An injectable hydrogel/staple fiber composite for sustained release of CA4P and doxorubicin for combined chemotherapy of xenografted breast tumor in mice
INTRODUCTION
Tumor blood vessels play a key role in tumor progression and metastasis,but they also provide an important therapeutic target for treatment of malignant solid tumors.Currently two types of therapeutic agents targeting tumor vasculature are available,namely anti-angiogenic agents and vascular disrupting agents (VDAs).Several anti-angiogenic agents such as bevacizumab,sunitinib and sorafenib,which inhibit the formation of new blood vessels,have been used clinically for treating malignant tumors,but their effects are substantially affected by tumor types and tumor heterogeneity,and as a common problem in cancer treatment,these agents may also cause tumor resistance to lower their therapeutic benefits.
Remarkably4, after weeks and weeks in the hospital, the little boy survived. His legs were extremely scarred by the vicious() attack of the animal and, on his arms, were deep scratches where his mother s fingernails dug into his flesh in her effort to hang on to the son she loved.
VDAs have been shown to have lower tumor resistance than the anti-angiogenic agents.Among the VDAs,combretastain A-4 disodium phosphate (CA4P)shows a promising anti-vascular effect by specifically destabilizing the microtubule in the endothelial cells of the tumor.Nevertheless,monotherapy with CA4P causes hypoxia and necrosis in center of the tumor but may leave tumor residue at the periphery,thus leading to a potential risk of tumor recurrence.Pre-clinical studies demonstrated that CA4Ps showed an enhanced antitumor effect when combined with other approaches such as antiangiogenic agents,chemotherapy,radiotherapy and radio-immunotherapy.In addition,the conventional systemic administration of CA4Ps almost inevitably causes cardiotoxicity with relatively low drug enrichment at the tumor site.
The emergence of controlled drug delivery systems have offered a new strategy for cancer therapy,which allows sustained maintenance of an local effective therapeutic concentration at the tumor site,thus reducing adverse effects and improving the efficacy of the drug.Compared with the controlled drug delivery systems that release a single drug,the dual or multidrug delivery systems with distinct release profiles are capable of both temporally and concentration-dependent release of different molecules to mimic the natural biological events.Inspired by this concept,VDAs and cytotoxic drugs are often entrapped in the same drug vehicles to achieve combined cancer treatment,using the nanocarriers including nanocapsules,polymer nanoparticles and other nanoplatforms.But given the symmetrical geometric structure of the nano-carriers and the diverse physiochemical properties of the drugs,these drug delivery systems can not achieve precise drug loading ratio and release schedule.In addition,as most of therapeutic nanoparticles for solid tumor treatment are administered systemically,their targeting efficacy can be influenced by their interaction with the proteins in blood,the extravasation into and interaction with the perivascular tumor microenvironment (TME) and the properties of the nanoparticles.
Local drug delivery systems such as preformed implantable scaffolds and injectable soft materials can achieve higher drug accumulation by delivering the drug directly to the tumor tissues.Up to now,two categories of local drug delivery systems have been used fortumor therapy:one is the well-established drug-loaded implant fabricated by electrospinning,casting or 3D printing,and the other isformed implants such as gels with special responsiveness to either temperature or pH of the tumor microenvironment.In particular,the themo-sensitive hydrogels contain both hydrophobic and hydrophilic components,which can undergo phase transition or swelling/de-swelling as the ambient temperature changes.Various synthetic poly-mers such as poly(N-isopropylacrylamide) (pNIPAAM),poly(ethylene oxide)-b-poly(propylene oxide)-b-poly(ethylene oxide) (PEO-PPO-PEO) and PEG-poly((lactic acid)co-(glycolic acid))-PEG (PEG-PLGA-PEG) ABA or BAB-type triblock copolymers have been widely used to prepare thermo-sensitive gels for injection at the tumor site.A wide range of chemotherapy drugs can be encapsulated in these injectable gels for single or dual drug delivery.Yu et al fabricated a hydrogel based on methoxy poly(ethylene glycol)-poly(r-ethyl-Lglutama-te)(mPEG-b-PELG) polymer co-loaded with CA4P and cisplatin(CDDP)and achieved prolonged release of both CA4P and CDDP.More importantly,the combination of hydrogels with dispersed drug-loaded nanoparticles not only enhances intratumoral drug retention but also achieves moderate drug delivery,thus producing an excellent tumor-suppressing effect.Various nanoparticles can be embedded in hydrogels for local injection.
