Clinical observation of acupuncture plus acupoint sticking therapy for insomnia and its influence on subjective and objective sleep indicators
XIE Chen (谢晨), ZHENG Yixin (郑益鑫), LI Jinjin (李金金), FANG Chaojun (方超君), CHEN Yunfei (陈云飞)
1 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
2 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
Abstract
Keywords: Acupuncture Therapy; Acupoint Sticking Therapy; Pittsburgh Sleep Quality Index; Liver-Qi Stagnation and Spleen Deficiency; Insomnia
Sleep is significant in maintaining a normal life.Insomnia is far more than only a sleep problem. It also affects daytime functions, hindering memory and concentration, and may result in other medical conditions such as depression[1]. Insomnia can occur in any age group, and the onset age gets younger and younger as society develops[2-3]. Research shows that China has a lower prevalence rate of insomnia than Western countries but is parallel to other Asian countries; young Chinese are more likely to be affected than the aged[4]. On the other hand, insomnia can be a secondary symptom of other diseases, and the incidence of secondary insomnia has been rising year after year, e.g., pain-induced insomnia[5]and post-stroke insomnia[6]. The treatment of insomnia includes pharmaceutical and non-pharmaceutical treatments.The former can be divided into Chinese medication and Western medication. Sedative and sleeping pills are the main Western medication used for insomnia but may lead to adverse reactions to a different extent[7].Acupoint sticking is a unity of both medication and acupoint and has been proven effective for kinds of diseases[8-10]. In this study, we adopted acupoint sticking therapy of different dosages and treatment durations to treat insomnia based on the same acupuncture intervention and observed the changes in sleep indicators via actigraphy to evaluate sleep quality in combination with sleep-related scales. The report is as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The diagnostic criteria for insomnia in theInternational Classification of Sleep Disorders-Third Edition(ICSD3)[11]stipulated by the American Sleep Disorders Association (ASDA) were referred.
1.1.2 Syndrome differentiation standard in traditional Chinese medicine (TCM)
We adopted the syndrome differentiation standard for liver-Qi stagnation and spleen deficiency in theGuiding Principles for Clinical Study of New Chinese Medicines[12]. The major symptoms are distending pain in the stomach or hypochondrium, abdominal bloating,reduced food intake and poor appetite, and loose stools.The secondary symptoms include depressive emotion or irritation, frequent sighs, excessive bowel sounds and gas, abdominal pain with urgency to run to the bathroom, and the pain reduces after defecation, a tongue with white or greasy coating, and thready or thin pulse beats. Three major symptoms (distending pain in the stomach or hypochondrium is necessary) or two major symptoms (still distending pain in the stomach or hypochondrium is necessary) together with two secondary symptoms can confirm the diagnosis.
1.2 Inclusion criteria
Conformed to the diagnostic criteria in Western medicine; in line with the TCM syndrome differentiation standard; aged 25-65 years old; voluntarily joined in the trial and signed the informed consent.
1.3 Exclusion criteria
Patients with circulatory, respiratory, or digestive disorders; those with contagious diseases or serious open wounds; those with malnutrition or severe mental disorders; pregnant women or those in the lactation period.
1.4 Suspension and dropout criteria
Suspension due to adverse reactions; received other pharmaceutical or non-pharmaceutical interventions for insomnia during the treatment; poor compliance;those lost during or after treatment.
1.5 Statistical methods
We used the SPSS version 18.0 software for statistical analysis. Pearson correlation analysis was used for linear correlation analysis. The measurement data satisfying normal distribution were expressed as mean ± standard deviation (±s) and compared using one-way analysis of variance (ANOVA) or ANOVA of factorial design. The comparison of data before and after treatment was performed by pairedt-test. Those not conforming to normal distribution were expressed as median (inter-quartile range) [M (IQR)] and compared using the rank-sum test. The enumeration data were expressed as rates and compared using the Chi-square test.P<0.05 indicated statistical significance.
1.6 General data
A total of 120 patients with insomnia due to liver-Qi stagnation and spleen deficiency were recruited from Shanghai Research Institute of Acupuncture and Meridian and Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine. They were randomized into a low-dosage group and a high-dosage group using the random numbers generated by the SPSS version 18.0 software in a stratified and stage-by-stage manner.Each group was further divided into a 7 d sub-group and a 14 d sub-group, with 30 cases in each group. That is to say, there were four groups: a high-dosage 7 d group, a high-dosage 14 d group, a low-dosage 7 d group, and a low-dosage 14 d group. In the end, 5 cases dropped out in the high-dosage 7 d group, 8 in the high-dosage 14 d group, 9 in the low-dosage 7 d group, and 2 in the low-dosage 14 d group. Hence, 96 cases completed the study. There were no significant differences in age,gender, or disease duration across the four groups(P>0.05), suggesting comparability (Table 1).
