Clinical observation of warm needling moxibustion plus lumbar traction for lumbar disc herniation
DAI Jifeng (戴基凤)
Mingguang Hospital of Traditional Chinese Medicine, Anhui Province, Chuzhou 239400, China
Abstract
Keywords: Acupuncture Therapy; Warm Needling Therapy; Traction; Point, Jiaji (EX-B2); Intervertebral Disc Displacement;Low Back Pain
Lumbar disc herniation (LDH) is a common disease in the department of acupuncture and Tuina (Chinese therapeutic massage). It is mainly manifested as low back and lower-limb pain, numbness of one or both lower limbs, and even incomplete paralysis of both lower limbs and uncontrolled stool and urination in severe cases, seriously affecting the quality of life of patients[1-2]. LDH is mostly caused by the deformation and rupture of the annulus fibrosus of the intervertebral disc, leading to the protrusion or prolapse of the nucleus pulposus tissue, which stimulates or compresses the adjacent spinal nerve roots. It is a syndrome of a series of clinical symptoms[3-4]. The symptoms of LDH are usually lingering and require long-term treatment, which affects patients’ life and work. Therefore, a safe and effective treatment protocol is urgently needed[5]. Clinical practice guidelines have recommended non-surgical treatments for LDH, mainly including physical therapy, lumbar traction, and analgesic drugs[6-8]. In this study, we observed the curative efficacy of warm needling moxibustion plus lumbar traction for LDH.
1 Clinical Materials
1.1 Diagnostic criteria
This study referred to the diagnostic criteria in theLumbar Disc Herniation[9]: patients with different degrees of lumbar pain and lower limb radiating pain,and were confirmed by lumbar spine CT.
1.2 Inclusion criteria
Those who met the diagnostic criteria of LDH; had no LDH-related treatments within at least one month before enrollment; patients and their families agreed to participate in this trial and signed informed consent.
1.3 Exclusion criteria
Patients with osteoporosis, lumbar spondylolisthesis or fracture; combined with spinal cord compression or cauda equina compression; those with vertebral tumor or vertebral body tuberculosis; those who with a history of spinal surgery; those with severe diseases of heart,brain, liver, kidney, or hematopoietic systems.
1.4 Dropout criteria
Those who failed to complete the prescribed course of treatment; who did not strictly follow the treatment protocol; those who got worse in the disease condition during treatment or developed complications and needed to change the treatment; those who took medication by themselves that affected efficacy evaluation; those who dropped out during the trial.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 25.0 statistical software. All measurement data in this study were in normal distribution and expressed as mean ± standard deviation (±s). Independent samplet-test was applied to the comparisons between groups. Paired samplet-test was applied to the comparisons of intra-group data. Counting data were expressed as numbers of cases or percentages and analyzed by Chi-square test.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
This study followed the Helsinki Declaration and was reviewed and approved by the Ethics Committee of the Mingguang Hospital of Traditional Chinese Medicine,Anhui Province (Approval No. 201805-16). A total of 146 patients with LDH were enrolled in the Acupuncture and Tuina Department of our hospital between June 2018 and December 2019. All patients were divided into a combination group and a control group by the random number table, with 73 cases in each group.There were no dropout cases in this trial. There were no statistically significant differences in the general data between the two groups (P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Comparison of general data between the two groups
2 Treatment Methods
2.1 Combination group
The combination group was treated with lumbar traction plus warm needling moxibustion.
2.1.1 Lumbar traction
The patient took a supine position. The lumbar traction sleeve was fixed moderately tight on the waist and hip of the patient to perform the lumbar traction.The weight of traction started from a small amount,generally about 1/3 of the patient’s body weight. The traction weight was then gradually increased according to the patient’s tolerance. After the traction, the patient took a 5-minute rest and then got off the traction bed.The traction took 30 min each time and was performed once a day, with a 2-day break after consecutive 5 times.The treatment continued for three weeks.
2.1.2 Warm needling moxibustion
Points: Lumbar Jiaji (EX-B2) on the affected side,bilateral Chengshan (BL57), Huantiao (GB30), Weizhong(BL40), and Kunlun (BL60).
