Locoregional therapies and their effects on the tumoral microenvironment of pancreatic ductal adenocarcinoma
Thomas Lambin, Cyril Lafon, Robert Andrew Drainville, Mathieu Pioche, Frederic Prat
Abstract Pancreatic ductal adenocarcinoma (PDAC) is expected to become the second leading cause of death from cancer by 2030 . Despite intensive research in the field of therapeutics, the 5 -year overall survival is approximately 8 %, with only 20 % of patients eligible for surgery at the time of diagnosis. The tumoral microenvironment (TME) of the PDAC is one of the main causes for resistance to antitumoral treatments due to the presence of tumor vasculature, stroma, and a modified immune response. The TME of PDAC is characterized by high stiffness due to fibrosis, with hypo microvascular perfusion, along with an immunosuppressive environment that constitutes a barrier to effective antitumoral treatment. While systemic therapies often produce severe side effects that can alter patients’ quality of life, locoregional therapies have gained attention since their action is localized to the pancreas and can thus alleviate some of the barriers to effective antitumoral treatment due to their physical effects. Local hyperthermia using radiofrequency ablation and radiation therapy - most commonly using a local high single dose -are the two main modalities holding promise for clinical efficacy. Recently,irreversible electroporation and focused ultrasound-derived cavitation have gained increasing attention. To date, most of the data are limited to preclinical studies, but ongoing clinical trials may help better define the role of these locoregional therapies in the management of PDAC patients.
Key Words: Pancreatic ductal adenocarcinoma; Tumoral microenvironment; Stroma;Hyperthermia; Radiation therapy; High-intensity focused ultrasound
INTRODUCTION
Pancreatic ductal adenocarcinoma (PDAC) is one of the most common types of pancreatic cancer[1 ].Given the rapidly increasing incidence of PDAC in recent decades, it is expected to become the second leading cause of cancer death by 2030 in the United States and other industrialized countries[2 ]. The 5 -year survival rate is approximately 8 % following diagnosis[3 ], with only 20 % of the patients eligible for surgery[4 ]. Among the patients who undergo surgery, the 5 -year survival rate is only 20 % due to rapid recurrence and metastasis development[5 ]. Systemic treatments are associated with various types of adverse events that result in a poor quality of life for patients[6 ] and are often inefficient due to the characteristics of the PDAC tumor microenvironment (TME), which protects tumor cells from chemotherapies and immunotherapies. The TME is increasingly being considered a potential target of choice to improve outcomes for PDAC. Locoregional treatments, such as hyperthermia (HT) with microwave ablation or radiofrequency ablation (RFA), radiation therapy (RT), irreversible electroporation (IRE), and high-intensity focused ultrasound (HIFU) therapy, are gaining increasing attention for their ability to specifically target the tumor while limiting deleterious systemic adverse events and may often be used in combination with anticancerous drugs. Among other effects, locoregional therapies can induce changes in the structure, components, and properties of the TME that may help alleviate some of the barriers to successful treatment. In this review, we will summarize the characteristics of the TME in PDAC and describe the effects of locoregional therapies on vasculature, stroma, and immune response. We will pay special attention on characterizing the TME for clinical applications(Table 1 ).
PDAC MICROENVIRONMENT
Although most solid tumors develop specific interactions with their hostvianeoangiogenesis, the creation of a supporting network of cells and extracellular matrix, and some form of immunomodulation, PDAC remains one of the most stroma-rich cancers, with 90 % of its tumor mass composed of fibroblasts and their products[7 ]. The PDAC stroma is composed of an acellular and cellular compartment. The acellular compartment consists of an extracellular matrix rich in collagen, fibronectin,laminin, integrins, glycosaminoglycan, matrix metalloproteinase and secreted protein acids and is rich in cysteine[1 ,8 ] with cytokines and growth factors[9 ]. The cellular component is composed of pancreatic stellate cells and immune cells, such as macrophages, mast cells, lymphocytes, and plasma cells[1 ].Pancreatic stellate cells, which are resident cells of the pancreas, acquire an activated myofibroblast-like phenotype when activated and are assumed to be the main regulators of TME extracellular matrix production. With the tumoral microvasculature, all these elements form the TME. Interactions between acellular and cellular components of the TME are key factors in PDAC progression[10 ]. In PDAC, the TME has been associated with tumoral progression, metastasis dissemination, and resistance to chemotherapy by various mechanisms[8 ]. The abundant extracellular matrix increases intratumoral interstitial pressure[11 ] and acts as a barrier for drug delivery with compression of blood vessels. Tumor stiffness can also have a direct effect on chemosensitivity:in vitro, mechanically compressed PDAC spheroids (displaying high stiffness) are less sensitive to gemcitabine than free spheroids (without any mechanical compression), whereas there is no difference in Hoechst dye penetration between compressed and free spheroids, suggesting a therapeutic effect of compression independent of the solepenetration of gemcitabine into the spheroid cells[12 ]. One hypothesis to explain this phenomenon is that mechanical stress decreases cell proliferation, which may alter the efficacy of chemotherapies targeting proliferating cells[12 ]. Intratumoral stiffness itself can modify intracellular signaling pathways and promote epithelial-mesenchymal transition, leading to tumoral progression and chemoresistance[13 ]. In PDAC, the microvascular density is generally low and leaky. Combined with mechanical forces caused by the dense stroma and tumoral growth that compresses the vessels, limited perfusion can result, which is responsible for hypoxia and low nutrient availability along with low anticancer drug delivery[1 ,14 ]. On the immune response side, the TME in PDAC is characterized by a reduced number of cytotoxic T cells, along with an increase in M2 macrophages, N2 neutrophils, and T-regulatory cells at the tumor site, which all contribute to an immunosuppressive environment[15 ].
