Exploration on the Implementation of the Integration of Medical and Preventive Model in China’s Primary Health Care Institutions
Chen Hui,Wang Shuling
(School of Business Administration,Shenyang Pharmaceutical University,Shenyang 110016,China)
Abstract Objective To explore the different modes and approaches of medical and preventive integration in current primary health care institutions in China.Methods Through literature analysis,field research,telephone interviews,and other methods the implementation status was evaluated to systematically study the main experience and effect of implementing medical and preventive integration services in pilot areas.Results and Conclusion At present,there are three implementation modes of medical-prevention integration,namely,vertical mode based on the medical community,internal mode with optimized service process,and internal mode with great service capabilities.The three medical-prevention integration modes have their respective focuses,but they need to be further improved in terms of policy support,technical staffing,information system construction,and drug use.
Keywords:primary health care institution;medical and preventive integration;model
Since 2018,the National Health Commission of the People’s Republic of China has successively issued relevant documents to encourage local governments to actively explore and provide integrated and continuous medical and health services.Therefore,many regions in China have taken the management of key people with chronic diseases such as hypertension and diabetes as the entry point in the primary health work,studying the model of medical and preventive integration.They provide residents with the health services of preventing diseases first,preventing changes of the diseases,and preventing new illness after recovery.After closely integrating prevention and treatment in all links,they can better meet the needs of the people for health services in the new era.
1 Current status of primary health care institutions
Primary health care institutions mainly include community health service centers (stations),street/township health centers,village clinics,outpatient departments,and clinics (infirmaries).They are the foundation of China’s medical service network,occupying an important position in the medical system.
1.1 Current status of the number of primary health care institutions
At present,the new medical reform is at the critical moment,and primary care,as the focus of the reform,is the key breakthrough target.With the introduction of a series of policies,the function expansion and capability enhancement of the primary medical system have been promoted[1].From 2013 to 2019,the number of primary health care institutions continued to grow,as shown in Fig.1.By the end of 2019,there were 960 000 primary health care institutions in China,accounting for 94%of medical institutions.Among them,the number of township health centers was 36 000,the number of community health service centers (stations) was 35 000,the outpatient department (institute) was 267 000,and the village health room was 621 000.This service network can offer the timely medical services to residents in China.
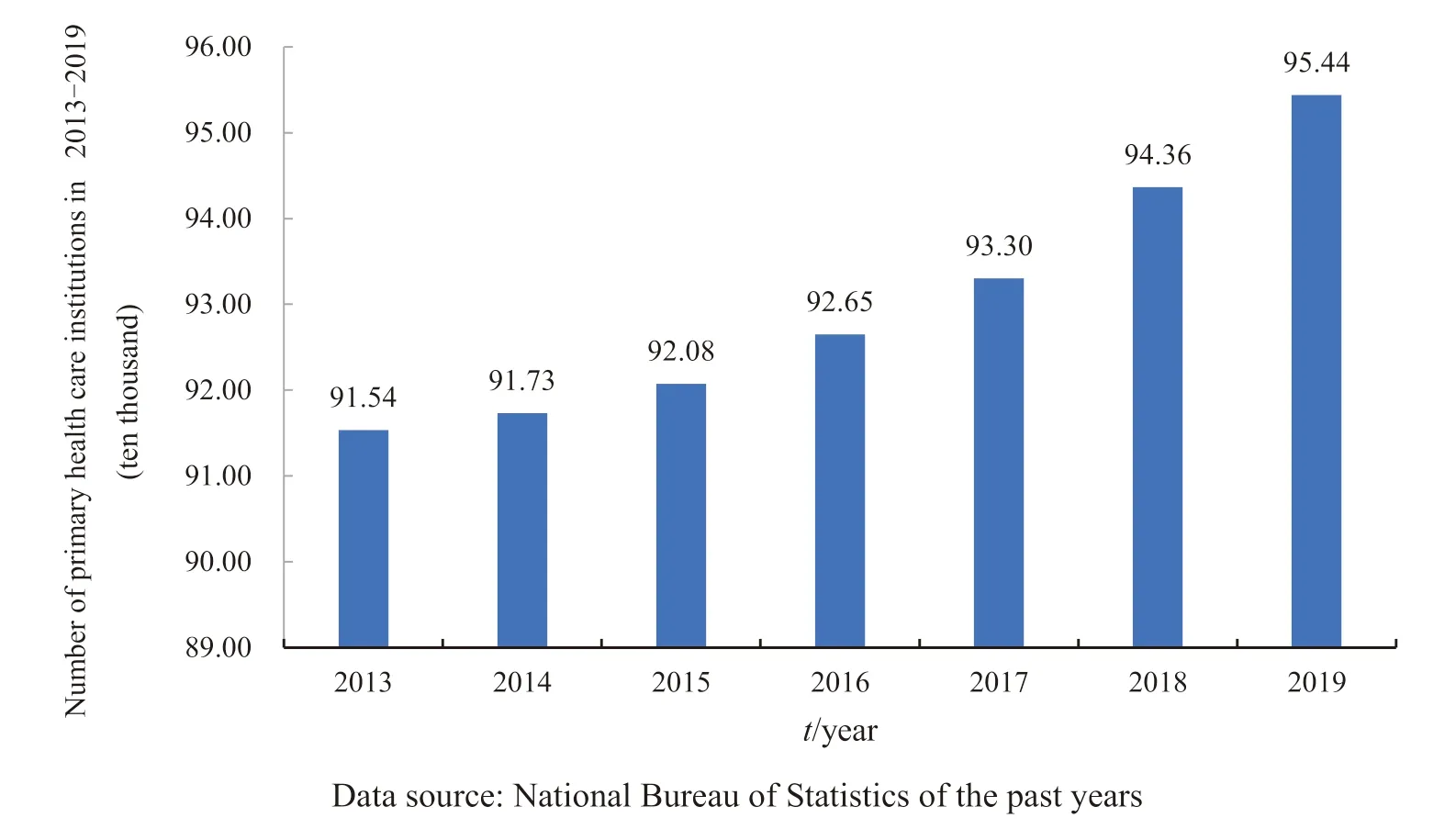
Fig.1 Changes in the number of primary health care institutions from 2013 to 2019
1.2 Service characteristics of primary health care institutions
Primary health care institutions have the characteristics of diversified services[2].They can provide residents with both consultation services and on-site services.They have close contact with residents and are easily recognized by them.The service model is flexible and efficient.At the same time,with the standardized management of basic public health services,grassroots institutions can establish family health files for residents.Therefore,they have a clearer grasp of the health status of residents in the community,and can meet the medical needs of different patients in a timely manner.
2 The connotation of medical and preventive integration
2.1 Interviewing key figures to explore the connotation of the integration
As to the connotation of medical and preventive integration,the directors of the grassroots departments of local health committees and relevant experts in the field of public health were interviewed.Then,the opinions of 15 interviewees were collected.As they were familiar with the basic medical work,their opinions came from their work experience and theoretical analysis.Lastly,the comments of peers were referred to ensure the objectivity of their answers.