Methods:After routine disinfection of the above points areas, acupuncture needles of 0.30 mm in diameter and 50-75 mm in length were used for the acupuncture treatment. After the arrival of Qi (Deqi), a moxa stick of 20 mm in diameter and about 1 cm in length (about 1.25 g in mass) was fixed on the needle handle at the above points and ignited. The moxa stick was 3 cm away from the skin, and meanwhile, a layer of heat insulation paper was laid on the skin of the above points. The temperature should be tolerable. Each point was treated with two moxa cones. The needles were retained for 30 min. The treatment was performed once a day for 20 consecutive times.
2.2 Control group
The control group only received the same lumbar traction as the combination group. The treatment frequency and time were the same as those in the combination group.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Lumbar function
Oswestry disability index (ODI) score[10]and Japanese Orthopaedic Association (JOA) score[11]were used to evaluate the lumbar function of the patients at grouping and by the end of the treatment, respectively.The ODI scale contained 10 items, and each item had a score ranging from 0 to 5 points, with a maximum of 50 points. The higher the score, the severer the lumbar dysfunction. The JOA score was mainly composed of subjective judgment, clinical signs, and daily life, with a maximum score of 29 points. The higher the score, the better the lumbar function of patients.
3.1.2 Pain condition[12]
Present pain intensity (PPI) score was used to assess the degree of lumbar pain and lower-limb pain of patients before and after treatment. The score was divided into six grades, scored 0, 1, 2, 3, 4, and 5 points,respectively. The higher the score, the severer the pain.
3.1.3 Inflammatory factor levels
The elbow venous blood was collected before treatment and on the day after treatment, centrifuged,and the supernatant was collected. The levels of serum tumor necrosis factor (TNF)-α and interleukin (IL)-6 were detected by the enzyme-linked immunosorbent assay. The higher the level, the severer the inflammatory response of patients.
3.1.4 Degree of straight leg raising[13]
The objective signs of patients were evaluated by the straight leg raising test before and after treatment,based on the straight leg raising level of the leg with comparatively severer symptoms. Straight leg raising angle ≥70° was normal, scored as 0 points; straight leg raising angle ≥46°, but <70°, scored 2 points; straight leg raising angle ≥15°, but <46°, scored 4 points; and straight leg raising angle <15°, scored 6 points.
3.2 Criteria of curative efficacy
According to the criteria of curative efficacy for LDH in theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[14], the curative efficacy was assessed.
Markedly effective: After treatment, clinical symptoms such as lumbar pain and lower-limb pain disappeared, the straight leg raising angle was ≥70°, and daily life and work were normal.
Effective: After treatment, clinical symptoms such as lumbar pain and lower-limb pain were significantly improved, and the straight leg raising angle was <70°.There were still mild disorders in the lumbar activities,which basically did not affect daily life or work.
Invalid: After treatment, there were no improvements in the clinical symptoms of patients, and straight leg raising was a mission impossible, with obvious disorders in the lumbar activities, seriously affecting the daily life and work.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The total effective rate was 93.2% in the combination group and 78.1% in the control group. The difference between the two groups was statistically significant(P<0.05). It is shown in Table 2.

Table 2. Comparison of the clinical efficacy between the two groups (case)
3.3.2 Comparison of the lumbar function
Before treatment, there were no significant differences in the scores of ODI or JOA between the two groups (P>0.05). After treatment, the ODI score in both groups decreased and the JOA score increased (P<0.05),and the intra-group differences before and after treatment were statistically significant (P<0.05). After treatment, the ODI score in the combination group was lower than that in the control group and the JOA score was higher than that in the control group. The differences between the groups were statistically significant (P<0.05). It is shown in Table 3.
3.3.3 Comparison of the lumbar pain and lower-limb pain
Before treatment, there were no significant differences in the PPI scores of lumbar pain and lower-limb pain between the two groups (P>0.05).After treatment, the PPI scores of lumbar pain and lower-limb pain in both groups decreased significantly(P<0.05), and the PPI scores in the combination group were lower than those in the control group (P<0.05). It is shown in Table 4.
