan).Circular regions (10-15 mm) for measurement were manually placed over the regions of interest (ROIs),which were decided by two expert investigators (WC and XQX).The attenuation values (calculated using HU) of the caudate nucleus (CN),putamen (PU),corpus callosum (CC),and posterior limb of the internal capsule (PLIC) at the level of the basal ganglia were measured.The GWR was calculated as the average of values measured independently by the two investigators.The readers were both blinded to the neurological outcomes and the other reader’s ROI placement,as well as patient data.The inter-rater reliability of GWR was determined using the intra-class correlation coefficient (ICC).
GWR-basal ganglia=(CN+PU)/(CC+PLIC);GWRsimplified=PU/PLIC.
The voxels of the cranium and its outside soft tissues should be eliminated to analyze the CT images’ intracranial components.According to their HU values,the voxels of the foreign body and cranium can be easily eliminated by MATLAB software.The brain extraction tool (BET)function within the FMRIB Software Library (FSL) was applied in order to manage extractions to remove external soft tissue at a fractional strength of 0.01 (supplementary Figure 1).A median filter was used to reduce the noise influence in CT images and improve the signal-to-noise ratio.Generally,the HU value of major intracranial components is not < 0 or > 80,and the cerebrospinal fluid (CSF) HU ranges from 0 to approximately 15.Therefore,intracranial component volume (ICCV) was defined as voxel numbers of HU from 0 to 79,and CSF volume (CSFV) referred to voxel numbers of HU from 0 to 15.Any voxels,which HU values went beyond this boundary condition,were not included,and pCSFV=CSFV/ICCV.
In this study,the changing trends in relevant CT parameters were used for comparison analysis of different CT time in predicting outcomes.They were calculated as the ratio of parameters in late CT to those in the early CT.
Outcomes
The primary endpoint of this study was neurological outcomes at hospital discharge that were evaluated according to the Cerebral Performance Category (CPC) score.The CPC score was as follows: 1=good recovery;2=moderate disability;3=severe disability;4=comatose or unresponsive wakefulness syndrome;and 5=death.The patients were divided into either a good outcome (CPC 1-2) group or a poor-outcome (CPC 3-5) group.
Statistical analysis
The statistical tests were performed using SPSS software,version 23.0 (SPSS Inc.,USA).Descriptive parameters were presented as the mean±standard deviation(SD) or median with interquartile range (IQR) for continuous variables and as counts with percentages (%)for categorical variables.By using-test or Mann-Whitney-test,the comparisons of continuous variables between the two groups were made.The comparisons of categorical variables were made by Chi-square test.In addition,the receiver operating characteristic (ROC) curve was analyzed by its corresponding area under the curve (AUC) with 95%confidence interval ().Based on the maximal sensitivity and specificity,the cut-off values of relevant CT parameters were calculated to predict poor neurological outcomes at hospital discharge.A two-tailed-value <0.05 was considered to be statistically significant.
RESULTS
Clinical characteristics
The baseline characteristics of the involved patients were summarized in Table 1.Totally 26 (27.7%) patients were in the good-outcome group,while 68 (72.3%)patients were in the poor-outcome group based on the CPC score at hospital discharge.In most of the pre-CA baseline variables (age,gender,and comorbidities)and CA characteristics (CA location,cardiac etiology,initial rhythm,and duration of resuscitation),no significant differences were found between the poor-and good-outcome groups,while non-bystander CPR was associated with unfavorable outcomes.
Comparison of GWR and pCSFV between different outcome groups
The inter-rater reliability of GWR showed excellent agreement (ICC 0.77).The GWR-basal ganglia of early CT were significantly lower in the poor-outcome group than in the good-outcome group (<0.05),however,in terms of pCSFV,no significant difference was found between the two groups (=0.824).Table 2 shows in the late CT analysis,thePU density,GWR,and pCSFV were significantly lower in the poor-outcome group (<0.05).