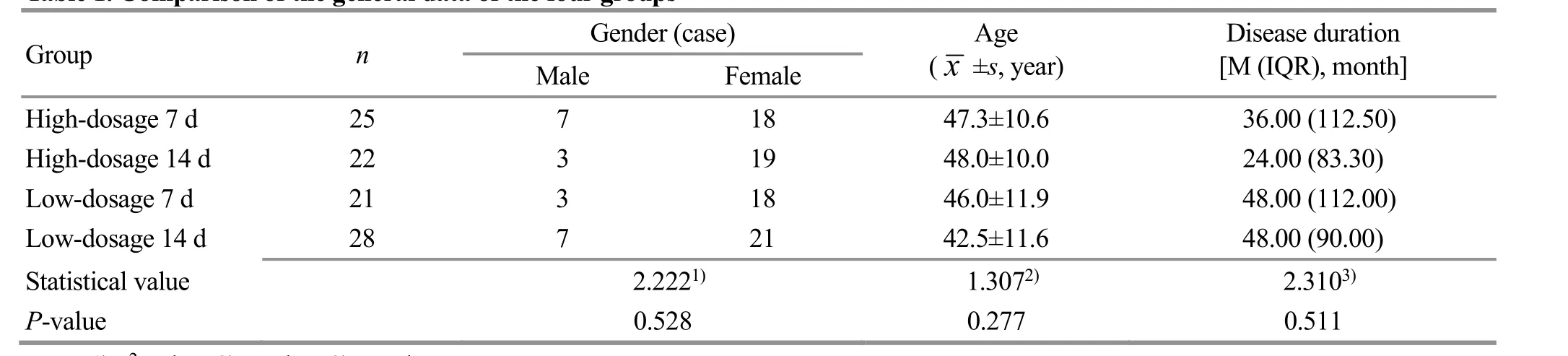
Table 1. Comparison of the general data of the four groups
2 Treatment Methods
2.1 Acupuncture treatment
Points: Baihui (GV20), Shenmen (HT7), Yintang(GV29), Shenting (GV24), Anmian (EX-HN22), Neiguan(PC6), Zusanli (ST36), and Sanyinjiao (SP6).
Method: After sterilization of the skin, acupuncture treatment was performed using needles of 0.22 mm in diameter and 40 mm in length. The needles were swiftly inserted, performed with lifting-thrusting and twirling manipulations, and then retained for 20 min when needling sensations were obtained (Deqi). The acupuncture treatment was performed once every other day for three sessions in total.
2.2 Acupoint sticking therapy
Points: Shenque (CV8) and Yongquan (KI1).
Medication and method:Wu Zhu Yu(Fructus Evodiae)powder was screened using a 100-mesh sieve, made into pastes, and then placed on empty adhesive plasters.The patients applied acupoint sticking on their own each night (half an hour before bedtime) with the bilateral Yongquan (KI1) used alternately.
2.2.1 High-dosage 7 d group
The acupoint sticking was offered at a dosage of 5 g herbal powder, 6-12 h each time, once a day for 7 d.
2.2.2 High-dosage 14 d group
The acupoint sticking was offered at the same dosage and frequency as in the high-dosage 7 d group but for 14 d in total.
2.2.3 Low-dosage 7 d group
The acupoint sticking was performed at a dosage of 3 g herbal powder, 6-12 h each time, once a day for 7 d.
2.2.4 Low-dosage 14 d group
The treatment was performed at the same dosage and frequency as in the low-dosage 7 d group but for 14 d in total.
3 Therapeutic Efficacy Observation
3.1 Observed indicators
3.1.1 Subjective indicators
The subjective indicators concluded Pittsburgh sleep quality index (PSQI) and TCM symptoms score.
The PSQI consists of seven domains and 18 self-rating items. Each domain is graded 0-3 and correspondingly scored 0-3 points, making a total score ranging from 0 to 21 points. A higher PSQI score means a worse sleep quality.