3.3.4 Comparison of the serum inflammatory factor level
Before treatment, there were no significant differences in the serum TNF-a or IL-6 levels between the two groups (P>0.05). After treatment, the serum TNF-a and IL-6 levels in both groups decreased (P<0.05),and the serum TNF-a and IL-6 levels in the combination group were lower than those in the control group(P<0.05). It is shown in Table 5.
3.3.5 Comparison of the straight leg raising test score Before treatment, there was no significant difference in straight leg raising test score between the two groups(P>0.05). After treatment, the straight leg raising test scores in both groups decreased (P<0.05), and the score in the combination group was lower than that in the control group (P<0.05). It is shown in Table 6.
Table 3. Comparison of the lumbar function score between the two groups ( ±s point)
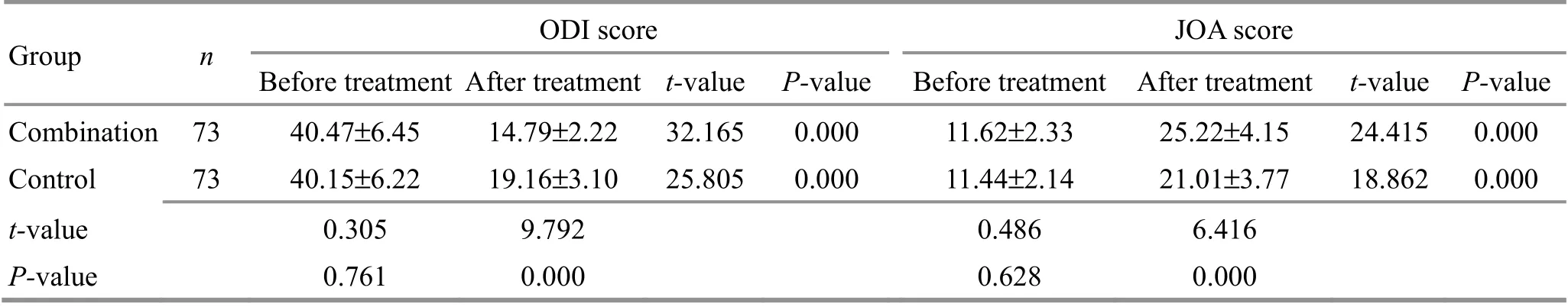
Table 3. Comparison of the lumbar function score between the two groups ( ±s point)
Note: ODI=Oswestry disability index; JOA=Japanese Orthopaedic Association
Group n ODI score JOA score Before treatment After treatment t-value P-value Before treatment After treatment t-value P-value Combination 73 40.47±6.45 14.79±2.22 32.165 0.000 11.62±2.33 25.22±4.15 24.415 0.000 Control 73 40.15±6.22 19.16±3.10 25.805 0.000 11.44±2.14 21.01±3.77 18.862 0.000 t-value 0.305 9.792 0.486 6.416 P-value 0.761 0.000 0.628 0.000
Table 4. Comparison of the lumbar pain and lower-limb pain between the two groups ( ±s point)

Table 4. Comparison of the lumbar pain and lower-limb pain between the two groups ( ±s point)
Note: PPI=Present pain intensity
Group n PPI score of the lumbar pain PPI score of the lower-limb pain Before treatment After treatment t-value P-value Before treatment After treatment t-value P-value Combination 73 4.32±0.82 1.28±0.29 29.863 0.000 4.10±0.71 1.14±0.31 32.644 0.000 Control 73 4.24±0.77 1.97±0.41 22.233 0.000 4.02±0.63 1.88±0.50 22.733 0.000 t-value 0.608 11.739 0.720 10.747 P-value 0.544 0.000 0.473 0.000
Table 5. Comparison of serum inflammatory factor level between the two groups ( ±s)

Table 5. Comparison of serum inflammatory factor level between the two groups ( ±s)
Note: TNF=Tumor necrosis factor; IL=Interleukin
?