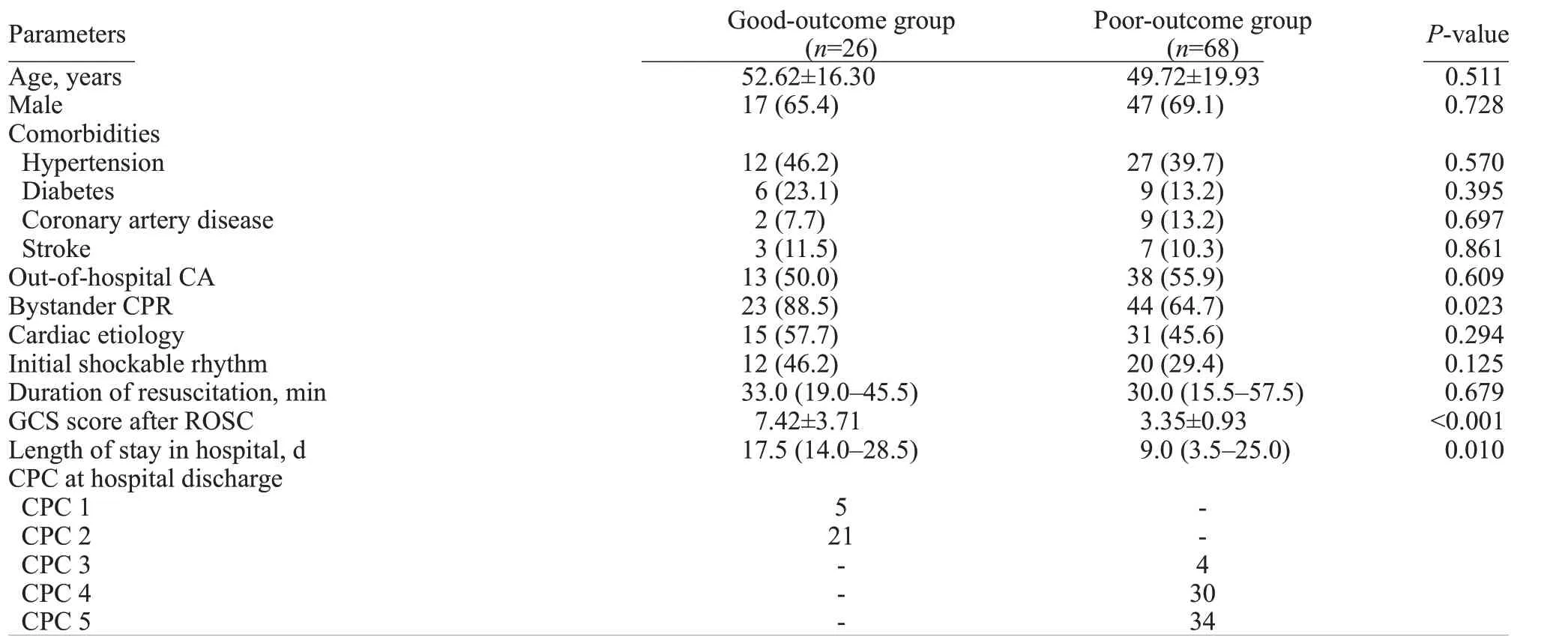
Table 1. Clinical characteristic of enrolled patients

Table 2. Comparison of CT parameters between different outcome groups by early (within 24 h) and late (24 h to 7 d) CTs
Comparison analysis
The ratios of GWR and pCSFV were significantly decreased in the poor-outcome group by comparing the parameters at different CT time (<0.05),while there was no significant difference in the ratio of PU density(>0.05) (Figure 2).

Figure 2. Comparison between different outcome groups in putamen density ratio (A),GWR ratio (B),and pCSFV ratio (C).GWR: grey-white matter ratio;pCSFV: proportion of cerebrospinal fluid volume.
Prognostic performance of relevant CT parameters
The prognostic performances of relevant CT parameters in the prediction of unfavorable outcomes were presented in Table 3.GWR-basal ganglia <1.18 in late CT showed the optimal predictive value (AUC 0.942,95%0.884-0.998,<0.001).Furthermore,a pCSFV <0.03 in late CT predicted unfavorable outcomes,with a sensitivity of 41.5% and a specificity of 100% (=0.010).The pCSFV ratio <0.98 predicted poor neurological outcomes with a sensitivity of 65.9% and a specificity of 93.8% (=0.001).

Table 3. ROC-analysis on the prediction of poor neurological outcome
DISCUSSION
Current guidelines suggest that GWR be applied in predicting poor neurological outcomes.Nevertheless,details including the time of CT scans differ among guidelines.In 2014,the European Resuscitation Council and the European Society of Intensive Care Medicine gave an advisory statement suggesting a significant reduction in GWR within 24 h after ROSC for the prediction of unfavorable prognosis in persistent coma patients following CA.Nevertheless,the 2015 American Heart Association guidelines defined the time when the CT examination should be performed as within 2 h after CA.Though great efforts have been made to apply the findings for prognosis evaluation,initial CTs may not be the best time point.The reason may be that similar to ischemic stroke,tissue changes resulting in changed densities of grey/white matter and in GWR may appear in the duration of hours to days in post-CA survivors,and the immediate post-CA CT image is often normal.A previous studydemonstrated generalized edema on brain CT that was visually detected by radiologists with no formal GWR measurement,with a sensitivity of 14.4% and a specificity of 97.6% for predicting poor outcomes within 24 h after ROSC;the same findings on brain CT performed from 24 h to 7 d after ROSC showed increased sensitivity (56.5%) and specificity (100%).The present study aimed to evaluate time-dependent GWR and pCSFV changes in comatose CA survivors,and both early (within 24 h) and late (24 h to 7 d) CTs were performed on the same patients to exclude a potential selection bias.