In the study,some respondents believed that the integration of medical and preventive medicine was the deepening of the combination of prevention and treatment,which could not only reflect the integration of medical and public health services,but also the integration of service teams,business management,information systems,and performance appraisal.Some respondents thought that medical and preventive integration meant service suppliers horizontally integrated resources to provide continuous medical services for specific clients (such as patients with chronic diseases).Other respondents believed that the integration should focus on the prevention and treatment of chronic diseases,and combine clinical diagnosis and treatment with follow-up management and health education.
2.2 Literature analysis on the development of medical and preventive integration
As early as 2011,“Difficulties and Countermeasures of Providing Continuous Health Services to Urban Communities in China” put forward the basic concept of integration of medicine and prevention.That is,breaking the barriers between medical treatment and prevention,and turning from disease diagnosis and treatment to paying attention to the health status of residents in the whole life cycle.In 2015,Shanghai University of Traditional Chinese Medicine published an article called “Shanghai University of Traditional Chinese Medicine and Wanda Information Set Up Medical and Preventive Integration System for Health Management”,which once again mentioned medical and preventive integration.It stressed that both Chinese and Western medicine should develop together,and the health management of “prevention,treatment and control”of chronic diseases must be carried out.Later,some regions started the mode of medical and preventive integration.For instance,Anhui Jieshou,known as the“Xiaogang village”,made some achievement while implementing medical and preventive integration[3].Luohu and other regions also formed a new mode of medical and preventive integration with their characteristics.In 2018 and 2019,the primary health care department of the National Health Commission issued an official proposal on medical and preventive integration,which took hypertension and diabetes as the breakthrough point.Besides,pilot work of integration was carried out in seven provinces and cities,including Shanxi,Chongqing and Guizhou.
2.3 Analysis on the connotation of medical and preventive integration
Based on the above contents,the connotation of medical and preventive integration should be divided into three levels:macro level,medium level and micro level.All the integration should focus on providing high-quality health management services for residents to maintain their health.
At the macro level,medical and preventive integration is the management integration,including fund allocation,service control and service provision management mechanism.The basic health services provided by primary health care institutions are integrated with financing and payment for medical treatment.Therefore,the management is taken as a whole.Besides,supervision and assessment mechanism of basic public health services are coordinated to divide the responsibility to each party involved[4].
As to the medium level,it means different types of medical institutions are cooperating to provide excellent health services through resource sharing.This can realize the efficient medical and preventive integration[5].On the other hand,institutions of the same type and level can provide the same services through the exchange of information and resources,forming a scale effect.This can help provide high-quality services of homogeneity.
The integration of medical and preventive services at the micro level provides continuous medical services for patients in primary health care institutions.The internal integration covers the following aspects,such as primary health care,general and specialized medical care,rehabilitation,nursing and other services.Besides,it also includes the key incentive and constraint mechanisms,and supports systems such as personnel management,financial management,performance management and information system.It provides health management services based on the need of patients[6].
