Posterior lamellar tarsorrhaphy in the early treatment of severe eyelid trauma/burns
Neelam Pushker,Deepsekhar Das,Sujeeth Modaboyina,Pallavi Singh,Sahil Agrawal
Oculoplasty &Pediatric Ophthalmology Services,Dr Rajendra Prasad Centre for Ophthalmic Sciences,All India Institute of Medical Sciences,New Delhi 110029,India
In patients with lagophthalmos due to eyelid trauma,it is imperative to ensure adequate closure of the eye to protect the ocular surface.Sometimes it is difficult to surgically close eyelids by conventional methods of tarsorrhaphy,such as intermarginal suture tarsorrhaphy,Week’s tarsorrhaphy,and tongue-in-groove tarsorrhaphy.We need intact eyelid tissues to perform these procedures and might not be possible in patients with severe lagophthalmos due to lost/damaged eyelid tissues either due to deficient length of tissues or increased tension at the wound site,which can result in surgical failure.
Patients with acute presentation of injury with extensive eyelid and periorbital trauma usually have associated tissue loss and ocular surface injury.An attempt to perform definitive surgery for eyelid reconstruction using grafts and/or flaps,as an emergency procedure,is not always feasible or,if done,can result in more damage to the tissues because of high failure rates.Herein,we describe posterior lamellar tarsorrhaphy (PLT),a novel and simple surgical approach that can be performed as an emergency procedure to protect the ocular surface in acute presentation of patients with severe lagophthalmos following extensive trauma/burns.
METHODS
This was a retrospective study of patients with early presentation to eye emergency with severe lagophthalmos due to extensive eyelid and periorbital burns or trauma who underwent PLT at our center between October 2018 and December 2020.The study adhered to the guidelines of the,and written informed consent was obtained.
Eight patients,all males with ages ranging from 8 to 63 years,were included.Trauma was due to thermochemical injury in 4 patients,road traffic accidents in 3 patients,and electrocution injury in 1 patient.Except 2 patients who presented on day 4 and day 10 after trauma,the remaining 6 patients were operated on within 24 h of injury.Three patients had bilateral involvement,3 had right eye involvement,and 2 had left eye involvement.In patients with bilateral involvement,only 1 patient underwent PLT for both eyes.Of them,1 patient had mild lagophthalmos,and the other patient had severe injury with hypotonus globe and no visual prognosis in the second eye,so only one eye underwent PLT.Therefore,a total of 9 eyes underwent PLT in our study.
RESULTS
In the 9 operated eyes,visual acuity at presentation was < 1/60 in 6 eyes,3/60 in 1 eye,6/18 in 1 eye,and 1 child with bilateral trauma was not cooperative for vision assessment.All patients had severe trauma to the eyelids,with lagophthalmos in 9 eyes (14.0±4.7 mm) and ocular surface injury in all eyes.Anterior lamellar tissue was swollen and friable,with areas of nonviable tissue and/or loss in 15 out of 18 (83.33%) eyelids (9 eyes).At least 1 eyelid margin was lost in all the operated eyes,and both eyelid margins were lost in 6 eyes.Complete absence of upper and lower eyelid anterior lamellar tissues was found in 3 eyes along with loss of posterior lamella until fornix in 2 patients and partial loss of posterior lamella in 1 patient.Six eyes had partial loss of anterior lamella with preserved posterior lamellar tissues.Extensive periorbital injury was present in all operated eyes,and full-face burns were present in two cases,with one of them having 45% total burn surface area (TBSA).
Exposure keratopathy was present in all operated eyes,with epithelial defects and infiltration in 6 eyes,limbal ischemia in 3 eyes,and corneal melt in 2 eyes.Reconstruction using a flap or grafting procedure did not seem to be a viable option in these patients.PLT was performed as an eye-saving procedure.In addition,periorbital laceration repair surgery was performed in 4 patients,and amniotic membrane grafts of both eyes were performed in 1 patient.
PLT was performed by splitting the anterior and posterior lamellae by incision at the gray line or skinconjunctival junction in patients with lost eyelid margins.The incision was made in the central part,aiming for closure of at least half of the horizontal aperture.The margins of the posterior lamellae (tarso conjunctiva) of upper and lower eyelids were made raw by excising 1 mm of margin tissues.In the lower eyelid,dissection was extended deep until the lower border of the tarsus,and the posterior lamellar flap was mobilized by giving medial and lateral vertical cuts until the lower tarsal border and advanced (Figures 1 A and B).The raw margins of both the posterior lamellae were brought together,and if found under tension,then a similar mobilization and advancement of the posterior lamellar flap of the upper eyelid was also carried out.The raw surfaces of the posterior lamellae were sutured together using interrupted 6-0 polyglactin sutures (Figures 1 C and D).The traumatized/deficient anterior lamellae were left to heal with secondary intention.The sutures were removed after 10 d.Postoperatively,all patients were advised to use topical lubricants and antibiotics.Depending on the extent of injury,other supportive treatment was also given.Split-thickness skin grafting of the abdomen,both thighs and right forearm,was performed in 1 patient who had associated 45% TBSA.