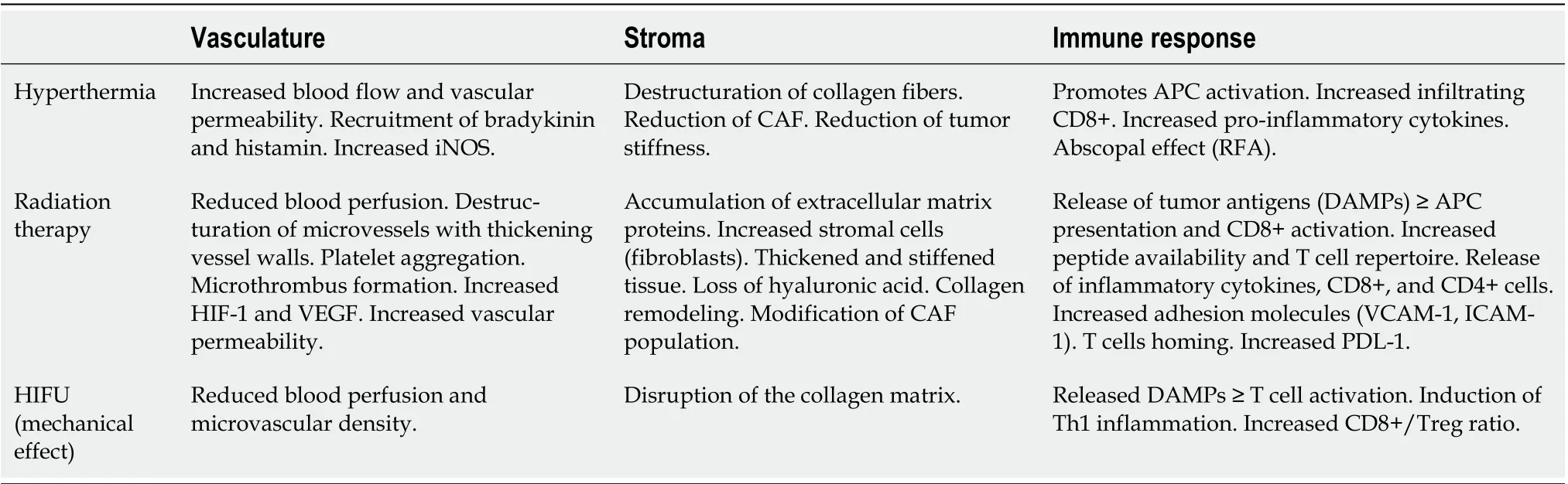
Table 1 Locoregional therapies and their main effects on the tumoral microenvironment of pancreatic ductal adenocarcinoma
Current studies suggest that the TME is an attractive target in the management of PDAC. Provenzanoet al[11 ] showed that the administration of an enzymatic agent allowing the deletion of stromal hyaluronic acid (PEGPH20 ) in a murine model of PDAC led to normalized intratumoral interstitial pressure, expansion of the tumoral microvasculature, and increased survivalin vivowhen combined with gemcitabine compared to gemcitabine alone. However, caution should be taken since other studies have shown that the presence of some TME elements serves to prevent cancer progression and should therefore not be suppressed indistinctively[16 ,17 ]. In a mouse model of PDAC, as well as in patients with pancreatic cancer, a decreased bulk of aSMA + myofibroblasts was associated with poor prognosis and reduced overall survival[17 ].
HT
HT is a therapeutic procedure used to increase the intratumoral temperature. There are various ways to increase temperature: for superficial tumors, local HT can be applied by means of antennas or applicators that emit microwaves (microwave ablation) or radio waves (radiofrequency ablation or RFA) placed at the surface of the tumor with an intervening medium. Interstitial and endocavitary HT are used for small tumors in which an intratumoral implantation of the antenna can deliver various types of waves: microwaves, radiofrequency, ultrasound, heat sources, or laser fibers. Regional HT and partial body HT are more suitable for deep seated tumors, such as PDAC, that can be heated by antennas placed in rings around the patient. Whole-body HT is dedicated to the treatment of metastatic tumors[18 ]. HT can be generated by an external source, such as hot air or infrared radiation, or an internal source, such as magnetic nanoparticles, which can be deposited in the region of interest and then exposed to a magnetic field, leading to an increase in temperature and allowing localized heating[magnetic hyperthermia (MHT)][14 ]. Nanoparticles can also be used for photothermal therapy (PTT),during which a laser can activate nanophotoabsorbers. MHT and PTT are both nanoparticle-based HT treatments[19 ,20 ].