3 Summary of implementation mode of medical and preventive integration in different regions
Through the analysis of the problems in basic medical services in various regions,field research,questionnaire survey,and other methods,the eff ective mode of medical and preventive integration in different regions can be summarized.Three modes are obtained.The first is the vertical integration represented by Anhui Province,as shown in Fig 2.The second is the internal integration with the optimized service process represented by Chongqing,as shown in Fig 3.The third is the internal medical and preventive integration mode with better service ability represented by Zhejiang Province,as shown in Fig 4.
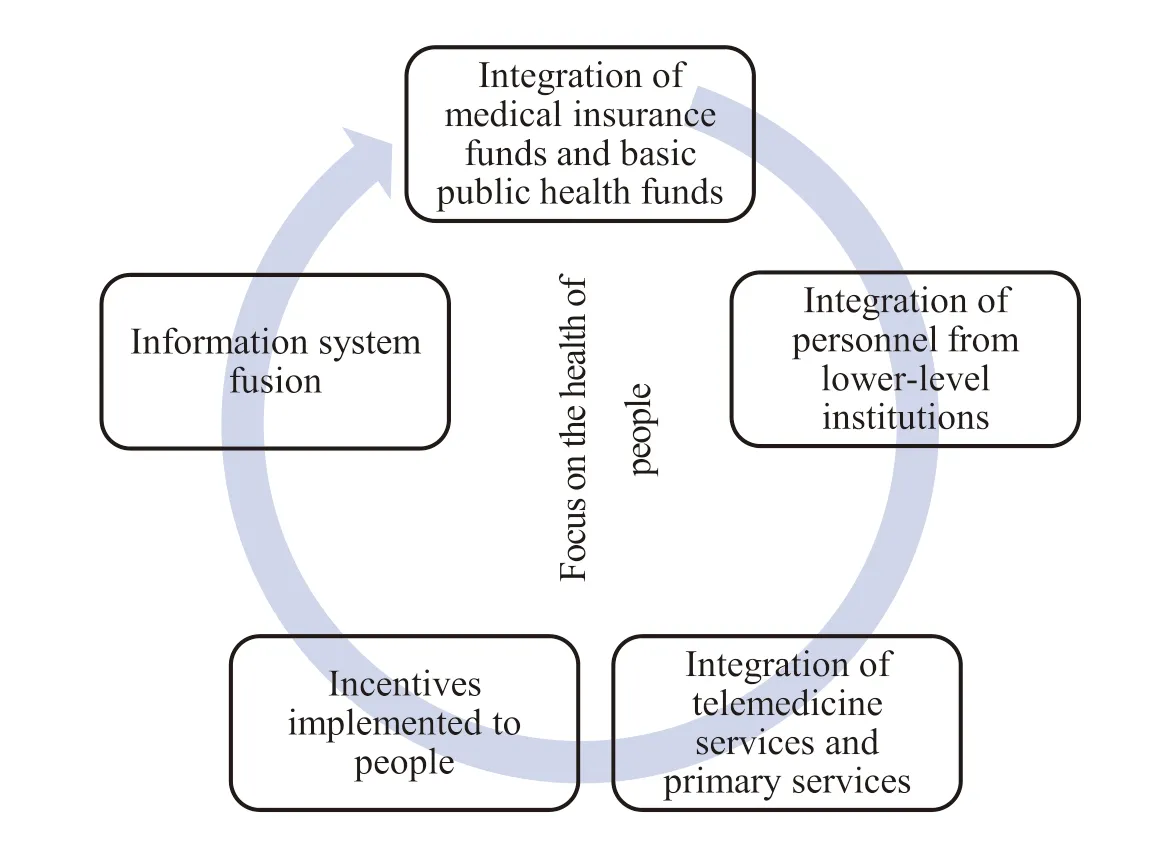
Fig.2 Mode of medicine-prevention integration approach
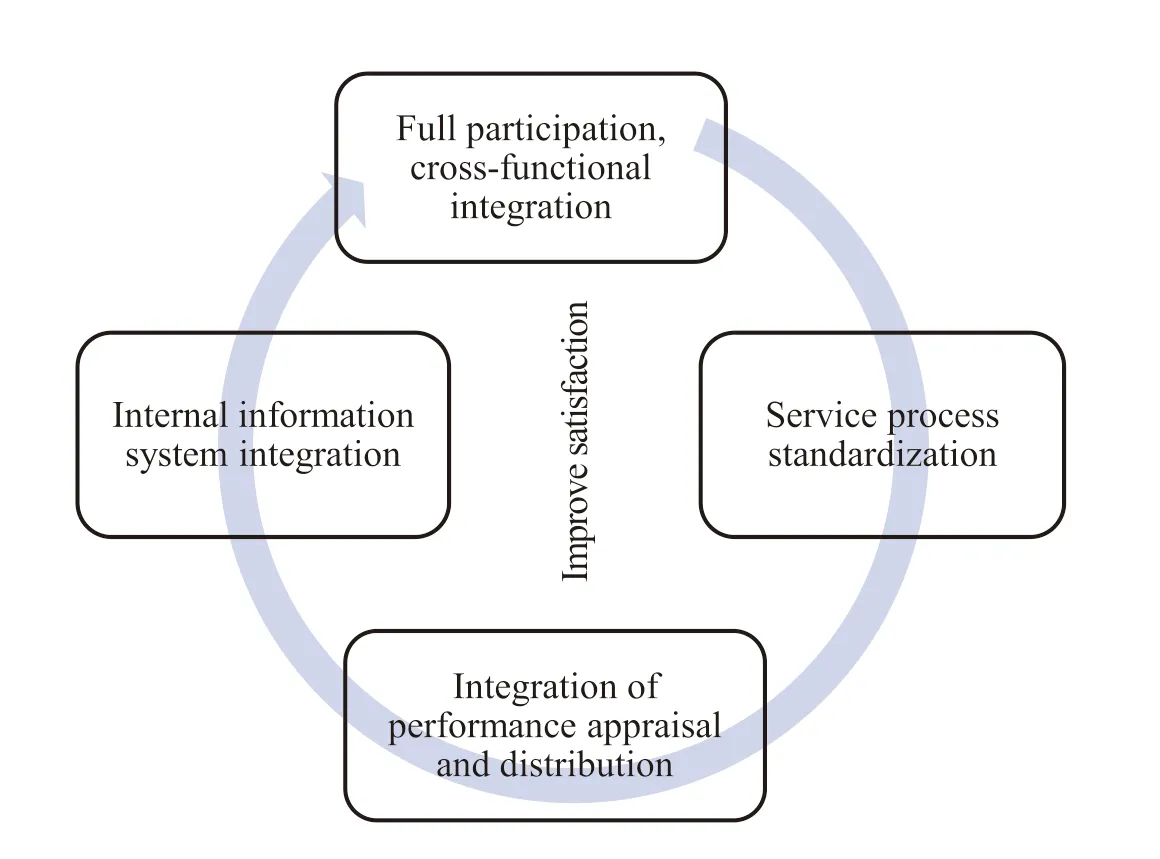
Fig.3 Mode of medicine-prevention integration approach
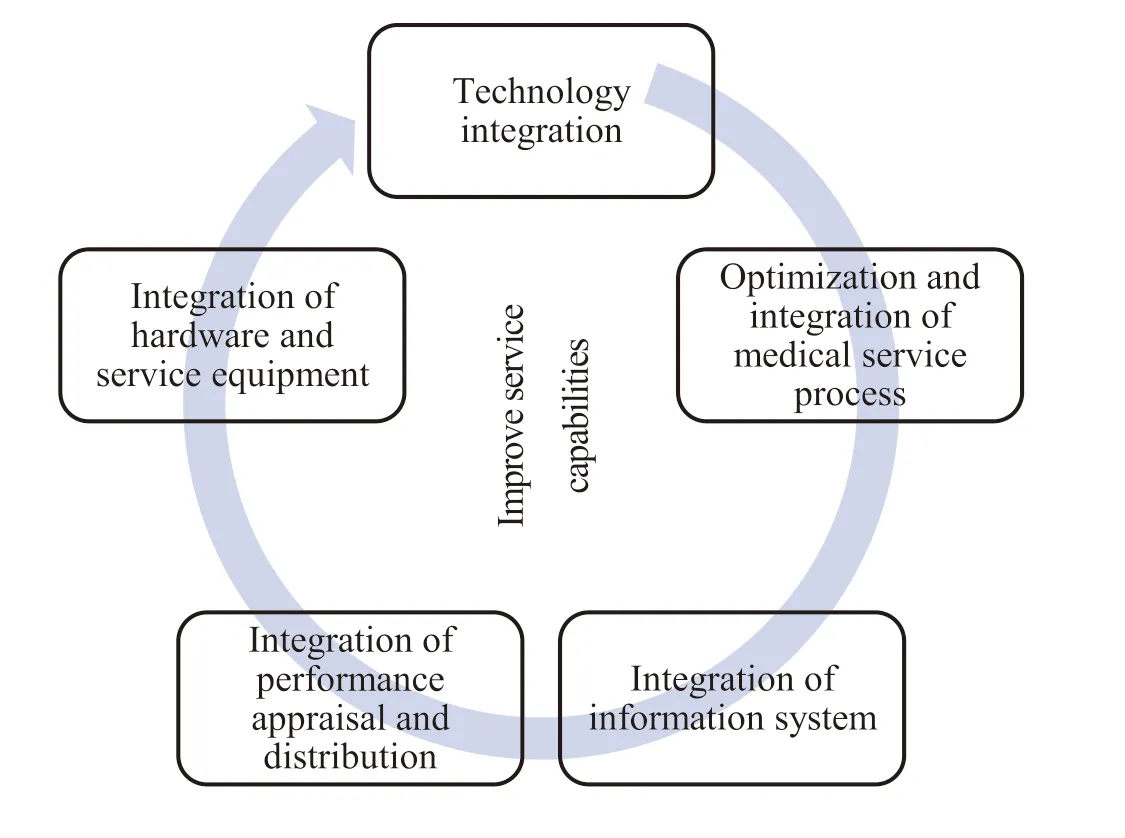
Fig.4 Mode of medicine-prevention integration approach
3.1 Mode 1:vertical integration based on medical community
3.1.1 Integration of medical insurance fund and basic public health fund
The basic medical insurance fund for urban and rural residents and the basic public health fund should be integrated.Their balance should be retained,and the overruns should be reasonably shared.Therefore,a close interest link can be established.The medical insurance management department will prepay the basic medical insurance fund according to the total number of the medical community.It will cover the reimbursement expenses of outpatient and hospitalization of residents in the current year,the contracted service fees of family doctors,and the hospitalization outside the county (excluding serious illness insurance objects).Then,the remaining funds shall be reasonably allocated to the member units of the medical community that can use independently.The financial department also allocates the funds for basic public health services in time according to the budget for the total number of the medical community.The basic medical and health institutions will be assessed and settled in the way of purchasing basic public health services.The balance of funds will be used as a whole for the reward of medical and preventive service personnel.
