A systematic Review of the Safety and Effectiveness of Epidural Analgesia for Labor Analgesia
Wang Dan ,Liu Chunping ,Zhang Fang* ,Gao jinglei
(1.School of Business Administration,Shenyang Pharmaceutical University,Shenyang 110016,China;2.China National Health Development Research Center,Beijing 100000,China)
Abstract Objective To re-evaluate the systematic review of the safety and effectiveness of epidural analgesia (EA) for labor analgesia.Methods The Cochrane database,PubMed,EMBASE,EBSCO,Web of Science,Science Direct,China Biomedical Literature database,CNKI,Wanfang and VIP databases were searched,and the search time was limited to August 2020.Two researchers screened the literature and extracted data according to the inclusion criteria.AMSTAR was used to evaluate the methodological quality of the included studies.Pain intensity and pain relief satisfaction were used as the main indicators for re-evaluation of the effectiveness.Midwifery rate,cesarean section rate,back pain,fever,nausea and vomiting,umbilical artery pH value,and newborn Apgar score were used as the main indicators to re-evaluate the safety.Results and Conclusion A total of 9 meta-analyses were included.The safety and effectiveness of EA and opioid intravenous analgesia,acupuncture stimulation,inhalation analgesia,no analgesia,and continuous delivery were evaluated separately.The included systematic reviews showed that EA could increase the rate of device-assisted delivery,causing maternal fever,and prolonging the first and second stages of labor.But the incidence of back pain,nausea,and vomiting was lower.Therefore,analgesia had a good effect with better satisfactory degree.Current evidence shows that EA is safe and effective for labor analgesia,but the quality of the reports of current studies is not high.
Keywords:epidural analgesia;opioid intravenous analgesia;non-epidural analgesia;acupuncture stimulation;inhalation analgesia;continuous care;labor analgesia;systematic review re-evaluation
Severe pain during childbirth will make the mother feel stressed,afraid,and anxious,causing a series of reactions such as increased blood pressure,more myocardial oxygen consumption,irregular contractions,and decreased placental blood flow.This can affect the delivery process and increase the risk of complications for newborns such as intrauterine distress and postpartum hemorrhage[1,2].In order to avoid the labor pain,most pregnant women choose cesarean section to terminate their pregnancy,resulting in the high rate of cesarean section in China.In this context,choosing safe and effective labor analgesia is crucial for both the mother and the baby.To implement the“Notice on Issuing Opinions on Strengthening and Improving Anesthesia Medical Services” and the “Notice on Launching Pilot Labor Analgesia Work”,the National Health Commission’s Medical Administration and Hospital Administration commissioned the National Health Commission’s Health Development Center to carry out a third-party evaluation project for labor analgesia pilot work.It would strengthen the evaluation and policy guidance of pilot work for labor analgesia so as to timely summarize and promote the beneficial experience.Under this project,the safety and effectiveness of the epidural analgesia (EA) used in pilot hospitals were analyzed,and a large number of systematic reviews were conducted to study the EA for labor analgesia.At present,there is still no relevant research to summarize these systematic reviews.This study used the method of systematic review and re-evaluation to analyze the safety and effectiveness of epidural labor analgesia,thus providing evidence for the next national promotion of clinical labor analgesia.
1 Methods
1.1 Inclusion and exclusion criteria
Research type:Systematic reviews on the safety and effectiveness of EA for labor analgesia published at home and abroad.
Research objects:Women giving birth vaginally or giving birth with analgesia trial.
Intervention measures:The study group used EA technique,and the control group used non-EA technique.
Outcome indicators:Safety indicators include midwifery rate,cesarean section rate,back pain,fever,nausea and vomiting,umbilical artery pH value,neonatal Apgar score,and labor process.Efficacy indicators include pain score and pain relief satisfaction.
Exclusion criteria:(1) Systematic reviews for repeated publications;(2) Systematic reviews which can obtain the full text to extract data;(3) Non-SCI journals and domestic core journals.
1.2 Search methods
Eligible trials were retrieved by searching databased references of related reviews or meta-analysis.Database of biomedical literature from China and abroad such as CNKI,Wanfang,VIP,the Cochrane library,PubMed,EMBASE,Web of Science,and ScienceDirect were searched.The search time was limited to August 2020.The following keywords such as epidural analgesia,analgesia,epidural space,labor pain,labor obstetric,systematic review,system overview,meta,meta-analysis and meta analyses were used.Taking PubMed as an example,the specific search method is shown in Table 1.
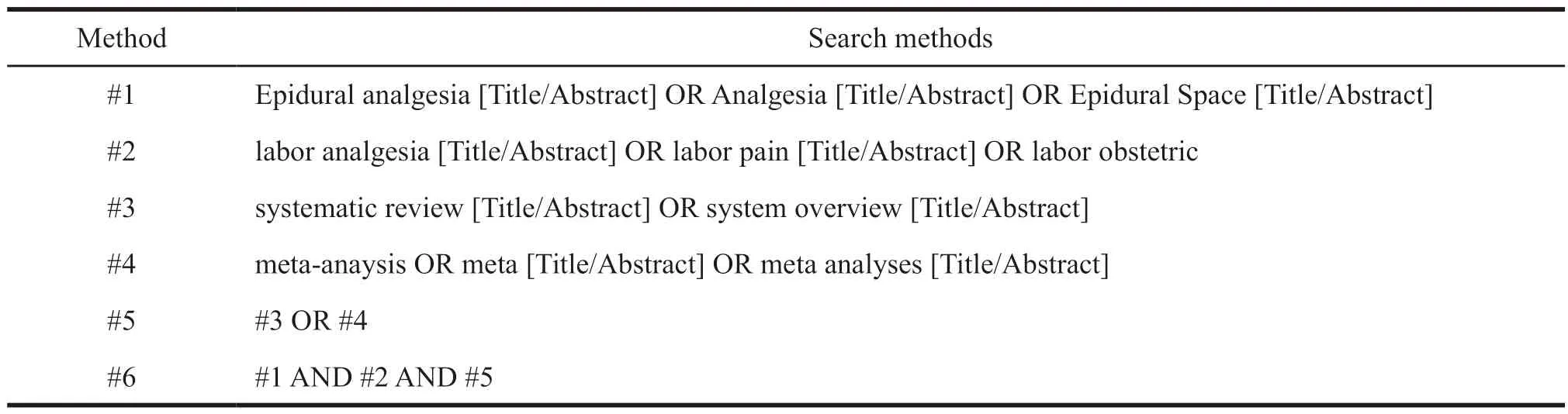
Table 1 PubMed search method
1.3 Data collection
Two reviewers independently assessed the literature based on the inclusion and exclusion criteria,extracted data,and cross-checked them.In case of disagreement,a third researcher was consulted to make the decision.First,the literature management software Endnote was used to screen the title and abstract.Then,the full text was taken out to analyze potential related research.The original author would be contacted to supplement the relevant information for the incomplete information report.Finally,the data for the determined research were extracted.The extracted data included the basic information of the literature,intervention measures,outcome indicators and methodological quality indicators in the systematic reviews.