Currently,there is no consensus on the time of brain CT for prognostic prediction in post-CA survivors.Differences in the time of the CT and in GWR thresholds,ranging from <1.18 (performed within 48 h)to <1.22 (within 24 h),make it difficult to give an exact recommendation.Furthermore,Hong et alassessed the prognostic value of GWR according to early (within 2 h) and repeated CT (within 7 d) and found that GWR measured by early CT was not a statistically significant predictor of unfavorable outcomes,and the GWRs of repeated CT were significantly lower than those of early CT in poor-outcome patients.Streitberger et alreported that the sensitivity to predict poor outcomes was higher in late CTs (>24 h after CA) compared with that in early CTs(<6 h after CA),as GWR decreased over time in severe HIBI survivors.In addition,under hypoxic conditions,the basal ganglia with high metabolic turnover are one of the first sites to be influenced.It seems that edema is much more severe in the basal ganglia area,particularly in the PU.Similar to these findings,the present study suggested that the GWR-basal ganglia of both early and late CTs,and PU of late CT were significantly lower in the poor-outcome group,as well as a significant increase in the prognostic p erformance of GWR in the late period.
Cerebral edema is a marked feature of HIBI in CA survivors.At the cellular level,non-contrast CT fails to directly observe edema,but it can effectively assess abnormal characteristics,including the formation of edema through pCSFV.As the cranium consists of rigid confines,cerebral edema progress can lead to a decrease in intracranial CSF and blood volume as a result of a compensatory mechanism.The proportion of voxels with CSF-specific attenuation can be a useful tool to evaluate the influence of brain edema and the CSF-volume changes on neurological prognosis.You et alreported similarity between pCSFV prognostic performances that were poor overall and those of GWR.The reason may be that cerebral edema appears to be more prominent 24 h after ROSC.The present study found that GWR and pCSFV decreased significantly over time in patients with poor outcomes,and pCSFV in late CT can be considered a prognostic approach for CA patients.A pCSFV <0.03 predicted poor neurological outcomes with a sensitivity of 41.5% and a specificity of 100%.It is worth mentioning that the brain shows age-related changes,including an overall reduction in brain volume and enlargement of the CSF space.Uncritical application of pCSFV cut-off values from a relatively older population could lead to false pessimistic prognostication in young patients.
Observations of stroke patients demonstrate that water content in the brain increases slowly over hours following the onset of ischemia.When CT was performed in the early period after CA,the prognostic value of CT parameters was low for poor outcome prediction.Furthermore,a previous study showed that the cut-off values differed over various time for poor outcome prediction.Severe HIBI leads to diffuse cerebral edema and delayed neuronal death.A recent neuropathology study indicated a strong link between histopathologically severe HIBI after CA and lower GWR (<1.10).Therefore,the present study described novel metrics to evaluate the trends in relevant CT parameters,i.e.,grey-matter density ratio,GWR ratio,and pCSFV ratio.The GWR and pCSFV ratios were both helpful in predicting poor outcomes.In particular,a pCSFV ratio ≤0.98 corresponded to decreasing pCSFV over the allotted time in poor outcome patients,which showed good specificity and higher sensitivity.The ratio may provide internal local consistency.
Several limitations exist in the present study.Firstly,the single-center location and relatively small sample size may limit generalizability.Secondly,because patients showed poor CPC at hospital discharge that was the primary clinical endpoint,rare cases of good neurological recovery might not be included in the study population despite the presence of cerebral edema in the early period following CA.Thirdly,the brain CT results were known by treating physicians and may have affected clinical decision-making.This may lead to a self-fulfilling prophecy.However,in our hospital,a multimodal approach over a relatively long observation period (at least 7 d) was used for evaluating prognosis and making decisions about the withdrawal of lifesustaining treatment.
CONCLUSIONS
Brain CT performed >24 h after CA may be a good choice as a neuroimaging approach to evaluating prognosis.Comparison analysis of different CT time (performed within 24 h and 24 h to 7 d) can be used as another promising tool to predict neurological outcomes in comatose CA survivors.Dynamic assessment of changes in relevant CT parameters(GWR and pCSFV) yields an improved prognostic value to predict unfavorable outcomes in post-CA patients.
This study was supported by Ruiyi Special Fund for Emergency Medicine Research (R2019019);Postgraduate Research &Practice Innovation Program of Jiangsu Province(SJCX20_0481).
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (No.2018-SR-356).
The authors have no conflicts of interest to declare.
GNW proposed and designed the study.WC and XQX analyzed and interpreted the data.GNW and ZMZ wrote the primary draft of the manuscript.JSZ revised the manuscript.All authors read and approved the final version of the manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World Journal of Emergency Medicine2022年5期
World Journal of Emergency Medicine2022年5期
- World Journal of Emergency Medicine的其它文章
- Intestinal microcirculation dysfunction in sepsis:pathophysiology,clinical monitoring,and therapeutic interventions
- Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study
- Analysis of imaging characteristics of blunt traumatic aortic dissection: an 8-year experience
- Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial
- Arctigenin attenuates paraquat-induced human lung epithelial A549 cell injury by suppressing ROS/p38 mitogen-activated protein kinases-mediated apoptosis
- Hepatocellular carcinoma-derived exosomal miRNA-761 regulates the tumor microenvironment by targeting the SOCS2/JAK2/STAT3 pathway