Hyperthermia and tumoral vasculature
HT is thought to increase blood flow and vascular permeability with an increase in antitumor effects. A study by Miyamotoet al[21 ] evaluated the effects of mild HT on the efficacy and accumulation of an anti-EGFR agent (cetuximab) in various xenograft mouse models of pancreatic cancer. Using a water bath, a temperature of 37 °C or 41 °C was applied to the tumor and allowed to decrease the tumoral volume compared to mice exposed to a standard ambient temperature of 25 °C (control). This was accompanied by an increase in cetuximab accumulation in cancer cells by 2 .5 - to 5 -fold, depending on the model studied. Of note, this effect was also observed when stromal dense tissue derived from surgically resected pancreatic cancer was transplanted into mice. This effect may be due to an increase in blood flow with an increase in tumor vessel permeability[22 ]. Indeed, another study showed that mild HT in a mouse model of pancreatic cancer could induce an 11 -fold increase in blood perfusion in a reversible manner during heating and a 3 -fold increase after the end of HT treatment along with an increase in vasculature permeability and an enhanced extravasation of macromolecules[23 ]. In a xenograft mouse model of breast cancer, non invasive radiofrequency (RF) produced increased transport and perfusion of fluorescent tracers into the tumors at temperatures below 41 °C, whereas vessel deformation and blood coagulation were observed when the temperature reached 44 °C[24 ]. The mechanism through which HT increases blood perfusion may be linked to a relaxation of smooth muscle following an increase in nitric oxide synthetized by endothelial cells. In a study by Songet al[25 ], the content of inducible nitric oxide synthase (iNOS) was evaluated in a murine model of fibrosarcoma following HT. No iNOS was detectable before HT treatment, while an increase in iNOS was observed 3 h after HT and remained detectable 24 h after treatment. Additionally, HT increases the recruitment of bradykinin and histamine molecules responsible for vessel dilation and the recruitment of capillaries[26 ].
Hyperthermia and stromal architecture
HT has been shown to disrupt the stromal architecture. In a study by Piehleret al[14 ], Achilles tendons(mainly composed of type I collagen) were exposed to various regimens of either extrinsic or ion-oxide nanoparticle-based MHT. The amount of intact collagen fibers decreased with the application of HT,with only 10 % of collagen fibers intact after 1 h of the 42 °C regimen and almost complete degradation after 1 h of the 50 °C or 70 °C regimen. Mild HT applied to spheroids of pancreatic cancer cells (Panc1 )and fibroblasts (WI 38 ) significantly decreased the amount of intact collagen fibers, with a coinciding decrease in spheroid volume and cell viability by apoptotic and necrotic processes[14 ]. Local HT through the use of a photothermal agent combined with a photothermal-chemotherapeutic agent(Abraxane@Mose2) and subsequently irradiated by a laser beam could disrupt tissue architecture and reduce the number of carcinoma-associated fibroblasts (CAFs), subsequently enhancing the efficacy of Abraxane in a mouse model of PDAC[27 ]. Similarly, in a mouse model of cholangiocarcinoma, a nanoheater used for PTT (multifunctional iron oxide nanoflowers decorated with gold particles) with high uptake by CAFs produced a significant depletion of CAFs as well as a reduction in tumor stiffness followed by significant tumor regression[28 ]. In another study by Marangon et al[29 ], tumor stiffness was monitored following PTT in squamous cell carcinoma in mice. Shear wave elastrography revealed a transient and reversible increase in tumor stiffness after thermal ablation or mild HT, followed by a return to its initial value within 24 h of laser exposure in the case of thermal ablation or a reduced level for mild HT. Additionally, while increased tumor stiffness was observed in untreated mice, the stiffness in the treated group was stable over time. In the same study, second harmonic generation was used to evaluate the effect of PTT on collagen structure and revealed a destructuration of collagen fibers in the vicinity of heated carbon nanotubes.
In several mouse models of pancreatic cancer displaying various levels of stroma formation, the concomitant application of mild hyperthermia and cetuximab induced a more significant antitumoral effect on stroma-rich models[21 ].In vitro, noninvasive RF has been shown to affect molecular transport in a 3 D model of PDAC with increased diffusion of DAPI fluorescence in spheroids following RF compared to no treatment[30 ]. In a xenograft mouse model of squamous cell carcinoma, the combination of MHT and doxorubicin demonstrated a more efficient reduction in tumor growth than doxorubicin alone[31 ]. In the same study, the space between collagen fibers was determined following MHT: while there were no differences between the control group and the group injected with nanocubes without exposure to a magnetic field (no HT), there was an increase in the interfibrillar space between the group injected and exposed to the magnetic field compared to the injected group without exposure to the magnetic field[31 ].
Hyperthermia and immune response
Data on the effect of HT on the immune response in PDAC are scarce, but the literature is abundant for other types of cancer. HT promotes antigen presenting cell (APC) activation and antigen-specific naïve CD8 + T cell differentiation, allows CD4 + T cells to shift towards the Th1 phenotype, and transforms regulatory T cells (Tregs) into Th17 cells[32 ]. In a mouse model of PDAC, RFA induced an increase in infiltrating CD8 + T cells and a decrease in Treg cells but showed no difference in the proportion of infiltrating CD4 + lymphocytes[33 ]. HT has been shown to induce chemokine production, such as CCL21 ,combined with adhesion factors (selectin, integrin, ICAM-1 ), thus allowing an increase in the interactions between lymphocytes and endothelial cells and the homing of lymphocytes[34 -37 ]. In parallel, HT induces the production of various proinflammatory cytokines, such as IL6 [38 ]. HT induces immunogenic cell death through various mechanisms[32 ], such as triggering DNA damage that produces mutations in tumor cell genes, which generate neoantigens that stimulate the T cell-based immune response[32 ,39 ]. HT can also generate damage-associated molecular patterns (DAMPs), of which heat shock proteins (HSP) are the most important but also include molecules such as calreticulin,HMGB1 or ATP. HSPs are chaperones that participate in the presentation of the chaperoned antigen to the MHC-1 complex of dendritic cells, thus allowing antigen-specific T-cell activation[34 ,35 ,40 ]. High levels of HSP are associated with poor prognosis in parallel to an enhanced immune response[32 ].Membrane HSP has been found to be a tumor-specific target for natural killer cells, whereas extracellular HSP can be considered a potent adjuvant to facilitate tumor antigen presentation and the induction of antitumor immunity[32 ,41 ,42 ]. More specifically, HSP70 has been shown to induce tumor cell proliferation in a mouse model of PDAC by activating AKT-mTOR signaling[33 ]. HSP60 has been shown to induce IFNg secretion and T cell upregulation[43 ]. In a murine model of PDAC, a study by Linet al[44 ] found that the maximum HSP synthesis was achieved at 43 °C, corresponding with an increased antitumor immune response. Beyond this temperature, both the release of HSP and the associated immune response decreased[34 ,44 ]. The accumulation of neoantigens, secondary to mutations and DAMPs, favors the activation of dendritic cells, allowing the transformation of the tumoral immunosuppressive microenvironment by inhibiting Treg cells and promoting tumor-infiltrating lymphocyte maturation[32 ].