The TCM symptoms score divided the symptoms into major symptoms (depressive mood or irritation;distending pain in the stomach or hypochondrium;loose stools) and secondary symptoms (frequent sighs;excessive bowel sounds and gas; abdominal pain with urgency to run to the bathroom and the pain reduces after defecation), which were scored 0-3 points. The full score is 30 points. The higher the score, the more serious the symptoms.
3.1.2 Objective indicators
The actigraphic readings were taken as the objective indicators in this study, including the total time in bed,total sleep time, sleep efficiency (the total sleep time ÷the total time in bed × 100%), the number of wake bouts after asleep (the total number that the body moves after asleep until waking up), length of wakes(sum of the duration of wakes after falling asleep till waking up), and sleep latency (time from going to bed till falling asleep).
3.2 Results
3.2.1 Correlation analysis
The pre-treatment correlation analysis of the subjective and objective indicators of the 96 patients revealed that the PSQI score was positively related to the total time in bed and total sleep time. It means that the higher the PSQI score, the longer the total time in bed and total sleep time. Besides, the association between the TCM symptoms score and the actigraphic readings was insignificant (Table 2).
3.2.2 Comparison of the actigraphic readings
Intra-group comparisons: The total sleep time and sleep efficiency increased after treatment in the high-dosage 14 d group and low-dosage 14 d group(P<0.05), while the other two groups showed insignificant changes in the total sleep time and sleep efficiency after treatment (P>0.05). The sleep latency changed significantly after treatment in all four groups(P<0.05). Inter-group comparisons: After treatment, the total sleep time was longer in the high-dosage groups than in the low-dosage groups of the same treatment duration (P<0.05); given the same dosage, the 14 d groups showed a shorter length of wakes after asleep than the 7 d groups (P<0.05), (Table 3-Table 5).
3.2.3 Comparison of the PSQI score
There was no significant difference in the PSQI score among the four groups before treatment (P>0.05). The PSQI score changed significantly after treatment in all four groups (P<0.05), suggesting that acupuncture combined with acupoint sticking therapy can improve sleep quality in the patients. There were no significant differences in the PSQI score after treatment or the post-treatment change in the score between the groups of the same treatment duration but different dosagesP>0.05). However, there were significant differences in the PSQI score after treatment and the post-treatment change in the score between groups of the same dosage but different treatment durations (P<0.05). The correlation between the dosage and treatment duration was insignificant (P>0.05), indicating that 14 d treatments can notably improve the PSQI score,insomnia symptoms, and quality of life in the patients(Table 6).
3.2.4 Comparison of the TCM symptoms score
There was no significant difference in the TCM symptoms score among the four groups before treatment (P>0.05). The TCM symptoms scores changed significantly after treatment in all four groups (P<0.05),suggesting that acupuncture combined with acupoint sticking therapy can improve the TCM symptoms in the patients. There were no significant differences in the TCM symptoms score after treatment or the post-treatment change in the score between the groups of the same treatment duration but different dosages(P>0.05). However, there were significant differences in the TCM symptoms score after treatment and the post-treatment change in the score between groups of the same dosage but different treatment durations(P<0.05). The correlation between the dosage and treatment duration was insignificant (P>0.05), indicating that 14 d treatments can notably improve the TCM symptoms score in the patients (Table 7).