3.1.2 Personnel f low and integration of superior and subordinate organizations
According to the needs of primary health care institutions,higher-level hospitals uniformly arrange medical personnel to go to primary health care institutions for regular consultations and routine operations.At the same time,a long-term mechanism should be established between the higher and lowerlevel medical institutions so that the grassroots medical staff can study in higher-level hospitals.It will promote the smooth two-way flow of medical staff at the medical institutions.
3.1.3 Integration of telemedicine services and primary services
The full coverage of telemedicine means medical services can be given to all the patients.For example,the higher-level hospital establishes a platform for remote diagnosis and treatment,such as consultation,imaging,and ECG center,which will complement the shortcomings of medical services in primary health care institutions through information technology.The drugs needed in the primary health care institutions are uniformly provided by the leading unit of the medical community,including unified online procurement,unified centralized distribution,and unified payment.These measures can not only guarantee people’s medication,but also strengthen the management of clinical pharmacy.Besides,carrying out prescription reviews can ensure the safety and rationality of primary medications.
3.1.4 Incentive measures for medical personnel
The basic medical insurance for urban and rural residents is budgeted after deducting the incremental risk fund (a 10% increase in funding compared to the previous year) and the critical illness insurance fund from the total funds raised in the current year,and no less than 95% of the fund is regarded as the total people of the medical community.The balance of medical insurance funds will be rewarded to the members of doctor team in proportion.
3.1.5 Integration of information systems
An information system should be established that covers the urban and rural areas.All medical information and health information of patients in the system can be shared by medical institutions,which means patients have the electronic medical records.Besides,remote consultations and remote diagnosis centers such as imaging and ECG should be established.It enables primary health care institutions to realize remote collaboration and resource sharing with higher-level medical institutions.At the same time,some technologies such as smart wearable systems should be introduced to ensure the authenticity of residents’ health examinations and health records.
3.2 Mode 2:internal integration with optimized service process
3.2.1 Full participation,overlapping functions
In order to ensure the smooth integration of the teams,the first step is to set up a good system.Therefore,detailed rules and regulations should be formulated based on the specific conditions of the primary health care institutions to define employees work.At the same time,based on full participation,the employees are divided into multiple large teams.Each team has a leader who manages several family doctor groups,and each group is composed of a family doctor and several assistants.
3.2.2 Standardized service process
Primary health care institutions should establish a service chain,including prevention,medical treatment,chronic disease management,and rehabilitation.The family doctor team mainly uses chronic disease management as an integrated entry point,taking care of the patients they are responsible for.In addition,family doctor signing,chronic disease management,and elderly management will become the daily work of general practitioners.
3.2.3 Principle of assessment and performance
The performance of public health workers will be included in their overall performance appraisal and distribution plan,which also will be linked with the service effect of the family doctor team.The weight design of medical and public health is determined according to the actual situation of the institution.Meanwhile,there are three-level appraisal modes in performance appraisal,namely,department appraisal,group appraisal,and member appraisal.Besides,specific appraisal rules are set up for different positions.In a word,the principle of distribution is more work,more pay.
3.2.4 Integration of internal information systems
You can think of this as being girl power at work in the animal kingdom, he said. We like to think of reproduction as being all about the males competing for females, with females dutifully picking the winner. But in reality females have much more invested than males, and they are making highly strategic decisions about their reproduction based on the environment, their condition and the quality of their mate. Amazingly, the female is somehow picking the sperm that will produce the sex that will serve her interests the most: The sperm are really just pawns in a game that plays out over generations.