The so-called “abscopal effect” has often been invoked to suggest that an immunomodulating mechanism had to take place when the local treatment of a malignant tumor - most commonly the use of RT - results in a response at a distant location[45 ,46 ]. In a PDAC mouse model implanted with tumors on both flanks, Feiet al[47 ] tried to determine whether RFA on one flank’s tumor could affect the untreated tumor located on the other side. After RFA on one side, the immune response on the opposite side showed an increase in CD8 +/PD-1 + T cells, along with suppression of immunosuppressive components of the tumor microenvironment (i.e., Tregs, tumor-associated macrophages, and tumorassociated neutrophils). Additionally, immune checkpoints such as PD-1 and LAG3 were upregulated in distant (untreated) T cells after one-sided RFA. Similarly, Gameiroet al[48 ] found that RFA induced local immunogenic modulation at the tumor surface in a model of colon adenocarcinoma, and the combination of RFA with vaccine therapy eradicated both primary and secondary tumors. Finally, in a clinical study for 10 patients with locally advanced pancreatic cancer (LAPC) that evaluated the immune response following coagulation necrosis-inducing RFA ablation, an increase in CD4 +, CD8 +, and effector memory T cells along with IL 6 was seen[49 ].
RT
RT uses an ionizing radiation beam (X-rays) whose energy is deposited in water along its path, leading to the formation of free radicals (reactive oxygen species or reactive nitrogen species) that oxidize molecular targets, provoking a dysregulation of cellular functions. These free radicals target DNA,leading to single- or double-strand breaks[50 ]. Today, there is no consensus on the role of RT in PDAC.The LPA07 trial did not show any improvement to the tumor in a small number of fractions to minimize the impact on the surrounding organs.
Radiation therapy and tumor vasculature
The effect of RT on tumor vasculature has been widely explored in various types of cancers. RT has been shown to have many direct or indirect effects on endothelial cells[50 ], and these effects are dependent on the dose received and the radiation schedule[51 ]. High single doses of radiation have been shown to cause vascular damage with reduced blood perfusion and hypoxia[52 ]. RT induces changes in tumor vasculature by destructuring microvessels and thickening vessel walls, thus reducing vessel lumen, all of which favor atherosclerosis. RT also induces platelet aggregation and microthrombus formation with an increase in inflammatory cell adhesion to endothelial cells[53 ]. RT can regulate and stabilize the level of HIF-1 , leading to the production of VEGF, which is responsible for endothelial cell proliferation and increased survival. RT can directly upregulate the expression of avb3integrins[54 ] and adhesion proteins[50 ]. In pancreatic cells, HIF-1 has been shown to induce the sonic hedgehog protein, leading to the formation of a stroma-rich microenvironment[55 ]. In a rodent model of pancreatic tumor, a single high dose (SHD) of radiation led to temporary vascular dysfunction along with enhanced expression of HIF-1 , which could be restored after 14 d. However, vascular permeability was higher in irradiated tumors 14 d after RT[56 ]. Similarly, a study by Lee et al[57 ] evaluated the effect of an SHD of radiationvsa fractionated regimen of radiation, which showed increased perfusion ability of tumor vessels following SHD, whereas fractionated RT had no effect. Mechanisms were further studied and showed that vessels treated with SHD-RT had lower pericyte coverage; increased vessel perfusion could therefore be due to an increased leakage of immature vessels, and the surviving vessels after SHD-RT might favor the penetration of small molecule drugs.
RT and stroma
RT induces chronic inflammation, leading to fibrosis through the accumulation of extracellular matrix proteins and an increase in stromal cells such as fibroblasts[58 ], which thicken and stiffen the tissue[51 ,59 ]. Fibrosis formation depends on the dose of radiation received. For example, in a 3 D model of mammary cancer stroma, increasing RT doses resulted in a reduction in fibroblast proliferation and activation along with a modest increase in matrix stiffness[60 ]. RT induces a loss of hyaluronic acid along with a remodeling of collagen and a modification of CAF population[50 ]. Protease activity is also altered with an upregulation of MMP2 [61 ], which is responsible for an increase in tumor invasiveness[58 ].In vitrostudies showed that human lung fibroblasts develop an irreversible senescent phenotype after exposure to a radiation dose higher than 10 Gy, while lower doses induced reversible DNA damage without growth arrest[51 ,62 ,63 ]. Senescent fibroblasts can release proteolytic enzymes,cytokines, growth factors, and ROS, creating a protumorogenic environment[49 ,57 ,64 ]. Similarly,in vitro, the coculture of ionizing radiation-exposed CAFs with pancreatic cancer cells enhanced the invasion-promoting capacity of CAFs, induced a high secretion of CXCL12 (a chemokine implicated in hematopoietic stem cell maintenance and cell migration) by CAFs, and promoted pancreatic cell migration, invasion, and epithelial-mesenchymal transition[65 ].