1.4 Validity assessment
The AMSTAR evaluation checklist[3,4]was used to evaluate the quality of the included systematic reviews.
2 Results
2.1 Flowchart
A total of 82 relevant articles were detected in the initial screening,and after gradual deletion,9 meta-analysis were finally included.One of them was a systematic review from the Cochrane library database that combined the meta-analysis of epidural labor analgesia with 5 other measures.So,it was split into 5 articles (Fig.1).
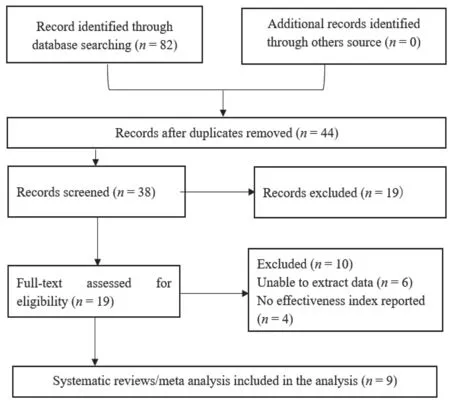
Fig.1 Document retrieval flowchart
2.2 Characteristics of systematic reviews
Table 2 shows detailed characteristics of systematic reviews.
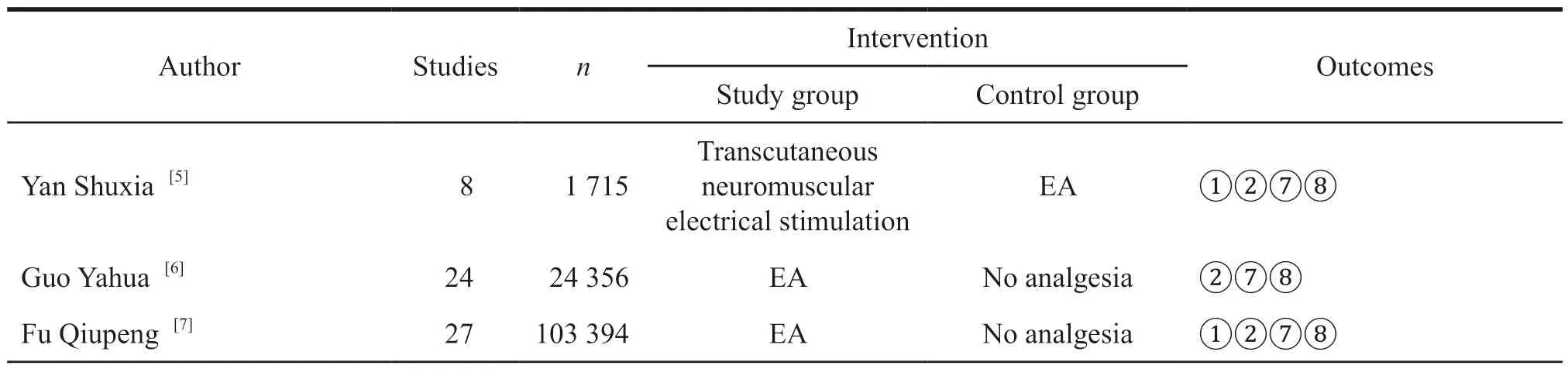
Table 2 Characteristics of systematic reviews
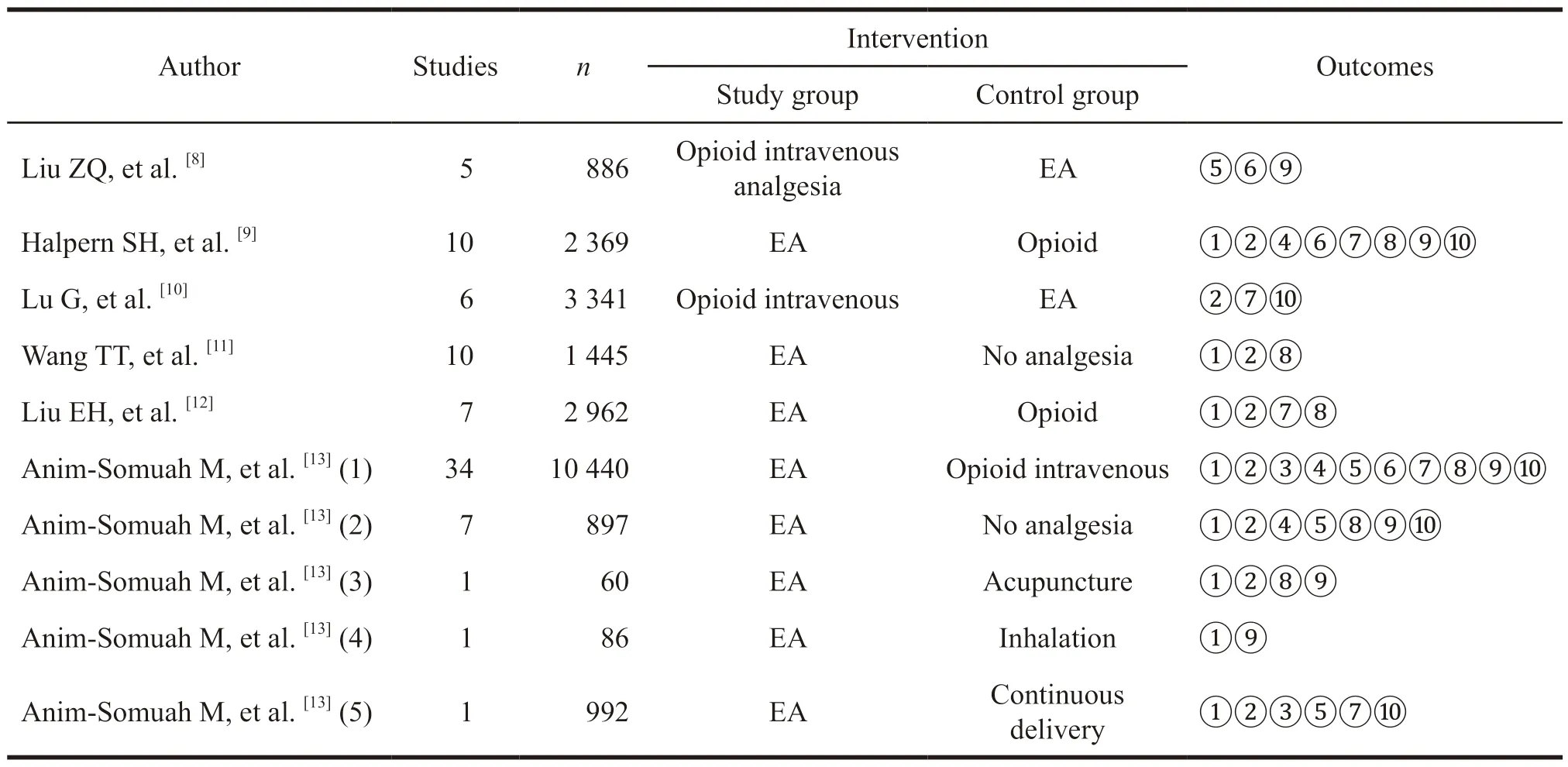
Continued Table 2
2.3 Quality of evidence
The methodological quality evaluation results included in the meta-analysis are shown in Table 3.The items with poor quality evaluation include:Item 11,describing relevant conflicts of interest.Item 10,assessing publication bias.Item 4,considering publication in the inclusion criteria.Item 5,providing a list of included and excluded research literature.Items with good quality evaluation include:Item 1,providing preliminary design plan and item 2,reproducibility of included research selection and data extraction.