Table 6. Comparison of the straight leg raising test score between the two groups ( ±s point)

Table 6. Comparison of the straight leg raising test score between the two groups ( ±s point)
Group n Before treatment After treatment t-value P-value Combination 73 3.46±0.75 1.23±0.31 23.478 0.000 Control 73 3.38±0.80 1.72±0.43 15.616 0.000 t-value 0.623 7.898 P-value 0.534 0.000
4 Discussion
In recent years, the incidence of LDH in China has been on the rise, and it tends to be younger[15]. At present, there are many treatment methods for LDH,such as medications and surgical treatment, which have certain effects but are prone to adverse reactions, and surgeries have certain risks. Clinically, safe and effective treatment options for LDH still need to be explored.
Traditional Chinese medicine believes that the pathogenesis of LDH is mainly liver-kidney deficiency, Qi stagnation and blood stasis, cold-damp stagnation and congelation, and meridian blockage. Therefore, the key to treatment lies in promoting blood circulation,removing blood stasis, and unblocking meridians[16]. In this study, we applied warm needling moxibustion plus lumbar traction for the treatment of LDH. The warm needling moxibustion could improve local blood and lymph circulation and reduce sensory nerve excitation and intramuscular tone[17]. Jiaji (EX-B2) were used as the primary points in this study, combined with Chengshan(BL57), Huantiao (GB30), Weizhong (BL40), and Kunlun(BL60), which have effects of unblocking meridians and activating collaterals, and reducing swelling for relieving pain, to effectively relieve pain and reduce clinical symptoms of the low back and lower limbs[17].
In this study, it was found that the total effective rate of warm needling moxibustion plus lumbar traction was significantly higher than that of the control group. After treatment, the lumbar ODI scores of patients in both groups decreased, and the JOA scores increased. The changes in ODI and JOA scores in the combination group were more significant, suggesting that the efficacy of the combination group is superior to that of the control group. The study of DOU Q H[18]found that warm needling moxibustion at lumbar Jiaji (EX-B2)could improve quality of life and reduce pain score in patients with LDH, and improve their physical,psychological, and social functions. In this study, the lumbar and lower-limb PPI scores after treatment in the combination group were significantly lower than those in the control group, which was the same as the previous study, indicating that warm needling moxibustion at Jiaji (EX-B2) can relieve pain in patients with LDH. Further comparison of the straight leg raising test score showed that the straight leg raising test score in the combination group was significantly lower than that in the control group after treatment, indicating that warm needling moxibustion at Jiaji (EX-B2) can help the recovery of leg function in patients with LDH.
Inflammatory cytokines are closely related to the occurrence and development of LDH. IL-6 and TNF-α are both pro-inflammatory factors. A study found that IL-6 and TNF-α were associated with neuropathic pain in patients with LDH and involved in the inflammatory process of lumbar intervertebral disc degeneration[19].The study of CUI J M[20]found that warm needling moxibustion could significantly reduce the serum levels of IL-6 and TNF-α and relieve pain in patients with LDH.In this study, the serum levels of TNF-α and IL-6 in both groups after treatment were lower than those before treatment. And the serum levels of TNF-α and IL-6 in the combination group were lower than those in the control group, indicating that warm needling moxibustion at Jiaji (EX-B2) plus lumbar traction has better effects in improving inflammatory symptoms,reducing inflammatory responses, and relieving pain for patients with LDH than lumbar traction alone.
In summary, warm needling moxibustion plus lumbar traction is effective in the treatment of LDH. It can significantly improve the lumbar function of patients,relieve pain, and reduce inflammatory responses, and thus is worthy of clinical promotion.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project fund support for this study.
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 14 May 2021/Accepted: 18 August 2021
 Journal of Acupuncture and Tuina Science2022年4期
Journal of Acupuncture and Tuina Science2022年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Study on the mechanism of moxibustion for rheumatoid arthritis based on liquid chromatography-mass spectrometry
- Study on the relationship between relieving energy crisis in myofascial trigger points with An-Pressing manipulation and AMPK/PGC-1α pathway activation
- Regulatory effect of acupuncture on electrical activity level of optic cortex in amblyopia model rats
- Influence of Tuina plus oxiracetam on serum inflammatory factors and oxidative stress in mild vascular dementia patients
- Effects of acupuncture on nutritional status in patients in a persistent vegetative state:a prospective randomized controlled study
- Clinical observation of acupuncture plus acupoint sticking therapy for insomnia and its influence on subjective and objective sleep indicators
