Initial venous lactate levels as a predictor of mortality in severe sepsis: a single-center retrospective cohort study
Thidathit Prachanukool,Pitsucha Sanguanwit,Karn Suttapanit Chaiyaporn Yuksen,Piraya Vichiensanth
Department of Emergency Medicine,Faculty of Medicine Ramathibodi Hospital,Bangkok 10400,Thailand
Sepsis is the most common cause of death among critically ill patients.Accordingly,most patients with sepsis are diagnosed and initially treated in the emergency department (ED).Moreover,some studies have shown that early resuscitation is an important determinant of sepsis survival.
Elevated serum lactate levels,which have been observed even during hemodynamic stability,have been considered an important marker of impaired tissue perfusion among sepsis patients.Some studies have established lactate levels as diagnostic,therapeutic,and prognostic indicators of tissue perfusion in sepsis.Previous studies have also shown that elevated blood lactate levels were associated with an increased risk of death.
Increased blood lactate levels have been used to identify critically ill patients at high risk of death even before the development of hemodynamic instability.Scott et alobserved a 3-fold increase in 30-d mortality in children with a venous lactate level >36 mg/dL.Early venous lactate levels assist in the assessment of sepsis severity.Venous lactate levels are able to predict outcomes among patients with sepsis.Venous lactate levels are more manageable and less painful to determine compared to arterial samples.The peripheral venous lactate levels may serve as an alternative to arterial blood lactate measurements to predict in-hospital mortality.
Blood lactate levels can be measured by various devices(central laboratory,point-of-care blood gas analyzer).Most devices used at the bedside have acceptable limits of agreement compared to central laboratory devices.
This study aimed to compare the predictability of venous lactate to other measures,such as arterial lactate,Sequential Organ Failure Assessment (SOFA),quick SOFA (qSOFA),and systemic inflammatory response syndrome (SIRS)criteria,to predict 28-d hospital mortality and morbidity in patients with sepsis admitted to the ED.
METHODS
Study design and setting
This study was a retrospective cohort.A prognostic prediction research study was conducted in the ED,Faculty of Medicine Ramathibodi Hospital,a university-affiliated super tertiary care hospital in Bangkok,Thailand. The Ethics Committee of the Faculty of Medicine,Ramathibodi Hospital,Mahidol University,Bangkok,Thailand,approved this study in terms of Human Rights Related to Research Involving Human Subjects (Ethics code: MURA2017/247,date of IRB approval 22 May 2017).
Inclusion and exclusion criteria
Patients who visited the ED with clinical SIRS determined from the electronic medical record from August 2015 to March 2017 were recruited (Figure 1).

Figure 1. Patient inclusion flow diagram.
The eligible criteria were patients older than 15 years who visited the ED for severe sepsis.According to the Surviving Sepsis Campaign 2012 guideline,severe sepsis was defined as sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to the infection): (1) sepsis-induced hypotension;(2) blood lactate level above the upper limits of the normal laboratory;(3) urine output <0.5 mL/(kg·h) for more than 2 h despite adequate fluid resuscitation;(4) acute lung injury with PaO/FiO<250 mmHg (1 mmHg=0.133 kPa) in the absence of pneumonia as the infection source;(5) acute lung injury with PaO/FiO<200 mmHg in the presence of pneumonia as the infection source;(6) creatinine >2.0 mg/dL;(7) total bilirubin >2 mg/dL;(8) platelet count <100,000/cumm;and(9) coagulopathy (international normalized ratio >1.5).
The exclusion criteria were as follows: (1) not following the sepsis protocol;(2) do-not-attempt resuscitation;or (3)incomplete medical records.
Data collection
The researchers reviewed the medical records in the database software of RAMATHIBODI electronic medical record (EMR).Because this was a retrospective observational cohort study,the researchers did not influence clinical decision-making.The clinicians were blinded to the data collection process.
The potential confounding factors,such as age,sex,comorbidities,information at the ED triage area,initial venous lactate level,and arterial lactate level,were recorded.The qSOFA score and SIRS criteria were calculated from the patient data.Treatments,such as a mechanical ventilator,vasopressors,and time to antibiotic administration,were reviewed from the hospital database.