RT and immune response
RT has been shown to modulate the immune response by various mechanisms, the first of which is the release of tumor antigens, whereby DAMPs allow APC presentation and CD8 + activation followed by cell death, called immunogenic cell death. RT can also increase peptide availability and activate mTOR,leading to an increase in the MHC-1 protein subunit and an increase in the T cell repertoire[66 ]. RT induces the release of inflammatory cytokines such as IFNviathe cGAS-STING pathway, which is activated by DNA damage caused by RT[67 ]. Adhesion molecules are also upregulated, with an increase in VCAM-1 and ICAM-1 leading to increased infiltration of lymphocytes to tumor cells and affinity binding to CD3 + cells[68 ]. Finally, RT facilitates homing of T cells to the TME by upregulating chemokines such as CXCL16 [69 ]. In a murine orthotopic pancreatic cancer model, irradiated tumors displayed increased CD8 + and CD4 + cells, with a high single dose of RT being more efficient in recruiting CD8 + T lymphocytes than fractionated RT. However, fractionated RT induced more infiltration of myeloid-derived suppressor cells than high-dose RT[57 ].In vitro, RT increased the expression of PDL-1 in a Jack/stat1 -dependent manner[70 ]. Evidence to date suggests that immunotherapy such as anti-CTLA-4 or anti-PD-1 in PDAC has disappointing results or displays efficacy only in patients with PDAC who test positive for mismatch repair deficiency or microsatellite instability-high (MSI-h) due to the poorly immunogenic nature of PDAC[71 -74 ]. Some data suggest that the combination of RT with immunotherapy could be a future approach to overcome this limitation. In a study by Leeet al[57 ], the combination of SHD-RT with anti-PD1 increased the delivery of anti-PD1 in a murine orthotopic mouse model of PDAC (UN-KC-6141 ), which is consistent with the increased tumor perfusion observedin vivofollowing RT. The survival of mice receiving a combined treatment of anti-PD1 /SHD-RT was significantly improved compared to that of mice receiving anti-PD1 or SHD-RT alone. Splenocytes isolated from mice treated with the combination therapy showed increased cytotoxicity specifically toward UN-KC-6141 cells. In addition, while the combined group was free of peritoneal tumors, all of the control, SHD-RT, and anti-PDL1 alone groups bore metastases. This encouraging result is in accordance with anotherin vivoPDAC mouse model study by Fujiwaraet al[75 ] reporting increased survival following a combination of anti-PD1 therapy and RT.
HIFU
HIFU is a noninvasive therapeutic technique using a focused ultrasound beam to create either thermal effects or a mechanical effect called cavitation at the focal point. With respect to thermal effects, due to the focal concentration of energy delivery, HIFU is capable of producing rapid coagulation necrosis with limited inflammatory response and minimal damage to the TME outside the focal zone, inside of which the TME is destroyed. Otherwise, the effects of HT on the TME have been described above in a dedicated section. With respect to the mechanical effect of HIFU, acoustic cavitation can be defined as the initiation, growth, oscillation, and collapse of gas bubbles inside a medium due to high tensile acoustic pressures that exceed cohesion forces between molecules. When exposed to an acoustic field, a bubble will oscillate radially (regime of stable cavitation) and possibly collapse (regime of inertial cavitation). At the tissue level, stable cavitation can stretch tight junctions and allow the extravasation of molecules from the vascular to interstitial space, making the plasma cell membrane transiently permeable and allowing for the internalization of molecules. Comparatively, inertial cavitation is more violent and may induce irreversible membrane disruption and cell implosion or hemorrhage in tissues[76 ]. HIFU is regularly used in prostate cancer or in the management of uterine fibroids[77 ,78 ] but also in the management of PDAC, although it is much less common. HIFU has been suggested to improve quality of life and alleviate pain in patients with a metastatic course of their disease[79 ].
To date, few preclinical studies have evaluated cavitation as a potentiator of chemotherapy with promising results. A previous study from our group evaluated the impact of various inertial cavitation intensities combined with gemcitabine on the viability of PDAC spheroids composed of both KPC pancreatic cancer cells and activated fibroblasts designed to mimic the tumor stroma[80 ]. Even if this model was far from a PDAC tumor, it possessed some of its essential features, including the presence of activated fibroblasts, the production of extracellular matrix and a dense intercellular arrangement. This work demonstrated that inertial cavitation decreased the viability of spheroids exposed to cavitation and gemcitabine compared to either cavitation alone or gemcitabine alone. Moreover, gemcitabine had no impact on fibroblast viability, whereas the effect of chemotherapy on the viability of PDAC cells was enhanced when combined with cavitation. Of note, the effects of gemcitabine toxicity were less evident in spheroids composed of both KPC cells and fibroblasts compared to those composed of KPC cells only, which is consistent with the protective effect of the TME and supports the benefit of the combination[80 ].
In 2015 , Li et al[81 ]. showed in KPC mice that cavitation with pulsed HIFU enhanced the intratumoral concentration of doxorubicin by 4 .5 -fold compared to controls, with an increase in doxorubicin concentration when cavitation was high and sustained. Of note, there were no differences when pulsed HIFU was delivered during or before doxorubicin administration. On the pulsed HIFU-treated tumors,macroscopic evaluation revealed hemorrhagic areas, while microscopic evaluation showed disorientation and separation of the collagen matrix with fraying of collagen fibrils. A study by Huanget al[82 ] evaluated the impact of cavitation induced with an ultrasound contrast agent (microbubble) in a mouse model of pancreatic cancer. Blood perfusion evaluated by contrast-enhanced ultrasound imaging revealed a decrease in blood flow within the tumor after cavitation treatment compared to pretreatment measurements, whereas blood perfusion of nontumoral tissue was not impacted. Immunostaining of blood vessels also showed decreased expression of CD31 and reduced microvascular density in the cavitation group.