Table 2. Correlation between the subjective and objective indicators
Table 3. Comparison of the total time in bed, total sleep time, and sleep efficiency in the four groups ( ±s)

Table 3. Comparison of the total time in bed, total sleep time, and sleep efficiency in the four groups ( ±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the high-dosage 7 d group after treatment, 2) P<0.05;compared with the high-dosage 14 d group after treatment, 3) P<0.05
Total sleep time (minute) Sleep efficiency (%)388.67±70.56 81.30±7.85 399.76±73.13 83.19±6.87 359.91±61.56 78.13±8.00 400.41±64.511) 84.42±6.241)354.24±63.62 76.98±5.09 361.62±61.722) 80.93±4.891)361.12±69.72 79.02±10.69 375.32±50.791)3) 83.56±7.941)
Table 4. Comparison of the number of wake bouts and length of wakes after asleep in the four groups ( ±s)

Table 4. Comparison of the number of wake bouts and length of wakes after asleep in the four groups ( ±s)
Note: Compared with the high-dosage 7 d group after treatment, 1) P<0.05; compared with the low-dosage 7 d group after treatment, 2)P<0.05
Group n Time Number of wake bouts (number) Length of wakes after asleep (minute)High-dosage 7 d 25 Before treatment 39.08±13.98 64.25±30.89 After treatment 37.12±12.23 69.52±25.42 High-dosage 14 d 22 Before treatment 40.36±12.59 72.47±30.46 After treatment 38.91±15.87 59.59±32.151)Low-dosage 7 d 21 Before treatment 32.14±9.03 83.42±21.81 After treatment 32.85±6.37 84.14±19.77 Low-dosage 14 d 28 Before treatment 35.53±10.72 72.53±37.17 After treatment 34.54±11.01 62.85±31.422)

Table 5. Comparison of the sleep latency in the four groups [M (IQR), minute]
Table 6. Comparison of the PSQI score before and after treatment ( ±s point)

Table 6. Comparison of the PSQI score before and after treatment ( ±s point)
Note: PSQI=Pittsburgh sleep quality index; compared with the same group before treatment, 1) P<0.05; compared with the high-dosage 7 d group after treatment, 2) P<0.05; compared with the low-dosage 7 d group after treatment, 3) P<0.05
Group n Before treatment After treatment Difference between before and after treatment High-dosage 7 d 25 14.16±3.00 11.20±4.231) 2.96±3.16 High-dosage 14 d 22 13.27±3.74 8.68±3.801)2) 4.59±3.712)Low-dosage 7 d 21 13.19±3.06 10.10±2.881) 3.10±2.96 Low-dosage 14 d 28 12.50±2.87 8.18±3.201)3) 4.32±3.083)
Table 7. Comparison of the TCM symptoms score before and after treatment ( ±s point)

Table 7. Comparison of the TCM symptoms score before and after treatment ( ±s point)
Note: TCM=Traditional Chinese medicine; compared with the same group before treatment, 1) P<0.05; compared with the high-dosage 7 d group after treatment, 2) P<0.05; compared with the low-dosage 7 d group after treatment, 3) P<0.05
Group n Before treatment After treatment Difference between before and after treatment High-dosage 7 d 25 14.04±4.08 11.24±4.231) 2.80±3.88 High-dosage 14 d 22 15.91±5.34 8.77±3.641)2) 7.14±5.272)Low-dosage 7 d 21 14.29±5.32 11.62±3.811) 2.67±4.75 Low-dosage 14 d 28 13.43±5.65 7.79±4.361)3) 5.64±4.513)
4 Discussion
Insomnia, also known as “sleeplessness” or literally“being unable to lie down”, mainly manifests as difficulty falling asleep, waking up easily during sleep,trouble falling asleep again after waking, or even staying sleepless the whole night. According to TCM, this problem originates from Yin deficiency and Yang hyperactivity and disharmony between the two aspects.In the view of modern medicine, the pathogenesis of insomnia should be hyperarousal, which means that excitation gives rise to insomnia. We can find some similarities between the two medical systems in the understanding of insomnia’s pathogenesis.
Stress is a significant factor in the development of insomnia, and a stress state itself refers to an emotional state caused by unexpected changes. The liver is a viscera in charge of dredging and dispersing. It regulates the flow of Qi and blood via modulating Qi activities to balance the mood. When the liver behaves poorly or excessively, the flow of Qi and blood will lose control and subsequently lead to insomnia, which breeds the idea of treating insomnia by targeting the liver. The TCM emotion theory and the stress theory of modern medicine share something in common; emotion management can help with intervening in the stress state. Thus, considering the significance of emotion and its relationship with the liver, we chose patients with insomnia due to liver-Qi stagnation and spleen deficiency as the subjects.
Acupoint sticking therapy is effective for insomnia[13-15], which has been backed up by systemic review[16]. However, the existing evidence has been weakened by the variety in the medication, a lack of evaluation measures that combine subjective and objective perspectives, unequal treatment duration,indefinite medication dosage, etc. Through analysis of the literature studying the treatment of insomnia with acupoint sticking therapy, we have found thatWu Zhu Yuis the most commonly used medication, and Yongquan (KI1) and Shenque (CV8) are the most commonly used points[17-18].Wu Zhu Yuenters the Liver Meridian and works to soothe the liver to relieve depression. As the Jing-Well point of the Kidney Meridian, Yongquan (KI1) belongs to the element of wood and can guide fire to its origin to treat insomnia.Shenque (CV8) is an essential point of the Conception Vessel, connecting various vessels, and is the root of the Zang-Fu organs. It bears the function of calming the mind. Hence, this study adopted the medication and points mentioned above for acupoint sticking therapy.