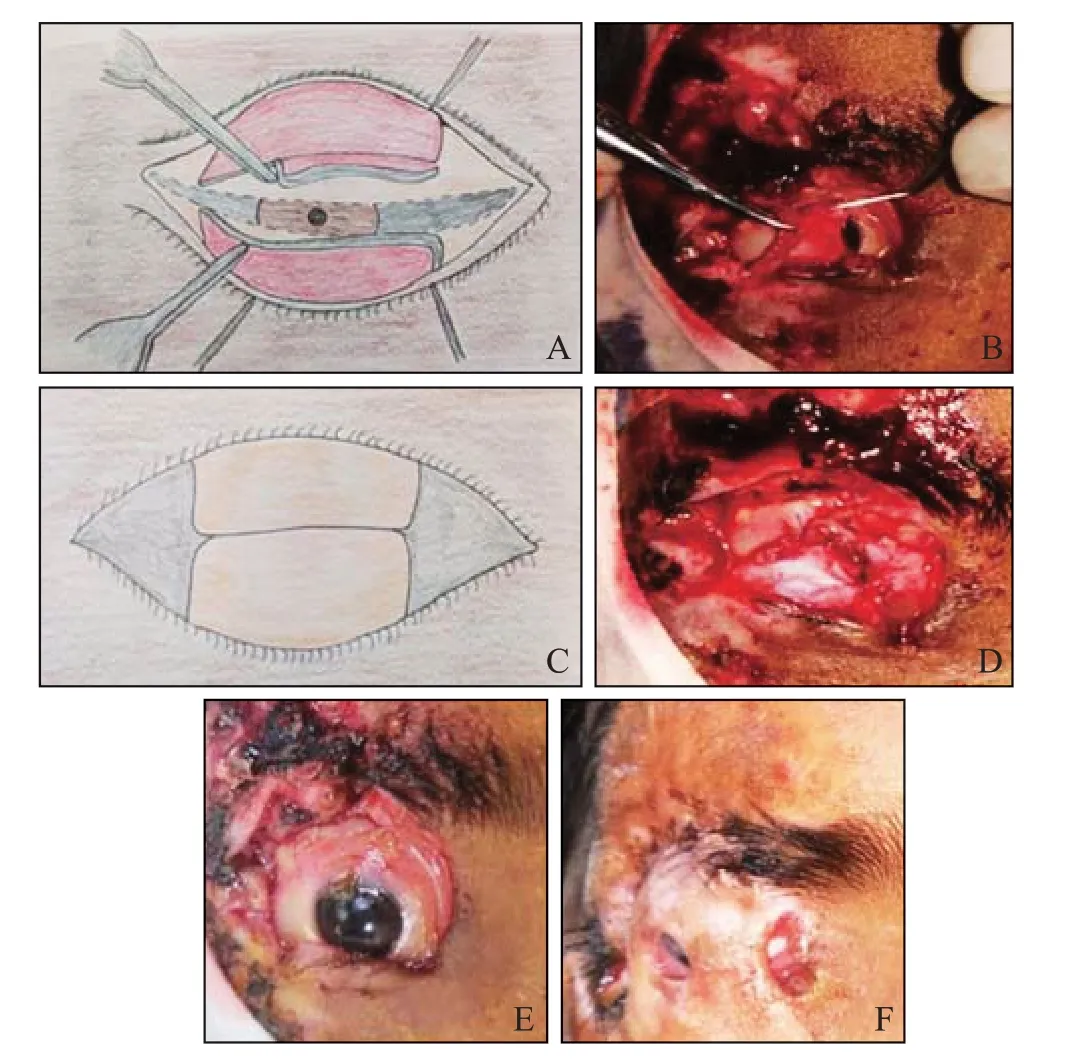
Figure 1. Illustration of the surgical technique.A: sketch diagram shows advancement of posterior lamellae after splitting the eyelid margins and giving vertical lateral and medial cuts until borders of the tarsal plates in upper and lower eyelids,respectively;B: clinical photograph shows advancement of posterior lamellar flap of lower eyelid after giving medial and lateral vertical cuts till the lower tarsal border;C: sketch diagram shows the raw margins of both the posterior lamellae brought together and sutured using interrupted sutures;D:clinical photograph of same patients with upper and lower posterior lamellar flaps being advanced and sutured together using interrupted 6-0 polyglactin sutures;the traumatized/deficient anterior lamellae were left as such to heal with secondary intention;E: preoperative picture showing full thickness loss of upper and partial loss of lower lid with residual lid margin tissues,laterally with periorbital laceration wound with tissue loss and eschar formation;F: intact posterior lamellar tarsorrhaphy at 3-month follow-up in the same patient.