The construction of the hospital information system (HIS) and public health management system should be strengthened to realize the collaboration and information sharing between diagnosis and public health services.Therefore,clinicians can access the information of residents’ health files,and public health doctors can inquire about medical information,which realizes the collaboration and information sharing between medical treatment and public health services.The medical and preventive integration mode of “disease prevention+precision treatment+health promotion” can be established based on health file query,health management and health education.
3.3 Mode 3:internal integration with highlighted service capabilities
3.3.1 General practitioners improve their professional skills
The development model of “general practice +specialist” integration is to improve the professional and technical capabilities of general practitioners.Through combining their own interests,active declaration,specialized training,and learning from teachers,the number and quality of general practitioners can be enhanced.At the same time,the general practitioner can be trained to cure a certain disease.Supplemented by nurses and pharmacists,a strong team can help form the medical and preventive integration.
3.3.2 Optimized medical service process
Before consultation,patients can make appointments with contracted family doctors through online platforms or telephone.There are standardized procedures for patients’ visits.An assistant in the general practitioner’s office can provide services such as measuring blood pressure,blood sugar,dressing change,referral,consultation,file building,as well as appropriate health education.Family doctors should strengthen health education when patients visit them,and screen complications,such as early symptoms of cancer,high blood pressure,high blood sugar and other concurrent diseases.After diagnosis,longterm health services and life interventions should be provided to patients with chronic diseases.Besides,standardized management must be improved in blood pressure and blood glucose monitoring,complication screening,diagnosis and treatment procedures,and treatment plans for patients.
3.3.3 Improvement of inter-institutional and intrainstitutional information systems