In the ED,lactate levels were used to screen suspected sepsis patients.Every suspected sepsis patient had serum lactate checked within 20 min of the initial ED physician evaluation.The patients with initial venous lactate levels>4 mmol/L were re-evaluated for arterial lactate levels and analyzed by point-of-care BloodGas GEM 3000 (codei1 sr02971).
Primary and secondary outcomes
The primary outcome of this study was to determine the initial venous lactate level as a predictor of 28-d hospital mortality.The secondary outcomes were defined as a predictor of the vasopressor and mechanical ventilator used within 24 h among patients with sepsis in the ED.
Statistical analyses
Categorical variables are expressed as absolute values and percentages and continuous variables as medians and interquartile ranges (IQRs).Categorical variables were compared using the Chi-square test or Fisher’s exact test when appropriate,while continuous variables were compared using the Mann-Whitney-test.
We used the area under the receiver operating characteristic (AUROC) curve and odds ratio () from logistic regression to assess the initial venous lactate’s ability to determine the primary and secondary outcomes.The model calibration was also evaluated using the Hosmer-Lemeshow test with a-value <0.05 suggesting imperfective calibration and the observed-to-expected (O/E) ratio with a ratio of 1 indicating perfect calibration.Correlations between venous and arterial lactate levels were also presented using the equation.We used Stata version 14.0 (StataCorp LP.,USA) for statistical analyses.
RESULTS
Demographic and descriptive data
The demographic and descriptive data of the 460 included patients are listed in Table 1.Non-survivors had higher initial venous lactate levels (median,5.9 mmol/L vs.4.0 mmol/L;=0.001).
Univariate and multivariate analyses
Univariate analysis revealed odds ratios of 1.19 (95% confidence interval [] 1.12-1.27) for initial venous lactate level,2.31 (95%1.74-3.06) for qSOFA score,0.65 (95%0.42-0.97) for hypertension,1.12 (95%0.85-1.22)for active malignancy,and 1.57 (95%1.22-1.7) for respiratory tract infection (supplementary Table 1).
Multivariate analysis identified initial venous lactate(adjusted1.17,95%1.09-1.24) and qSOFA score(adjusted2.12,95%1.58-2.83) as independent factors for 28-d hospital mortality (supplementary Table 1).
Performance of initial venous or arterial lactate
The performance of initial venous lactate and initial arterial lactate for predicting outcomes is presented in Table 2.
The initial venous lactate level had a modest ability to predict vasopressor administration within 24 h of ED arrival;however,it had a poor ability to predict mechanical ventilator use within 24 h after ED arrival (Table 2).

Table 1. Demographic and descriptive data of the included patients
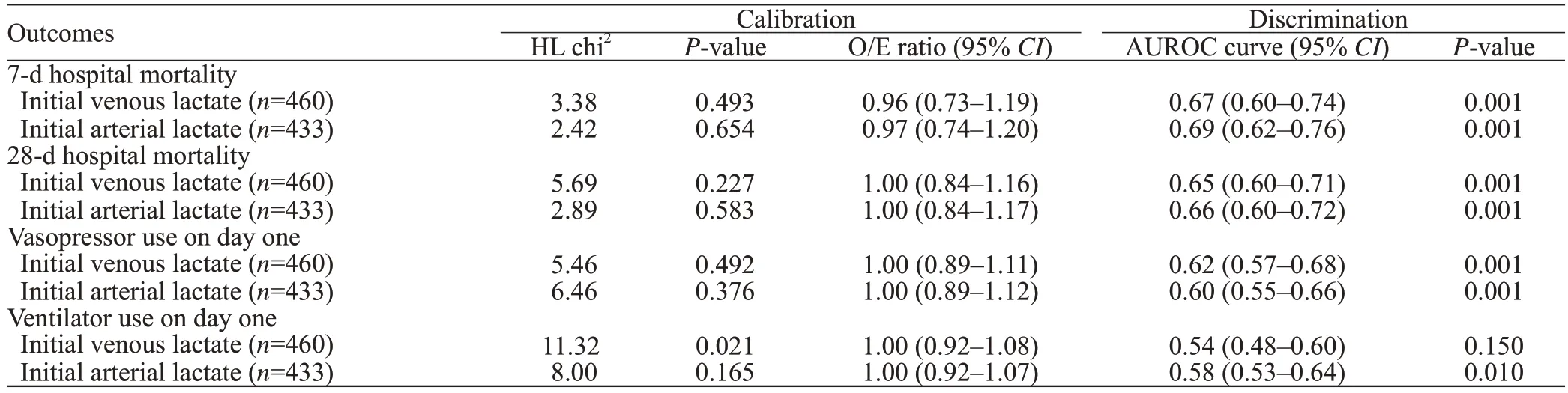
Table 2. Performance of initial venous lactate and initial arterial lactate for predicting outcomes
The Hosmer-Lemeshow test for initial venous lactate and arterial lactate levels was not significant.The O/E ratio was near 1,indicating good calibration and the ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h.