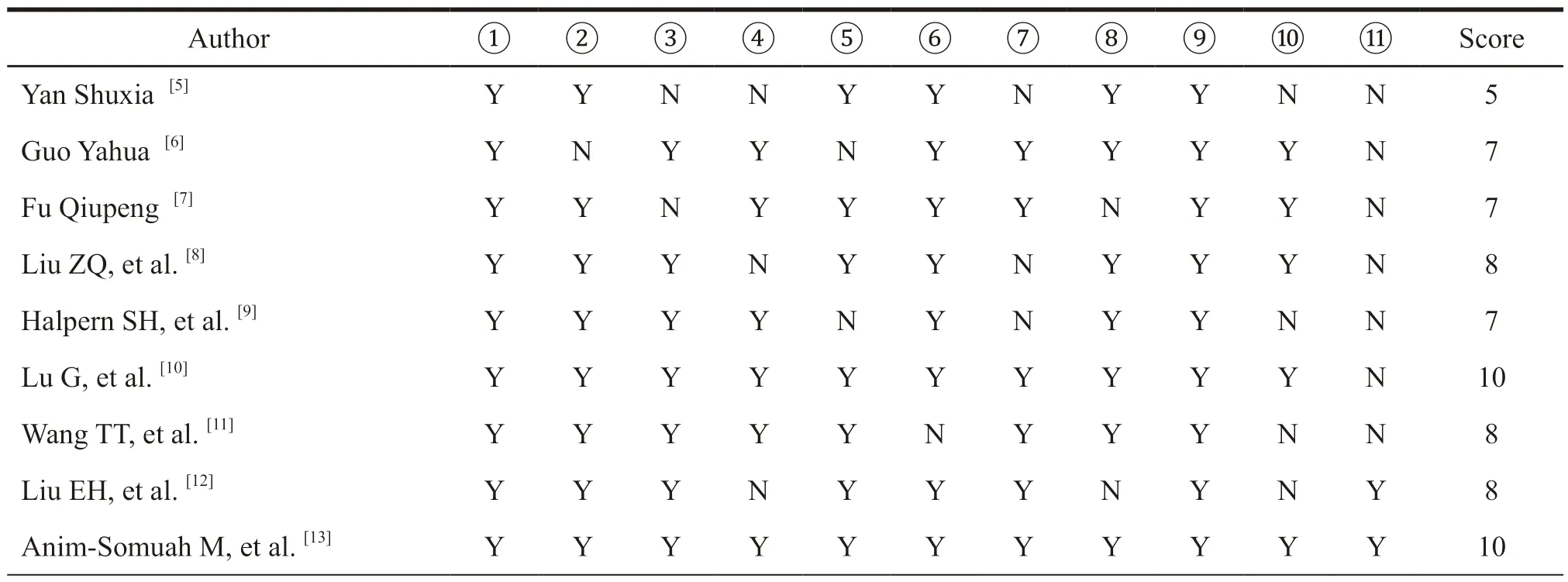
Table 3 Methodological quality evaluation results included in meta-analysis
2.4 Safety re-evaluation results
2.4.1 Incidence of midwifery
A total of 9 meta-analyses were included to compare the incidence of EA and assisted delivery.The summary results are shown in Table 4.Among them,5 meta-analysis[7,11,13]showed that EA did not increase the incidence of midwifery compared with the control group.There was no statistically significant difference.Yan Shuxia[5]compared EA with transcutaneous neuromuscular electrical stimulation,and the results showed that EA would increase the incidence of midwifery with statistical significance.Comparisons of 3 meta-analysis[9,12,13]of EA and opioid all show that EA can increase the incidence of maternal midwifery.
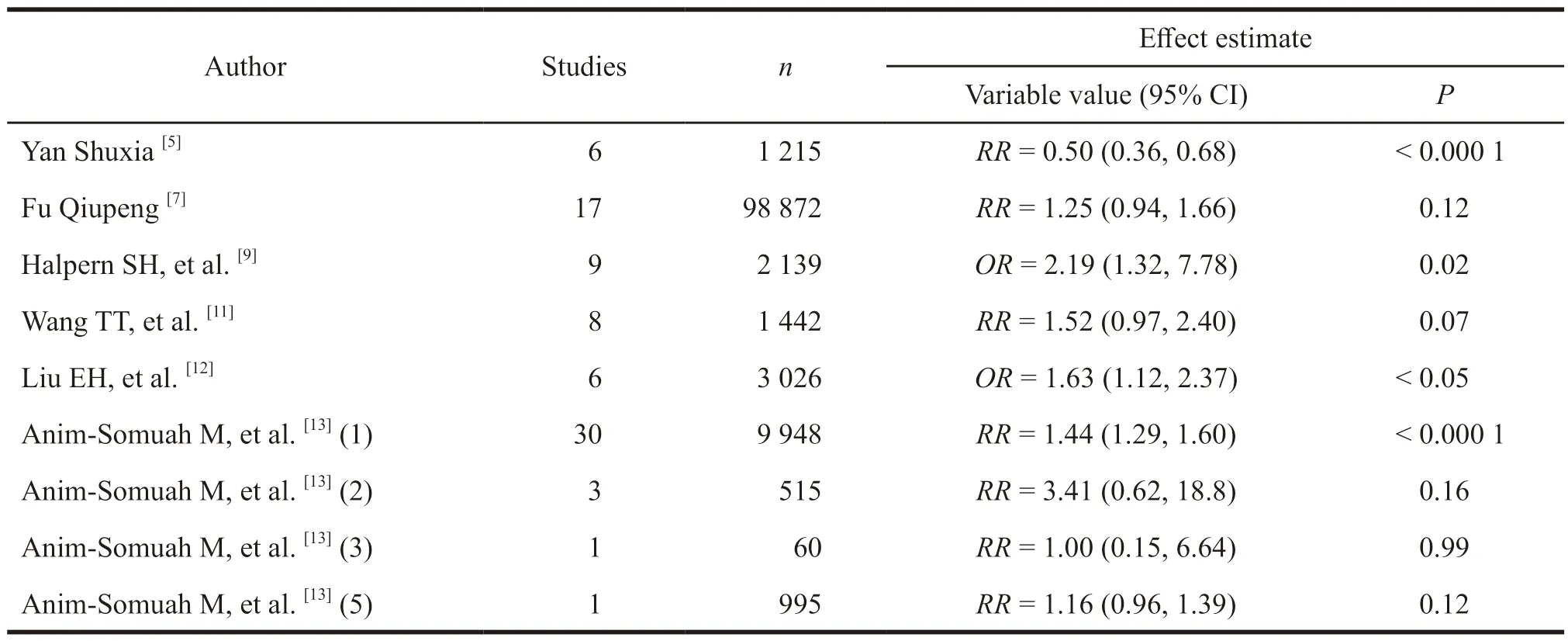
Table 4 Summary of the incidence of midwifery included in the meta-analysis
2.4.2 Cesarean section rate
A total of 11 meta-analyses were included to compare the incidence of cesarean section with EA.The summary results are shown in Table 5.Seven of the meta-analysis results showed that EA did not increase the incidence of cesarean section.Yan Shuxia[5]found that EA could increase the incidence of cesarean section compared with percutaneous neuromuscular electrical stimulation through a metaanalysis.Other 3 articles[6,7,13]showed that the EA group could reduce the incidence of cesarean section compared with the no analgesia group.