On follow-up,ocular surface symptoms resolved,and corneal re-epithelialization was achieved within 4-6 weeks in all patients.A patient with thermochemical injury and severe ocular surface injury had limbal ischemia with complete epithelial defect and infiltration,vision was light perception in oculus dexter (OD) and total corneal melt with no light perception in oculus sinister(OS).He underwent amniotic membrane grafting with PLT as a primary procedure in both eyes;at the 3-week follow-up,corneal grafting with resuturing of PLT was performed in both eyes.His vision recovered to 6/60 OD with PLT in place,and he had no vision OS at the 6-month follow-up.In the rest of the operated eyes,visual acuity improved to > 6/18 in 6 eyes and 6/60 in 1 eye.Four eyes underwent full-thickness skin grafting for cicatricial ectropion and lagophthalmos as a secondary procedure at a mean follow-up duration of 5.4±0.7 months.The mean follow-up duration of patients in our study was 6.5±3.4 months (range 3-15 months).At the last follow-up,out of 9 operated eyes,5 eyes had partial corneal opacity,3 eyes had clear cornea,and 1 eye with total corneal melt at presentation went into phthisis bulbi.None of the patients required a repeated tarsorrhaphy procedure or had a nonhealing epithelial defect or progression to corneal melt/perforation.Three eyes are still awaiting skin grafting procedures due to the COVID-19 pandemic.
DISCUSSION
Eyelid trauma/burns account for approximately 65% of facial trauma,and 15% of these patients become blind if not treated in a timely manner.An important aspect in the early management of eyelid trauma is to ensure adequate closure and lubrication of the ocular surface,which prevents as well as halts exposure and trauma-related corneal complications.Studies show that surgeons prefer to perform primary reconstruction with grafts and/or flaps in burns/trauma patients,instead of tarsorrhaphy.In most of these reports,the intervention was performed within 2-4 weeks of presentation.The main reason for avoidance of permanent tarsorrhaphy was that the procedure can lead to eyelid margin irregularity,trichiasis,entropion,etc.In contrast,Frank et almentioned the use of tarsorrhaphy in some unavoidable situations with severe eyelid damage.Delayed reconstructive procedures are known to have disadvantages of hypertrophic scarring and deformities,whereas advantages are better planning and success of a full-thickness graft.
In acute presentation of patients with severe lagophthalmos due to eyelid and periorbital trauma,where a flap cannot be raised and/or if the recipient eyelid bed has friable and ischemic tissues with tissue loss,the primary reconstructive procedure using grafts and/or flaps becomes difficult.In this small subset of patients,tarsorrhaphy remains the mainstay of emergency care for protection of the ocular surface.All our patients had associated damage to one or both eyelid margins with other surrounding tissue involvement,as already mentioned,where damage to the anatomy of the eyelid margin because of the procedure was not the main concern.The technique resulted in a strong fusion because the posterior lamellar flaps were mobilized free and the wound was not under tension.Furthermore,we achieved adequate ocular surface coverage that led to healing of the cornea with useful visual recovery in most of the patients.We observed that the posterior lamella,being a hidden part of the eyelid,was less damaged/deficient than the anterior lamella because we could advance it freely with our technique.
Previous reports are available on mobilization of remaining conjunctiva from the eyelid and fornices and suturing them together,and even a study describes advancement of levator muscle along with skin graft to cover the ocular surface in patients with severely traumatized/loss of eyelid tissues.
CONCLUSIONS
PLT provides adequate coverage of the ocular surface,which remains a priority over iatrogenic damage by the procedure in the acute presentation of patients with severe lagophthalmos due to loss of eyelid and periorbital tissues where primary repair or reconstructive procedures are difficult or not possible.It is not a procedure of choice over other less damaging procedures of tarsorrhaphy or in cases where it can be completely avoided.
ACKNOWLEDGMENT
We would like to thank Dr Saloni Gupta,Northern Railway Central Hospital,New Delhi,for her assistance in the hand-drawn diagrams illustrating the surgical technique.
None
The study was approved by Ethics Board of Dr Rajendra Prasad Centre for Ophthalmic Sciences,All India Institute of Medical Sciences,and written informed consent was obtained.
There are no conflicts of interest.
NP: conceived and designed the work and did final approval;DD: data analysis and interpretation;SM: literature search and manuscript draft review;PS: critical revision and data acquisition;SA: wrote the manuscript and acted as a gurantor.
 World Journal of Emergency Medicine2022年5期
World Journal of Emergency Medicine2022年5期
- World Journal of Emergency Medicine的其它文章
- Intestinal microcirculation dysfunction in sepsis:pathophysiology,clinical monitoring,and therapeutic interventions
- Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study
- Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study
- Analysis of imaging characteristics of blunt traumatic aortic dissection: an 8-year experience
- Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial
- Arctigenin attenuates paraquat-induced human lung epithelial A549 cell injury by suppressing ROS/p38 mitogen-activated protein kinases-mediated apoptosis