Different acupuncture protocols perform differently in treating insomnia[19-20]. Baihui (GV20), Shenmen(HT7), Yintang (GV29), Shenting (GV24), Anmian(EX-HN22), Neiguan (PC6), Zusanli (ST36), and Sanyinjiao (SP6) are often selected to treat insomnia as these points can calm the mind to help with sleep[21].Therefore, the insomnia patients recruited in this trial all received the acupuncture treatment by selecting these points while receiving the observation of the effects of acupoint sticking therapy with different medication dosages and treatment durations on the subjective and objective indicators.
PSQI is a scale for evaluating sleep quality[22-23]. In this study, the PSQI score was improved after treatment in all four groups. Further, different dosages did not significantly affect the score (P>0.05), but different treatment durations did (P<0.05). We can conclude that 14 d acupoint sticking therapy can notably improve the PSQI score and the symptoms in treating insomnia based on acupuncture treatment.
The syndrome of liver-Qi stagnation and sleep deficiency is quite common in insomnia patients[24-26]. In this study, the four groups all gained marked improvements in the TCM symptoms score. Different medication dosages did not significantly affect the score(P>0.05), but different treatment durations did (P<0.05).We can conclude that based on acupuncture treatment,14 d acupoint sticking therapy can significantly improve the TCM symptoms in insomnia patients, which is consistent with the conclusion regarding the PSQI score.
Actigraphy and polysomnography are two objective measures often used to observe the sleep state[27-28].Actigraphy is an effective way to assess the total sleep time and how awake the person is when sleep starts. It is easy to operate and portable and thus has been popular in observing sleep-wake activities.
We observed the patients’ sleep state using actigraphy and polysomnography and found that based on acupuncture treatment, acupoint sticking therapy can markedly improve sleep latency; the high- dosage and low-dosage 14 d groups showed improvements in the total sleep time and sleep efficiency; regarding the length of wakes after asleep, the 14 d groups were better than the 7 d groups; the high-dosage groups worked better than the low-dosage groups in comparing the total sleep time. Thus, we can say that 14 d acupoint sticking therapy can significantly shorten the length of wakes after asleep, and the high-dosage acupoint sticking treatment can extend the total sleep time in insomnia patients based on acupuncture treatment.
The correlation analysis of the subjective and objective indicators in the 96 insomniac subjects before the study revealed that the PSQI score was positively correlated with the total time in bed and total sleep time, while there was no significant correlation between the TCM symptoms score and actigraphic readings. According to the study results, based on acupuncture treatment, acupoint sticking therapy works differently on the total sleep time when the medication dosage is different and works differently on the PSQI score and the length of wakes after asleep when the treatment duration is different. We can further draw a conclusion that based on acupuncture treatment, different treatment durations of acupoint sticking therapy have a consistent effect on the subjective and objective indicators.
In a word, based on the same acupuncture treatment,acupoint sticking therapy produces different effects on the subjective and objective indicators in insomnia patients when the treatment duration differs; 14 d is superior to 7 d. We are planning to extend the treatment duration and design follow-up studies in the future to find the optimal treatment length for acupoint sticking treatment of insomnia.
Conflict of Interest
There is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Topics of Shanghai Municipal Commission of Health and Family Planning (上海市卫生和计划生育委员会科研课题, No.20174Y0063); Youth Project of National Natural Science Foundation of China (国家自然基金青年项目, No.81804200).
Statement of Informed Consent
Informed consent was obtained from all individual participants.Received: 10 November 2020/Accepted: 29 June 2021
 Journal of Acupuncture and Tuina Science2022年4期
Journal of Acupuncture and Tuina Science2022年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Research on clinical application of manual therapy to tumor-related adverse reactions
- Observation on efficacy of thumbtack needle combined with pediatric Tuina for constipation in children caused by liver depression and Qi stagnation
- Clinical study on Tuina plus physical agents for lateral collateral ligament injury of ankle in gymnasts
- Efficacy of knee-balancing manipulation plus heat-sensitive moxibustion for knee osteoarthritis and its influence on CTX-Ⅰ, TRACP-5b,ADAMTS-4, and MMP-3
- Clinical observation of warm needling moxibustion plus lumbar traction for lumbar disc herniation
- Effects of acupuncture on nutritional status in patients in a persistent vegetative state:a prospective randomized controlled study