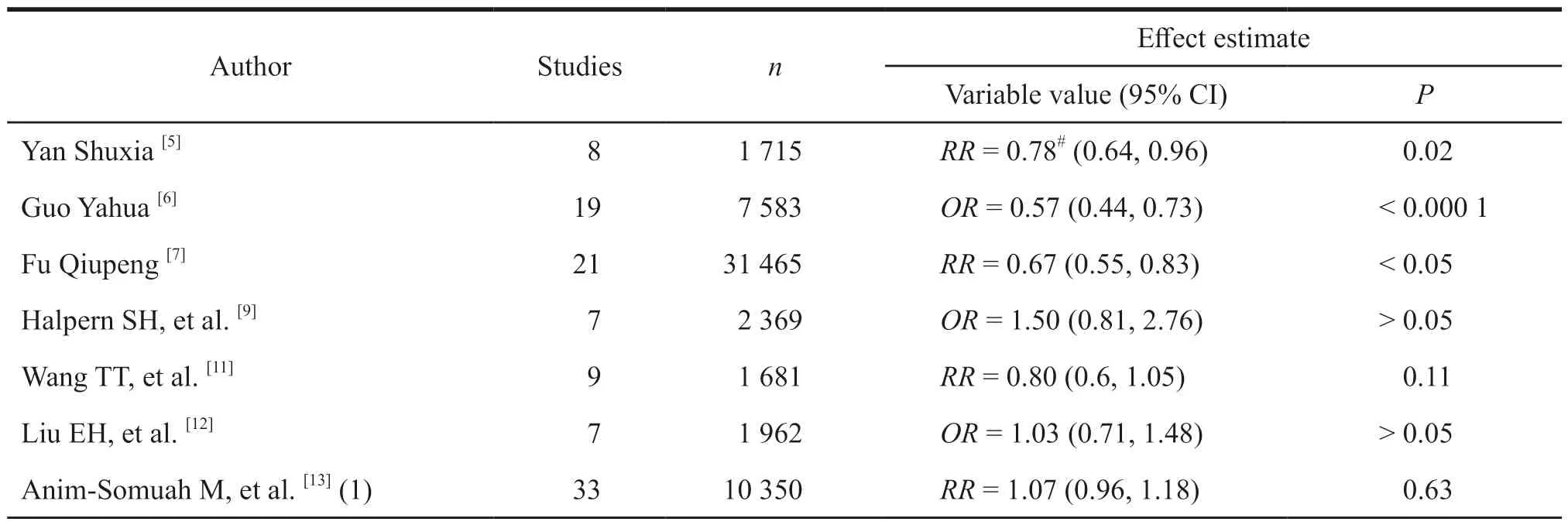
Table 5 Meta-analysis summary of the incidence of cesarean section
Continued Table 5
2.4.3 Back pain
A total of 2 meta-analyses were included to compare the occurrence of back pain in women with EA.The summary results are shown in Table 6.The meta-analysis of Anim-Somuah M,et al.[13](1)compared EA with opioid intravenous analgesia.The results showed that there was no statistical difference between EA and opioid intravenous analgesia in the incidence of maternal back pain.The meta-analysis of Anim-Somuah M,et al.[13](5) compared EA with continuous delivery,and the results showed that there was no statistical difference in the incidence of back pain between the two groups.
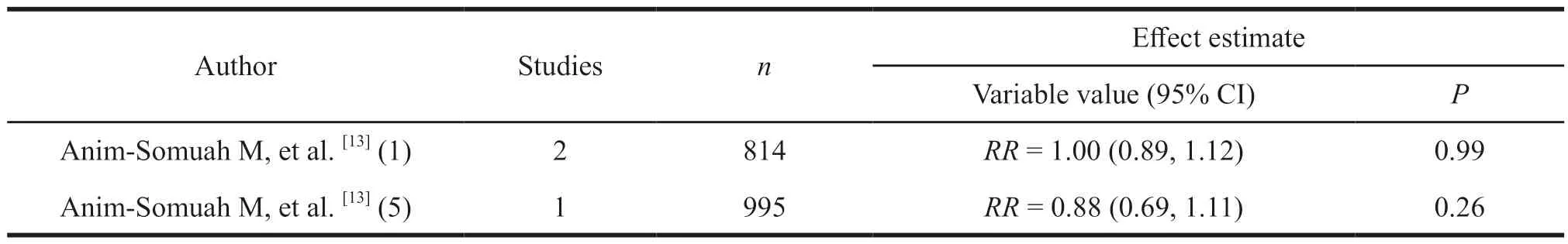
Table 6 Meta-analysis summary of back pain
2.4.4 Fever
A total of 4 meta-analyses were included to compare the occurrence of EA and fever.The summary results are shown in Table 7.Two of the metaanalysis[9,13]compared EA with opioid intravenous analgesia,and the results showed that EA had a higher fever rate than opioid intravenous analgesia.The meta-analysis research group of Lu G,et al.[10]studied intravenous opioid analgesia,and the results showed that EA could increase the incidence of maternal fever.A systematic review of Anim-Somuah M,et al.[13](2) compared EA with no analgesia,and the results showed that the difference in fever rate between the EA group and the no analgesia group was not statistically significant.