The internal medical system in the primary health care institution is connected with the public health system.The transparency of patient’s information in the hospital can maintain the continuity of patient’s visit.At the same time,a complete two-way referral channel will be established between the primary health care institutions and the higher-level hospital.When a patient at the primary health care institution chooses to be transferred to a higher-level hospital for treatment,he or she can apply to the responsible doctor directly.After passing the examination,the patient can directly go to the higher-level hospital for treatment without having to register again.Doctors in higher-level hospitals can use patients’ medical insurance cards to retrieve their health files and medical records in primary health care institutions for more information.
Professional assessment standards should be set up for medical treatment and public health separately.Setting performance distribution weights can help the personnel of primary health care institutions attach equal importance to medical treatment and public health.The professional contents of public health assessment and medical assessment should be compiled by the assessment personnel according to specific service assessment standards.At the same time,in order to improve the skills of grassroots personnel,the job skills competition should be normalized,which will be included in the comprehensive quantitative incentives performance of the year.This can build a dual-pronged work pattern that combines the quantity and quality of medical and public health services.
3.3.5 Convenient equipment and sound measures
(1) Providing rental services.Some primary health care institutions provide patients with free medical equipment rental services and instructions for use,including but not limited to nebulizers,oxygen generators,blood glucose meters,etc.,which will reduce the number of patients’ visits to hospitals and they return them after treatment.
(2) Customer service.A customer service center is set up to communicate,answer questions,and collect information from contracted residents and clients with the help of internet technology.Active communication with key management objects can realize continuous health management and reduce telephone troubles of general practitioners during working hours.
3.4 Comparative analysis of different modes of the integration
The above fusion models in this study have their respective focuses in the implementation process.Besides,they have some commonalities and differences in the close contact with higherlevel hospitals,family doctor team design,primary service provision,and information development(Table 1).
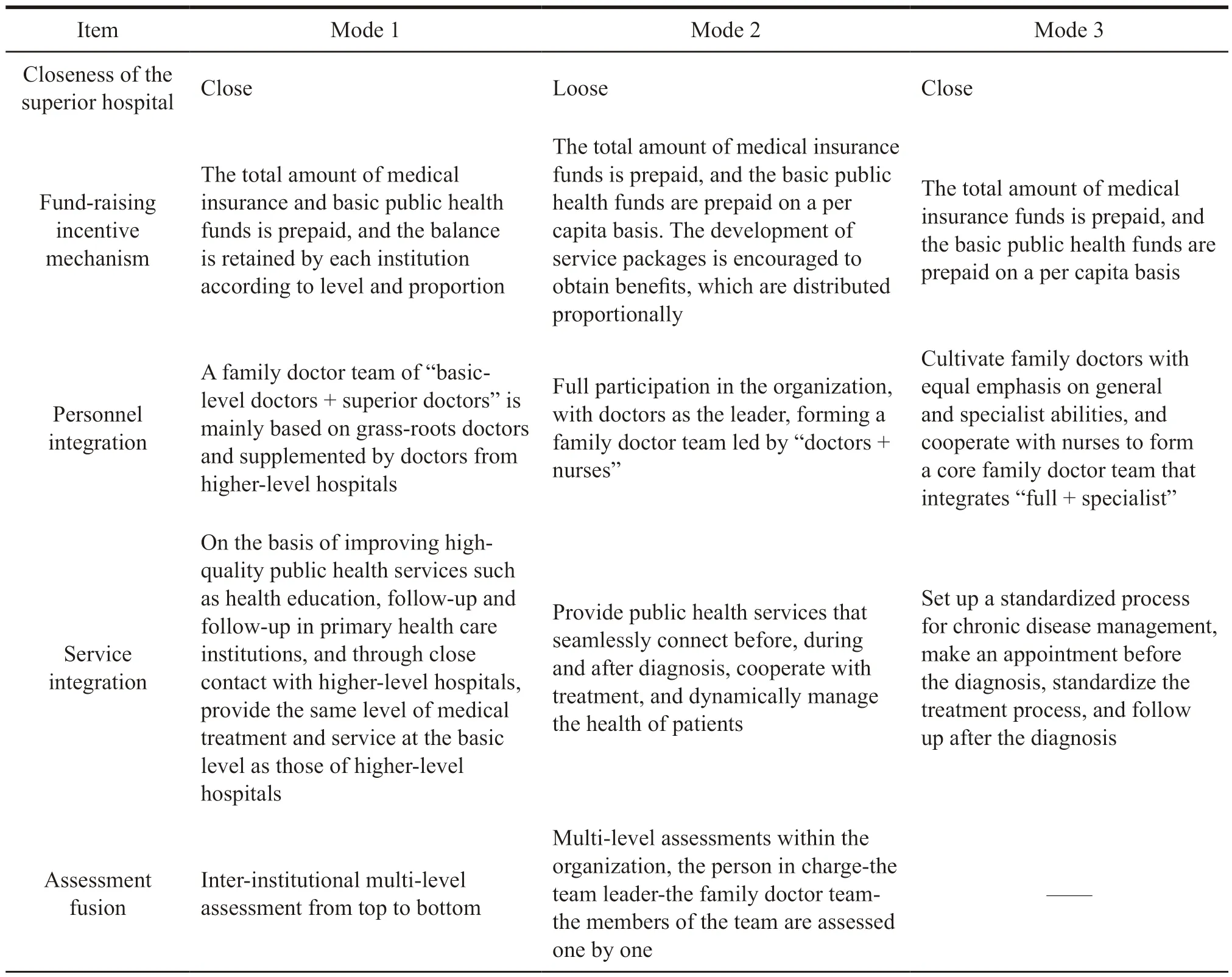
Table 1 Comparison of three fusion models
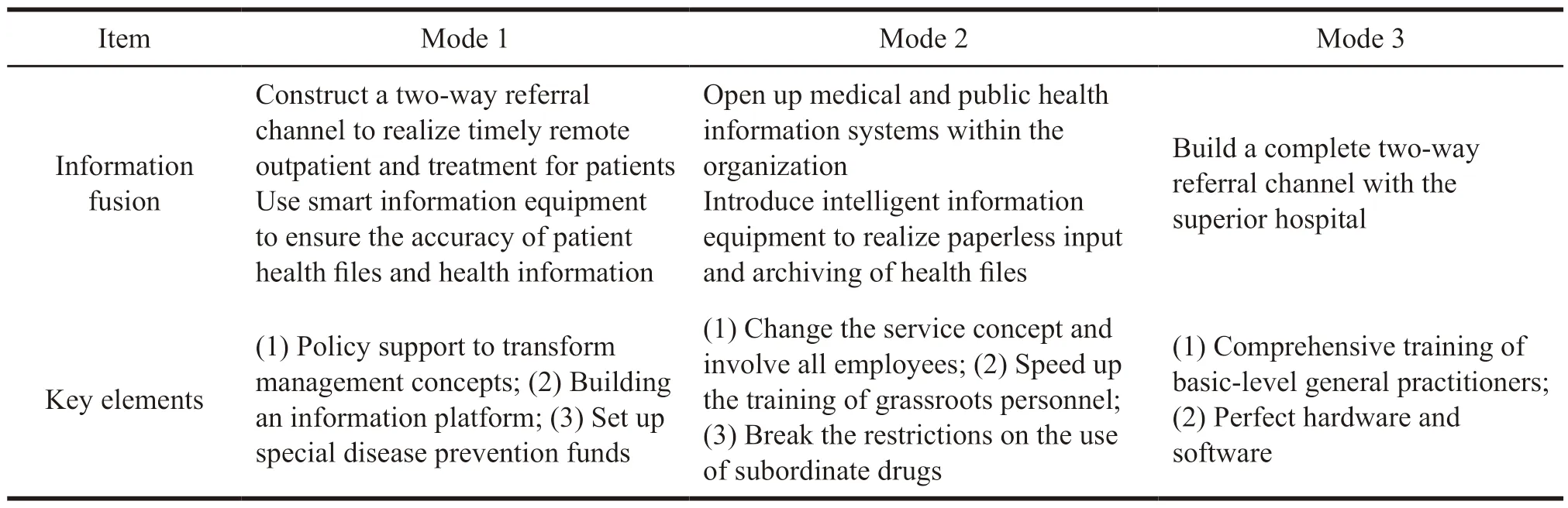
Continued Table 1
These three integration models have their respective focuses in the implementation process.