On the immunotherapy side, the mechanical effects of HIFU have been shown to induce subcellular fragmentation, leading to the release of DAMPs that are subsequently presented to dendritic cells[83 ]and trigger cytotoxic T cell activation[84 ]. Pulsed HIFU or low-intensity HIFU have been shown to drive Th1 inflammation, to stimulate localized cell recruitment factors and tumor cell surface immunogenic proteins, and increase the CD8 +/Treg ratio[85 ]. However, these data come from non-PDAC tumor types.
IRREVERSIBLE ELECTROPORATION
IRE is a nonthermal ablative therapy using a direct high voltage current with a short pulse length to increase cell membrane permeability, resulting in permanent cell death with minimal thermal deposition[86 -88 ]. IRE is applied by placing two or more electrodes in the tumor or around it[89 ] and can be used intraoperatively, laparoscopically, or percutaneously. IRE induces damage only to the cell membrane and has no effect on protein denaturation, blood flow, and connective tissue[88 ] and was first described for the treatment of human pancreatic cancer in 2012 [90 ].
Studies on the specific effects of IRE on the PDAC stroma are scarce. One study by Bhutianiet al[91 ]described an increase in gemcitabine delivery to the tissue located in the electroporation area in mice treated by IRE compared to untreated mice. Even if mechanistic explanations were not explored, this effect may be attributable to IRE-related alteration of the stroma. TME modulation following IRE is also characterized by a transient increase in microvascular density and an increase in tumor blood vessel permeability along with a softening of the extracellular matrix can lead to an increase in T cell infiltration[92 ]. IRE can induce microvessel endothelial cell apoptosis with microvessel thrombosisin vivo[93 ]. In a xenograft mouse model of PDAC, alterations of tumor microstructure were described following IRE in which acute coagulative necrosis and thrombosis were visible throughout the treated tumor volume after IRE, whereas minimal thrombosis was observed in the control group (no treatment).Using transmission electron microscopy, microvessel endothelial apoptosis and microvessel thrombosis were visualized, and magnetic resonance imaging (MRI) analysis revealed a significant increase in water diffusion after IRE, with a reduction in diffusion-weighted MRI images reflecting an increase in diffusion (water mobility) in the tissue after IRE[93 ].
From an immunologic point of view, available data are limited: a mouse study by Yanget al[94 ]described an increase in calreticulin after IRE, suggesting an induction of immunogenic cell death, with an increase in the intratumoral expression of CD8 + cells and GrB (granules of enzymes expressed by cytotoxic lymphocytes) when IRE was combined with a dendritic cell vaccine. In the same study,stromal fibrosis formation was not modified following IRE. In another study by Whiteet al[95 ], IRE was found to induce an increase in macrophage, T cell, and neutrophil infiltration within the tumor.
CLINICAL PERSPECTIVES
Hyperthermia
In accordance with mouse studies showing an increase in drug delivery with hyperthermia, a recent systematic review evaluated the clinical benefit of HT (regional, intraoperative, or whole-body HT)combined with chemotherapy, RT or both in 248 patients. Out of 14 studies, 6 showed a longer median overall survival in the HT group compared to the control group, with an 11 .7 mo median survival vs 5 .6 mo. The response rate was also higher in the HT groups[96 ]. These encouraging results have prompted randomized clinical trials to more clearly demonstrate any benefit of this therapeutic approach. A phase II study (HEATPAC-NCT02439593 ) is currently recruiting to compare deep locoregional HT administered with a microwave system (Aim 40 -43 °C for 60 min) with chemotherapyvschemotherapy alone in LAPC. The results from this study could provide a practical assessment of the efficacy of HT in PDAC[97 ]. Other current studies are summarized in Table 2 .
RFA in PDAC has been reported in small exploratory series for tumor debulking rather than for complete tumor ablation because safety margins are needed to avoid thermal damage to surrounding structures[98 ]. Following RFA combined with chemotherapy, overall survival ranges from 19 to 25 .6 mo[98 ,99 ]. There is a lack of randomized studies assessing the place of RFA in the management of LAPC.The PELICAN trial (NCT03690323 ) is planned to evaluate whether the combination of chemotherapy and RFA improves overall survival compared to chemotherapy alone in patients with LAPC without any progression after 2 mo of systemic treatment[100 ] (Table 2 ).
Endoscopic application of RFA, which is already feasible, is an attractive approach because of its minimal invasiveness. The active component is a 19 G needle that has a tip equipped with an electrode to be placed in the lesion under endoscopic ultrasound (EUS) guidance. This approach has been proven safe and feasible in small-sized studies of patients with unresectable PDAC[101 -103 ]. Nevertheless,larger prospective studies are needed. EUS-RFA clinical trials are ongoing (Table 2 ), and it would be interesting to evaluate EUS-RFA as an alternative to RT in LAPC patients with an objective response to chemotherapy who retain criteria against surgical resection.