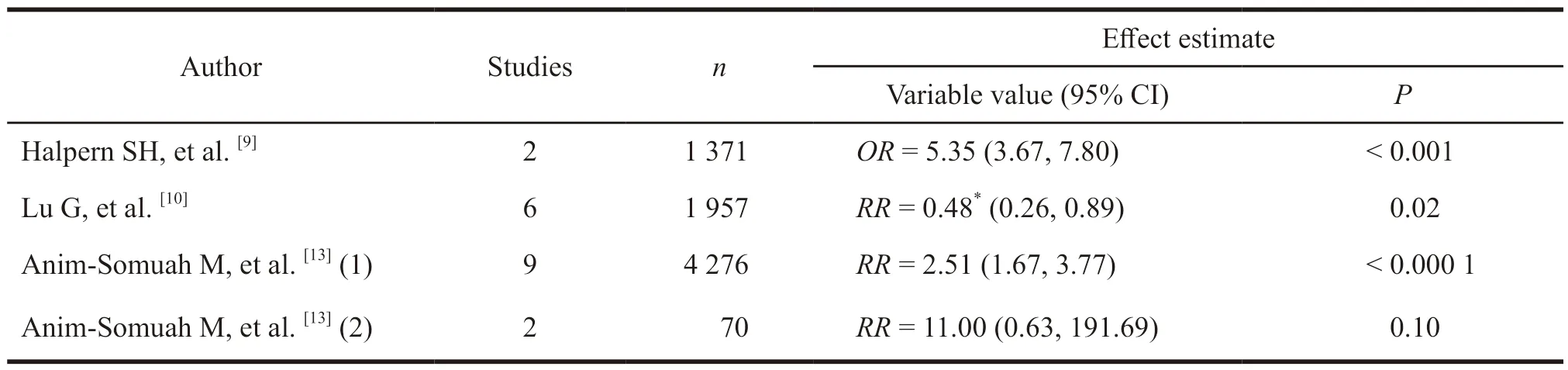
Table 7 Meta-analysis summary of fever occurrence
2.4.5 Nausea and vomiting
A total of 4 meta-analyses were included to compare the occurrence of EA,nausea and vomiting.The summary results are shown in Table 8.The metaanalysis of Anim-Somuah M (1)[13]compared EA with opioid intravenous analgesia,and the results showed that EA had a lower incidence of nausea and vomiting than opioid intravenous analgesia.The other three meta-analyses[8,13]results comparing non-anaesthetic analgesia with other analgesia showed that EA did not increase the incidence of nausea and vomiting.
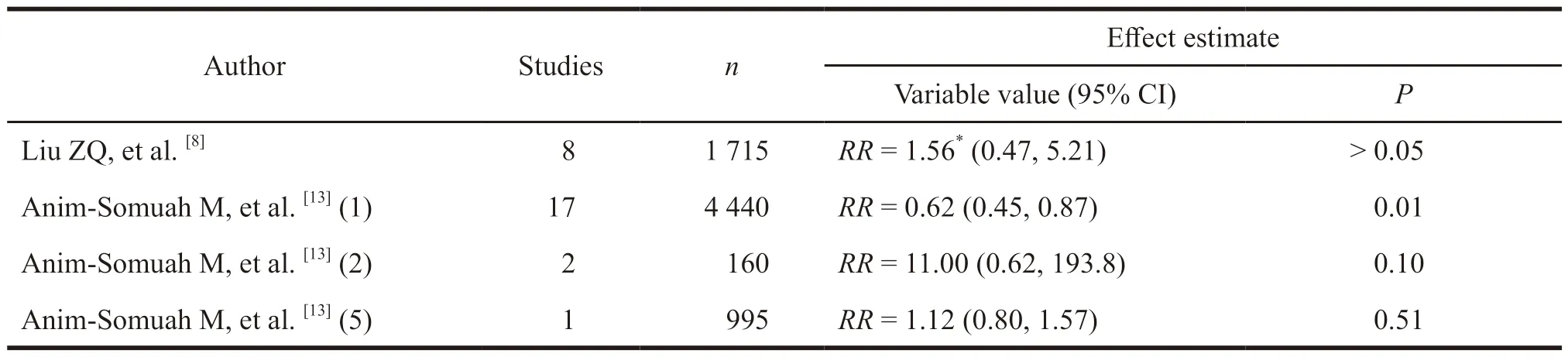
Table 8 Meta-analysis summary of the occurrence of nausea and vomiting
2.4.6 Umbilical artery pH value
A total of 3 meta-analyses were included to compare the pH value of the umbilical artery in neonates with EA.The results are shown in Table 9.Liu ZQ,et al.[8]compared patients’ intravenous self-control and EA,and the results showed that EA did not affect the pH of the neonatal umbilical artery.The other two meta-analyses[9,13]compared EA with opioid intravenous analgesia.The analysis index used the incidence of neonatal umbilical artery pH <7.2,and concluded that EA had a lower incidence of umbilical artery than opioid.
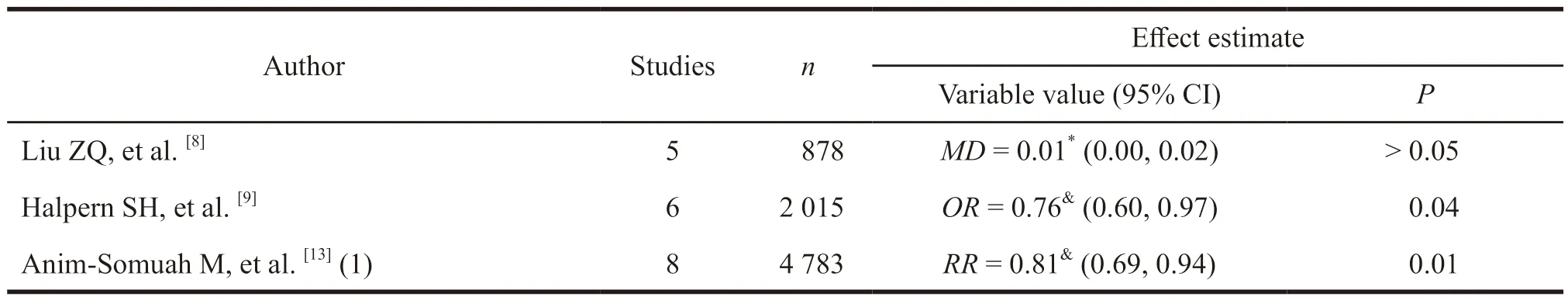
Table 9 Summary table of pH value of umbilical artery included in meta-analysis
2.4.7 Apgar score
A total of 8 meta-analyses were included to compare the Apgar scores of neonates with EA.The summary results are shown in Table 10.Among them,6 meta-analysis results[5,7,10,12,13]showed that EA and other labor analgesia had no significant difference in the Apgar score of newborns.Guo Yahua[6]compared the 1-minute Apgar scores of neonates in the EA group and the no analgesia group,and the results showed that epidural analgesia could reduce the incidence of neonatal asphyxia.Fu Qiupeng[7]compared the difference in the standardized mean of the Apgar scores of 1 minute neonates in the EA and non-analgesic groups,and the results showed that the labor analgesia group scores were lower than the control group.The meta-analysis results of Halpern SH,et al.[9]showed that the incidence of neonatal Apgar scores less than 7 at 1 minute and 5 minutes in the EA group was lower.