Mode 1 focuses on the close integration of primary health care institutions and higher-level medical institutions with stronger medical service capabilities.Its biggest feature is that the family doctor team is composed of the grassroots doctors and superior doctors.However,the main force of the family doctor team in mode 2 and mode 3 are the internal personnel of the primary health care institution,forming a relatively fixed team responsible for patients management.Their connection with the superior hospital is relatively loose,and the experts in superior hospitals regularly help.
Mode 2 focuses on optimizing the internal service process of primary health care institutions.It establishes standardized services,breaking the barriers between medical and public health work in the institution,which realizes that all employees in the institution participate in the implementation of medical and preventive integration.Finally,the overall improvement of service capabilities will be achieved,thus providing patients with continuous and dynamic health management.Therefore,patients are willing to choose the first consultation at the grassroots level hospitals,which achieves a positive treatment cycle.
Model 3 focuses on highlighting service capabilities within medical and health institutions and the service capabilities of general practitioners.Meanwhile,standardized service processes and active performance allocation strategies are adopted to provide patients with the rental medical equipment,which will bring patients a good medical experience and increase its competitiveness.
4 Suggestions
4.1 Strengthening the construction of primary medical personnel
4.1.1 Strengthening the training of general practitioners
At present,medical and health personnel are a key factor in improving the service capacity of primary health care institutions.Referring to the experience of primary health care in other countries,we can see that general practitioners provide local residents with basic medical and public health services.They not only treat most minor diseases of the residents,but also offer disease prevention services.Therefore,they have played a great role in implementing medical and preventive integration in primary health care institutions.However,since the establishment of the general practitioner system in 2011,the number of general practitioners in China is still seriously insufficient.The government should speed up the training of general practitioners for primary health care institutions[7].
4.1.2 Increasing the number of health personnel and improving the quality of health services
Health service personnel are a major factor in the process of medical and preventive integration,but they are currently in a serious shortage.First,we should determine the scale of health personnel in China.After calculating the minimum allocation and the average allocation standards of health personnel,we can introduce talents to improve the service capabilities of primary health care institutions[8].After the introduction of health personnel,it is necessary to ensure the stability of the health personnel team by increasing their salaries and the proportion of the total expenditure of health institutions.In addition,the professional knowledge training of the grass-root personnel should be strengthened,thus exploring a transport mechanism for higher and lower medical personnel.
4.2 Improving the allocation of primary medical equipment
Nowadays,the primary health care institutions in China have a low level of medical technology and equipment.In many rural areas,primary health care institutions have outdated and incomplete types of medical equipment.Besides,different regions have different requirements for the medical technology and equipment.Therefore,the higher level of primary health care institutions such as municipal health bureau,the provincial health bureau,and the national health bureau should appropriately increase the investment ratio in accordance with the actual situation of the primary health care institutions in the region during the macro coordination[9].
At the same time,in order to improve the use of special funds and the efficiency of equipment for primary health care institutions,the types and total quantities of equipment that meet the medical needs of regional residents should be determined.In-depth investigation and research can be conducted by experts from the medical field.Considering economic benefits,fairness and accessibility,and the basic conditions of the service population,economic development,and transportation of region where the health institution is located,we can work out classification standards at province,city,and county levels.They are the basis for the assessment and supervision of the service capabilities of primary health care institutions.So the technological equipment for primary health care institutions is practical,scientific,advanced and economical.
4.3 Opening up the drug use channel between the upper and lower institutions
Under China’s current medical insurance policy and drug system,drug use in primary-level hospitals are strictly restricted by the “National Essential Drug List” and the “Medical Insurance Drug List”.Primary health care institutions should be given the right to purchase drugs independently to avoid drug shortages or late delivery,which can restrict the normal work.At the same time,distribution companies should be selected reasonably,and drug supply supervision must be strengthened as well.A special national information platform can be built to ensure timely drug supply.So each province and city should complete the supplementary list of essential medicines according to the differences of regional disease to ensure the basic drug supply.
4.4 Speeding up informatization construction
As to outpatient service,inpatient service,general medical treatment management,and twoway referral management service,relevant national standards and regulations can be referred to form norms and procedures that meet the development of local primary health care institutions.In addition,inhospital information platforms should be set up to improve service levels in these primary health care institutions[10].
- 亚洲社会药学杂志的其它文章
- Drug Regulatory Science in EU and Its Enlightenment to China
- A systematic Review of the Safety and Effectiveness of Epidural Analgesia for Labor Analgesia
- Research on the Status of Patent Protection of Prostaglandin Analogues for Glaucoma in China
- The Development of DTP Pharmacy and Its Impact on Pharmaceutical Enterprises
- Comparative Analysis of Social Forces Participating in Emergency Management of Public Health Events in China,Australia,Germany and the United States
- The Investigation and Research of the Performance Appraisal of R&D Personnel in R Company