RT
Stereotactic body radiotherapy (SBRT) is increasingly being explored for the management of PDAC in combination with anticancerous drugs, especially for LAPC. An open-label phase 2 multicenter study by Hermanet al.evaluated the combination of gemcitabine plus SBRT in patients with LAPC, showing a good safety profile[104 ]. Similarly, 39 patients who underwent FOLFIRINOX followed by SBRT seemed to have an increased chance of undergoing radical surgery[105 ]. SBRT in combination with immune therapy is also being studied. In a phase I study by Xieet al[106 ], a combination of immune therapy(durvalumab ± tremelimumab) with SBRT in metastatic PDAC showed a favorable safety profile but only a modest clinical efficacy. Of note, none of the responders were MSI-h. While these results are interesting, further exploration is required, and many clinical trials are underway to evaluate the combination of SBRT or RT with anticancerous drugs (Table 2 ). A challenge for the use of SBRT is the required placement of fiducials to facilitate the delivery of radiation, which can be made difficult by respiratory movements and the vicinity of other organs[107 ]. These fiducials can be placed percutaneously when not impeded by surrounding organs or in a more invasive fashion, surgically.EUS-guided placement of fiducial also appears to be a promising method with a high rate of technical success and a reasonable rate of adverse events[91 ,108 ], but randomized studies are needed.
HIFU
Cavitation generated by HIFU is a very attractive method with a high potential to disrupt the stroma,thus overcoming the barrier to efficient drug delivery and stimulating the immune response in preclinical works. To date, there are no published clinical trials. However, one upcoming clinical trial(NCT04146441 ) of HIFU combined with chemotherapy (FOLFIRINOX) will determine whether focused ultrasound can increase drug uptake and overcome chemoresistance (Table 2 ). In a minimalist approach of ultrasound-induced enhancement of chemotherapy, 10 patients were enrolled in a phase I clinical trial to receive gemcitabine combined with low intensity ultrasound and microbubbles as an ultrasound contrast agent programmed to favor sonoporation, with encouraging results in terms of the number of chemotherapy cycles tolerated and median overall survival when compared to 63 historical controls receiving only chemotherapy[109 ].
HIFU is also a very attractive approach to increase the intratumoral temperature and increase drug delivery. In a monocentric retrospective study among 523 patients, a combination of HIFU with gemcitabine appeared to produce better overall survival than standard CT in unresectable PDAC[110 ].The PanDox study is a phase I study that plans to evaluate whether HIFU can increase the amount of drug delivery (doxorubicin or heat-sensitive doxorubicin) within the tumor in 18 patients with unresectable PDAC (NCT04852367 , Table 2 ).
Challenges in the method of ultrasound delivery still need to be addressed, since extracorporeal delivery to the deeply seated pancreas with gas interposition could be challenging. We are currently working on an endoscopic device that could overcome these limitations and noninvasively deliver cavitation at any part of the pancreas. The endoscopic approach to HIFU delivery, foreseen by our team some time ago[111 ], has also been recently studied in a porcine model[112 ].
Irreversible electroporation
After the landmark study by Martinet al[90 ] and subsequent large series of intraoperative applications[86 ], less invasive percutaneous IRE has shown promising results in terms of efficacy. A nonrandomized prospective single-center case series by Maet al[113 ] evaluated the efficacy of a combination of percutaneous IRE with gemcitabine compared with gemcitabine alone. The combination increased theoverall survival from the time of diagnosis by 3 -fold and nearly doubled the progression-free survival.In apost hoccomparison of data derived from a prospective IRE-FOLFIRINOX cohort and a retrospective FOLFIRINOX-only cohort, van Veldhuisenet al[114 ] found that the combination (30 LAPC patients) increased the time to progression compared to standard therapy (22 patients). Lin et al[115 ]showed promising results with IRE combined with allogenic natural killer cell immunotherapy with an increase in progression-free survival and overall survival. However, a multicenter prospective study by Ruaruset al[116 ] (PANFIRE II) described a high rate of adverse events in patients undergoing percutaneous IRE, with 29 out of 50 participants experiencing adverse events, 21 of which were major,and 2 deaths, including one clearly related to IRE. Thus, this procedure can be considered a high-risk procedure that requires the selection of patients who will benefit the most from the treatment. This high rate of adverse events, along with a relative cumbersomeness to set up, has limited the spread of this technique. New application methods are needed to overcome these issues. Many clinical trials are ongoing to better understand the benefits of combining IRE with chemotherapy or immunotherapy(Table 2 ).