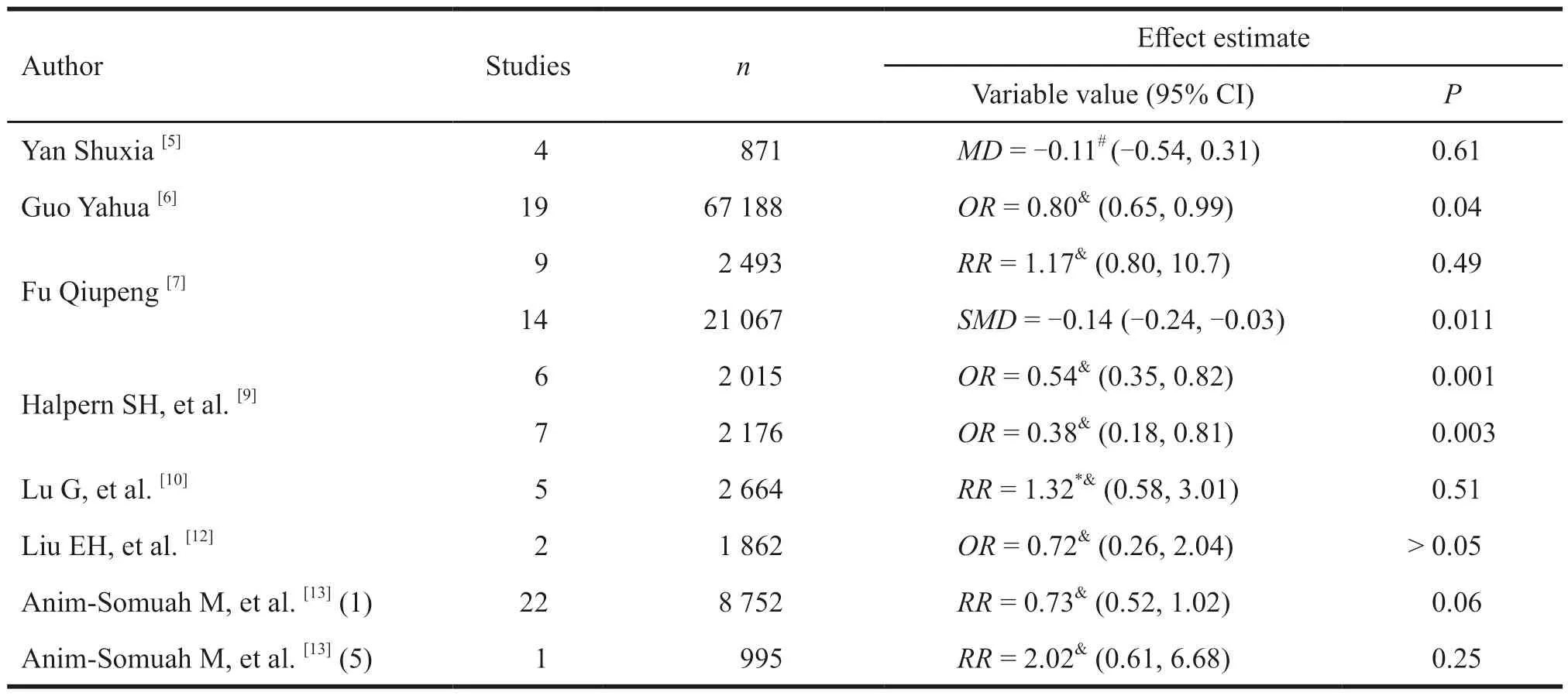
Table 10 Summary of Apgar scores of newborns included in the meta-analysis
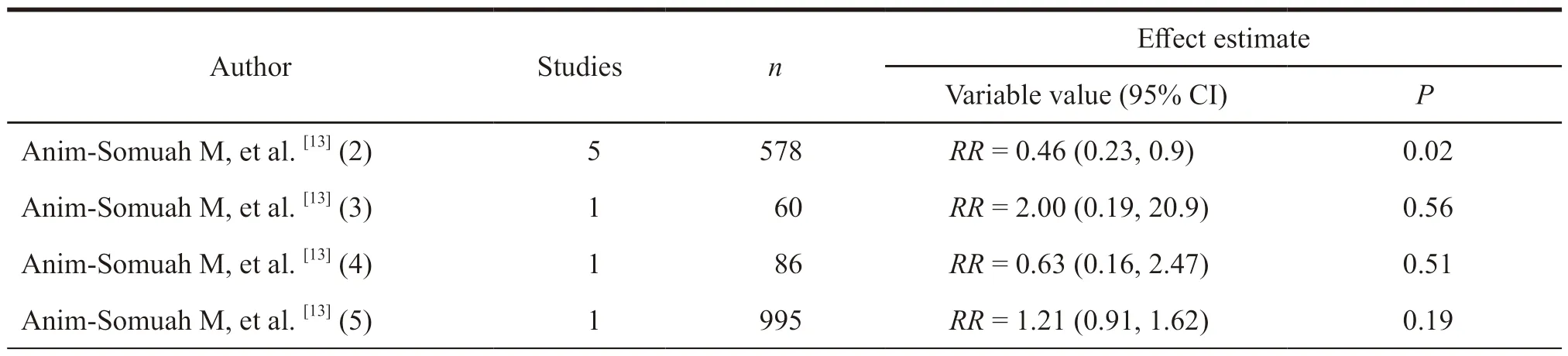
2.4.8 Labor
A total of 5 meta-analyses were included to compare the duration of EA in the first stage.The results are displayed in Table 11.Two of the metaanalysis compared EA with opioid intravenous analgesia.Halpern SH[9]and Anim-Somuah M (1)[13]all showed that EA could prolong the first stage of labor.The other three meta-analysis[7,11,13]compared EA with no analgesia or non-EA,and the results showed that there was no statistical difference in the first stage of labor.