The ability of the initial venous lactate level to discriminate between survivors and non-survivors after 28 d was not inferior to that of the qSOFA score and SIRS criteria (supplementary Figure 1).There was no significant difference in the ability to predict mortality between the initial venous lactate level and the qSOFA score (=0.89) or SIRS criteria (=0.4).
DISCUSSION
In a recent study conducted in Thailand,Musikatavorn et alreported that a single measurement of initial venous lactate was not associated with 30-d mortality.However,the study included non-elderly patients with sepsis who had hemodynamic stability.In another study in Thailand,Permpikul et alreported that patients with severe sepsis and septic shock who had an initial lactate level >2 mmol/L suffered higher mortality (43.6%).The study did not indicate whether the initial lactate measurements were arterial or venous.Our study showed that the initial venous lactate level could predict 7-d and 28-d hospital mortality among patients with severe sepsis with or without shock.Moreover,no significant difference was observed between the initial venous lactate level and arterial lactate level in their ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h.However,our results showed that the initial venous lactate level was not associated with mechanical ventilator use within 24 h.Our study found that only respiratory tract infections,such as pneumonia,bronchitis,and tracheobronchitis,were independent factors associated with mechanical ventilator use during the first day (adjusted4.76,95%2.97-7.63,adjusted by qSOFA,initial venous lactate,COPD,time to antibiotic and systolic blood pressure).
Many prognostic scores have been developed and usedto predict the risk of death and early resuscitation for patients with sepsis to reduce mortality rates.The qSOFA score and SIRS criteria have been easy to use in the ED.Previous studies have shown that the qSOFA score has an excellent ability to predict mortality among patients with sepsis both inside and outside the intensive care unit.Another study,however,showed that the qSOFA score failed to detect severe sepsis and had a more inferior ability to predict mortality compared to SIRS criteria.
The present study showed that initial venous lactate’s ability to discriminate between survivors and non-survivors within 28 d was not inferior to that of the qSOFA score and SIRS criteria.Multivariate analysis showed that the initial venous lactate level and qSOFA score were independent predictors of 28-d mortality.
This study has some limitations.This study was a retrospective study conducted in a single center.ED overcrowding and the availability of hospital admission to definite treatment may have affected patient outcomes.The information bias of the reviewer may be our limitation.
CONCLUSIONS
Initial venous lactate levels may have a modest ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h during severe sepsis.Moreover,no significant differences in the ability to predict 7-d and 28-d hospital mortality were observed between the initial venous lactate level and the qSOFA score or SIRS criteria.
None.
The Ethics Committee of Faculty of Medicine,Ramathibodi Hospital,Mahidol University,Bangkok,Thailand,approved this study in terms of Human Rights Related to Research Involving Human Subjects (Ethics code: MURA2017/247,date of IRB approval 22 May 2017).
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
TP wrote the first draft.All authors contributed to the design and interpretation of the study and to further drafts.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World Journal of Emergency Medicine2022年5期
World Journal of Emergency Medicine2022年5期
- World Journal of Emergency Medicine的其它文章
- Intestinal microcirculation dysfunction in sepsis:pathophysiology,clinical monitoring,and therapeutic interventions
- Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study
- Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study
- Analysis of imaging characteristics of blunt traumatic aortic dissection: an 8-year experience
- Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial
- Arctigenin attenuates paraquat-induced human lung epithelial A549 cell injury by suppressing ROS/p38 mitogen-activated protein kinases-mediated apoptosis