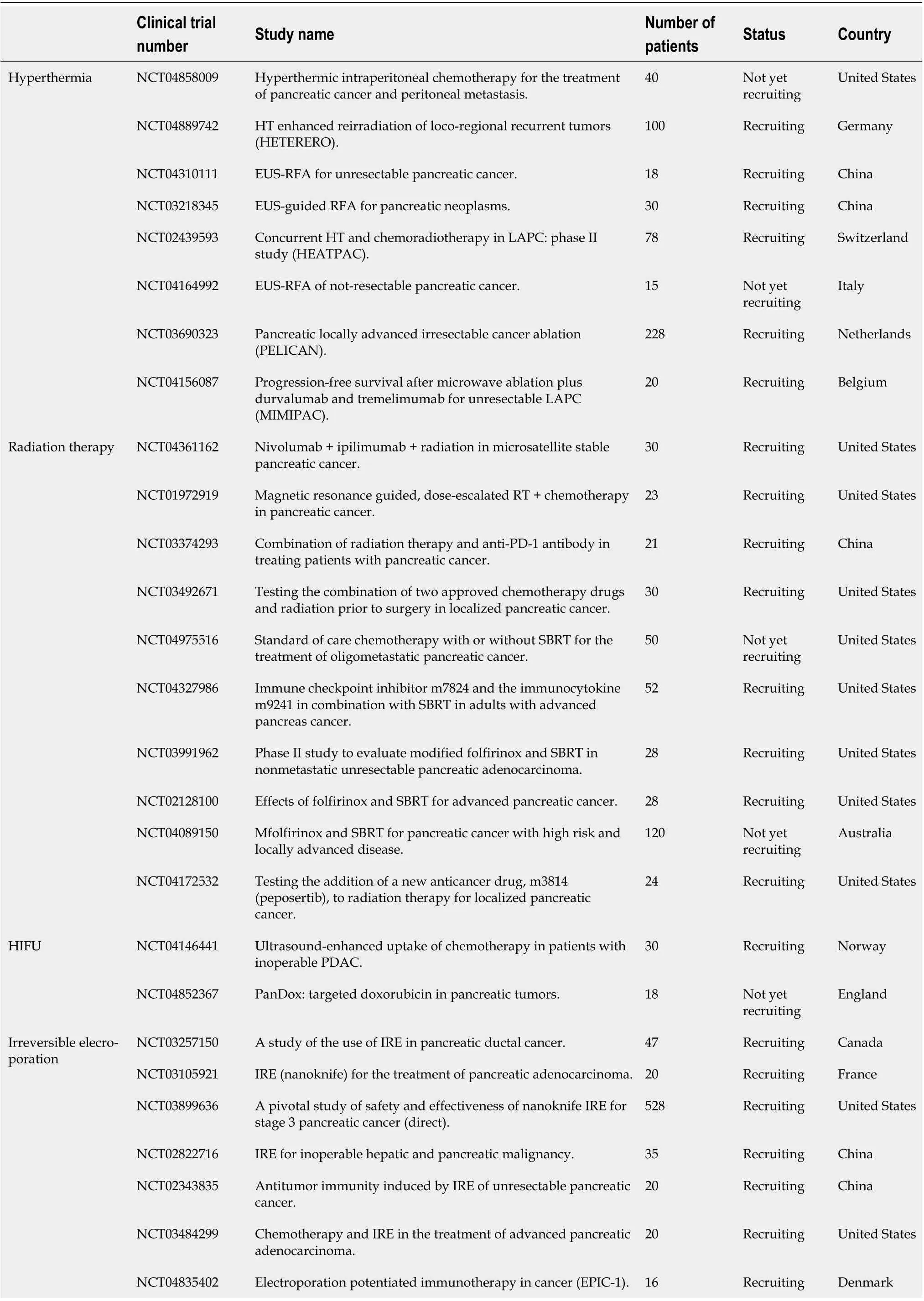
Table 2 Ongoing studies in locoregional therapies used alone or in combination with chemotherapy or immunotherapy for pancreatic ductal adenocarcinoma

HT: Hyperthermia; EUS: Endoscopic ultrasound; RFA: Radiofrequency ablation; LAPC: Locally advanced pancreatic cancer; RT: Radiation therapy; SBRT:Stereotactic body radiation therapy; PDAC: Pancreatic ductal adenocarcinoma; IRE: Irreversible electrotherapy.
CONCLUSION
The TME is one of the major causes of therapeutic resistance in PDAC. Fibrosis-related stiffness,hypomicrovascular perfusion, and an immune suppressive microenvironment are, within the limits of current knowledge, key determinants of this resistance. While systemic chemotherapies and immunotherapies have disappointing results and are responsible for adverse events resulting in poor quality of life, locoregional therapies can specifically target the tumor area with limited effects on surrounding tissues but significant impacts on the TME. Local HT using RFA and radiotherapy using local SHD are the two main modalities currently holding promise for clinical efficacy, but IRE and focused ultrasoundderived cavitation are also gaining increasing attention as treatments for PDAC. These techniques influence the tumor stroma, microvasculature, and immune environment and response (Table 1 ). To date, most of the data are preclinical with some promising results. Clinical trials are underway (Table 2 )and will allow the scientific community to have a more precise idea of the interest in using these treatment options alone or in combination with systemic therapies.
FOOTNOTES
Author contributions:Lambin T and Prat F reviewed the literature and prepared the manuscript; Lafon C, Drainville RA, and Pioche M contributed to and revised the manuscript; all authors approved the final manuscript.
Supported bythe Labex DEVweCan (Université de Lyon) and PCSI ITMO Cancer INSERM.
Conflict-of-interest statement:All authors declare no conflicts-of-interest related to this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4 .0 ) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4 .0 /
Country/Territory of origin:France
ORCID number:Thomas Lambin 0000 -0002 -9437 -0154 ; Cyril Lafon 0000 -0003 -1550 -970 X; Robert Andrew Drainville 0000 -0003 -2922 -9522 ; Mathieu Pioche 0000 -0002 -6482 -2375 ; Frédéric Prat 0000 -0002 -6018 -0491 .
S-Editor:Zhang H
L-Editor:A
P-Editor:Zhang H
 World Journal of Gastroenterology2022年13期
World Journal of Gastroenterology2022年13期
- World Journal of Gastroenterology的其它文章
- Therapeutic drug monitoring in inflammatory bowel disease: At the right time in the right place
- Endoscopic resection for early gastric cancer: Towards a global understanding
- Generic and disease-specific health-related quality of life in patients with Hirschsprung disease: A systematic review and meta-analysis
- Increased prognostic value of clinical–reproductive model in Chinese female patients with esophageal squamous cell carcinoma
- Comparison of the performance of MS enteroscope series and Japanese double- and single-balloon enteroscopes
- Management of incidentally discovered appendiceal neuroendocrine tumors after an appendicectomy