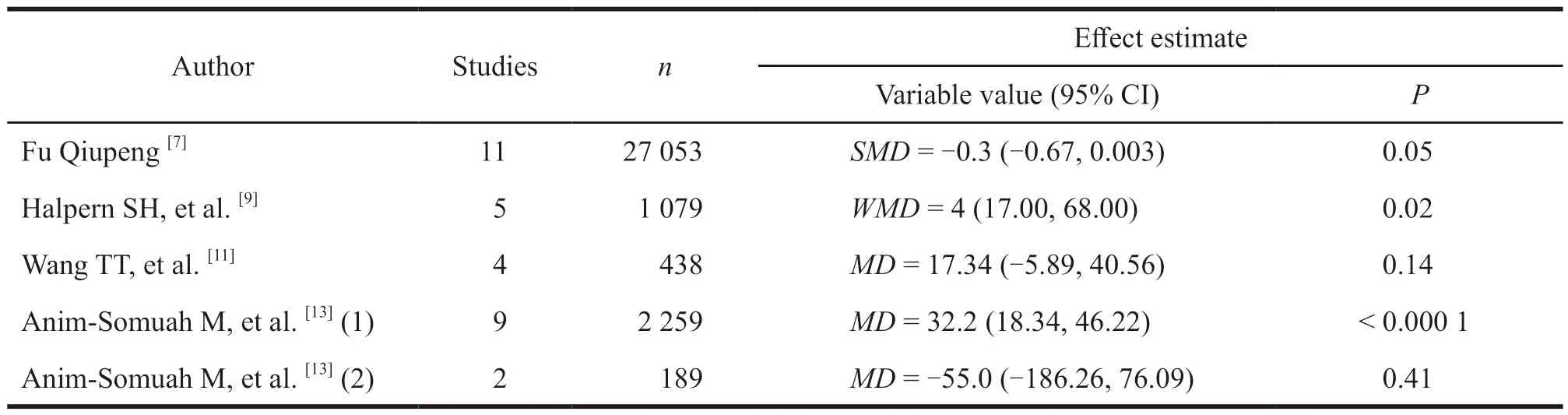
Table 11 Meta-analysis summary of the first stage of labor time
A total of 9 meta-analyses were included to compare the duration of EA in the second stage.The results are summarized in Table 12.Among them,4 meta-analysis results[6,7,11,13]showed that EA did not prolong the time of the second stage of labor.Yan Shuxia’s[5]meta-analysis results showed that EA could prolong the second stage of labor compared with transcutaneous neuromuscular electrical stimulation.Three of the meta-analysis[9,12,13]compared EA with opioid intravenous analgesia,and all the results showed that EA prolonged the second stage of labor.A systematic review of Anim-Somuah M,et al.[13](3)compared EA with acupuncture stimulation,and the results showed that EA prolonged the second stage of labor compared with acupuncture stimulation.
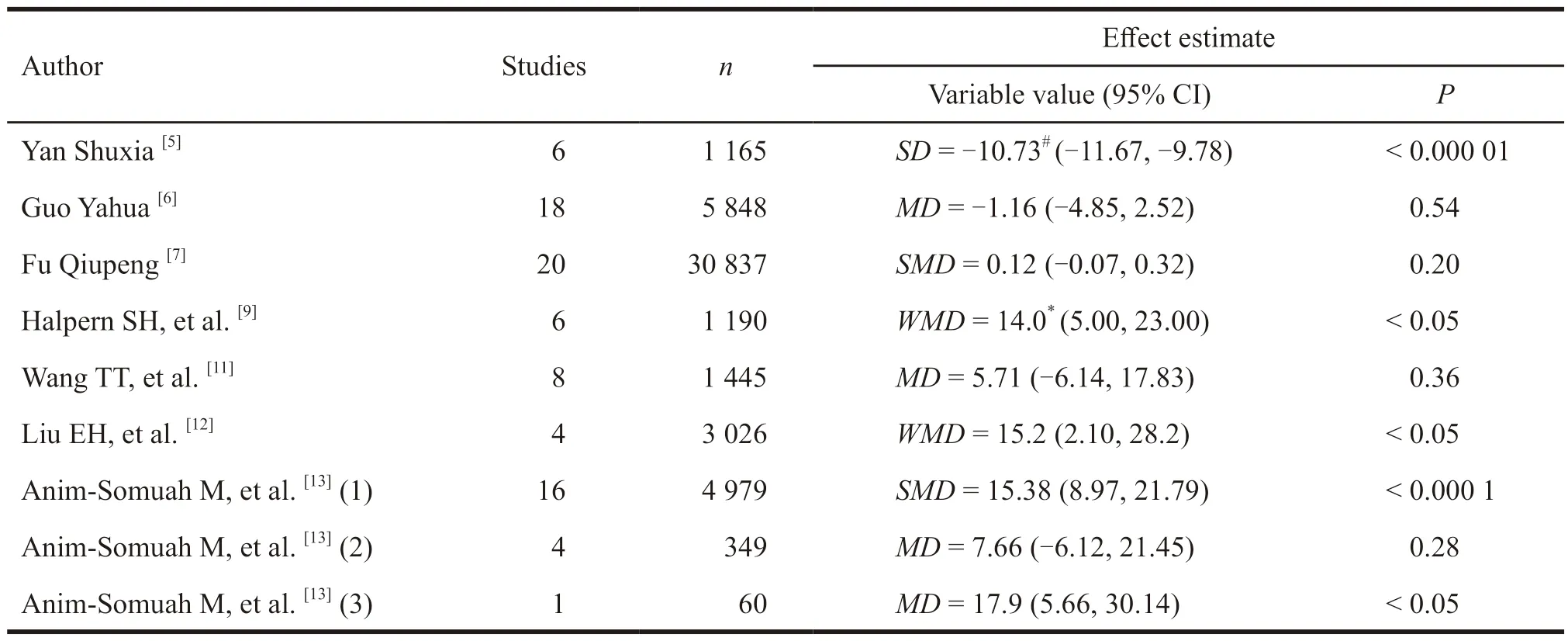
Table 12 Meta-analysis of the second stage of labor time
2.5 Effectiveness of re-evaluation results
2.5.1 VAS
A total of 4 meta-analyses were included to compare the pain scores after EA.The results are summarized in Table 13.Two meta-analysis[8,13]compared EA with opioid intravenous analgesia,and the results showed that the pain scores of EA were lower than that of opioids,and the analgesic effect was better.The meta-analysis of Anim-Somuah M,et al.[13](2) compared EA with no analgesia,and the results showed that the effect of EA was better than that of the no analgesia group,and the difference was statistically significant.The meta-analysis results of Anim-Somuah M,et al.[13](3) showed that the effect of EA was better than acupuncture stimulation.
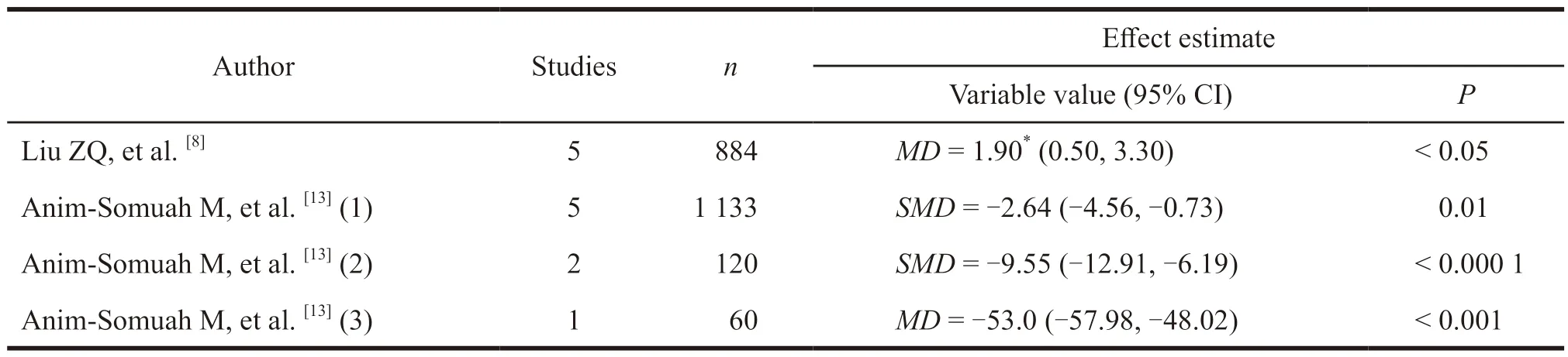
Table 13 Summary of meta-analysis pain scores
2.5.2 Pain relief satisfaction
A total of 5 meta-analyses were included to compare the satisfaction of epidural labor analgesia and pain relief.The results are summarized in Table 14.Lu G,et al.[10]comprehensively measured the VAS score through the AUC curve,and concluded that the EA group had lower pain scores and higher pain relief satisfaction.The meta-analysis of Halpern SH,et al.[9]and Anim-Somuah M,et al.[13]compared EA with opioid intravenous analgesia,and the results showed that patients’ satisfaction with EA was better than opioid intravenous analgesia.Two other meta-analysis compared EA and no analgesia with other analgesic measures,and the results showed that patients with EA were more satisfied,and the difference was statistically significant.
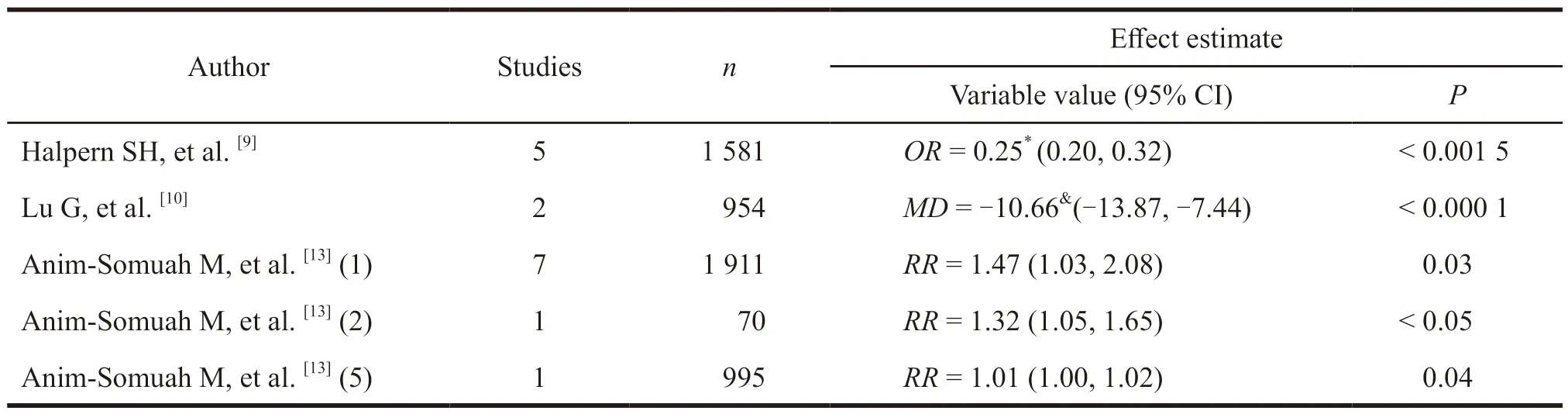
Table 14 Summary of meta-analysis of pain relief satisfaction
3 Discussion
In this study,a re-evaluation of systematic review method was used to assess the safety and effectiveness of epidural labor analgesia in order to provide evidence for the application of EA in labor.
In the methodological quality evaluation process of systematic reviews,3 systematic reviews did not consider the publication status in the inclusion and exclusion criteria,and 2 did not provide a list of inclusion and exclusion documents.It is difficult to judge whether the inclusion and exclusion of the literature is accurate.Three systematic reviews did not evaluate the scientific nature of the included studies,suggesting that the original literature could be biased.Four systematic reviews did not detect publication bias,suggesting that there might be publication bias that misled readers.Seven systematic reviews did not report the conflict of interest included in the original study.Therefore,the overall quality of the reports included in the analysis is not high.
For safety indicators,the incidence of EA is higher than that of opioid intravenous analgesia and transcutaneous neuromuscular electrical stimulation.This may be due to the need for intravenous infusion of saline solution before EA,resulting in maternal plasma oxytocin concentration decreased[14].Besides,obstetricians are more likely to perform deviceassisted delivery due to maternal uterine weakness[9].Scholars at home and abroad generally believe that epidural block will trigger the inflammatory reaction in the women to cause fever[15-18].In addition,the compensation of blood vessels above the block level will reduce heat dissipation,and the block of cold and heat will not be synchronized,resulting in the occurrence of maternal temperature regulation center disorder.It is also one of the important causes of fever during childbirth,which is consistent with the conclusions of this article.Opioids used for nausea and analgesia can cause nausea,vomiting,respiratory depression and other adverse reactions[19-21].Therefore,the incidence of nausea and vomiting in EA is lower.Through analysis,it is found that EA can block maternal sympathetic nerves,reduce maternal hyperventilation,and improve the acid-base balance of newborns[22],which cuts the incidence of neonatal acidosis and neonatal asphyxia.Regarding the time of labor,EA can prolong the time of the first and second stages of labor compared with opioids[9,13].But compared with no analgesic measures,there is no statistically significant difference in the impact of labor.
Regarding the rate of cesarean section,most domestic studies showed that EA could reduce the rate of cesarean section[23-27].But different meta-analysis had reached the opposite conclusion,which may be the intervention of EA in each study with different methods of administration,type of administration,concentration of administration,duration of administration,leading to clinical heterogeneity.Regarding effectiveness indicators,EA has better pain relief and higher maternal satisfaction.
Limitations of this study:Only published systematic reviews are included,and unpublished systematic reviews are not included.Search time is up to August 2020,and the emergence of new evidence may affect the results.
In summary,based on the current meta-analysis evidence,EA can increase the rate of device-assisted delivery,cause maternal fever and prolong the first and second stages of labor.But the incidence of back pain,nausea,and vomiting is lower,suggesting that EA has certain advantages in the effectiveness of labor analgesia.Limited by the number and quality of the included studies,the conclusions of this study need to be verified by more studies.It is recommended that more studies be carried out to provide high-quality evidence for the clinical promotion of labor analgesia.
- 亚洲社会药学杂志的其它文章
- Drug Regulatory Science in EU and Its Enlightenment to China
- Research on the Status of Patent Protection of Prostaglandin Analogues for Glaucoma in China
- Exploration on the Implementation of the Integration of Medical and Preventive Model in China’s Primary Health Care Institutions
- The Development of DTP Pharmacy and Its Impact on Pharmaceutical Enterprises
- Comparative Analysis of Social Forces Participating in Emergency Management of Public Health Events in China,Australia,Germany and the United States
- The Investigation and Research of the Performance Appraisal of R&D Personnel in R Company