All the experiments were performed at least in triplicates and the data are presented as±.Student's-test was used for comparisons between two groups,and One-way Analysis of Variance (ANOVA) was performed for comparisons of more than two groups.A probability value () of less than 0.05 was considered to indicate a statistically significant difference.
Compared with spherical nanoparticles,the nanoparticles with non-spherical shapes (nanorods and filamentous or worm-like micelles) can be more easily captured by tumor extracellular matrix (ECM) and the perivascular space close to leaky blood vessels to increase drug accumulation at the intermediate sites.To achieve maximum drug retention at the tumor site,we fabricated a doxorubicin hydrochloride (DOX)-loaded staple electrospun fiber with a length of 4 μm and dispersed the fibers in amphiphilic poly (D,L-lactideco-glycolide)-b-poly(ethylene-glycol)-b-poly (D,L-lactide-co-glycolide) (PLGA-PEG-PLGA) tri-block polymer solution to obtain a CA4P-loaded gel/CA4Ploaded staple fiber composite.This mixture can transform into hydrogel after intratumoral injection and achieve sustained release of CA4P and DOX.CA4P released from the hydrogel first shut down the blood vessels of the tumor,and the subsequently released DOX from the staple fibers can gain access into the interior of the tumor,thus increasing the drug enrichment in the tumor cells and induce cell apoptosis.
METHODS
Materials and reagents
PLGA-PEG-PLGA tri-block copolymer (relative molecular mass of 5250,1800-1500-1800,LA∶GA=3∶1)was purchased from Jinan Daigang Biomaterial Co.Ltd(Jinan,Shandong).Copolymer poly(ethylene glycol)-polylactide (PELA,Mw=42 300,Mw/Mn=1.23) containing 10% poly(ethylene glycol) (PEG) was synthesized as described previously.Doxorubicin hydrochloride(DOX · HCl) and CA4P were purchased from Dalian Meilun Biotech Co.Ltd (Dalian,China).Cell Counting Kit-8 reagent (CCK-8) was purchased from Dojindo Laboratories(Japan).Ki67 cell proliferation detection kit(KGA321) and one-step TUNEL cell apoptosis detection kit (KGA7062) were purchased from Jiangsu KeyGen BioTECH Co.Ltd (Nanjing,China).All the other chemicals used in this study were of analytical grade and provided by Chengdu Kelong Chemical Reagent Factory(Chengdu,China).
That afternoon, I went to a local sporting goods store and bought an assortment9 of wrestling headgear and shoes and sent them anonymously10 to the inner-city church.
Preparation of DOX-loaded PELA staple fibers
DOX·HCl was dechlorinated with triethylamine before electrospinning.DOX-loaded PELA staple fibers were prepared by electro-spinning combined with cryo-cutting as described previously.Briefly,30 mg DOX solution in 200 μL DMSO was added into 1g PELA solution in chloroform to obtain a 15% PELA solution by gently stirring the mixture using a magnetic stirrer (FlatSpin,Shanghai Shibin Electronic Technology Co.Ltd).For electrospinning,the polymer solution containing DOX was transferred to a 5 mL syringe fixed on a microinjection pump (Zhejiang University Medical Instrument Co.,Hangzhou,China) with the flow rate set at 0.15 mL/h.The fibers were collected on a piece of aluminum foil wrapped on a grounded rotating mandrel.After vacuum drying for 48 h,the fibrous mats were collected and folded perpendicularly to fiber alignment and frozen rapidly in liquid nitrogen.The frozen fibers were sectioned immediately using a cryostat microtome(LEICA1860,Leica Biosystems,Germany) at-20 ℃at the thickness of 5 μm to obtain DOX-loaded staple fibers(F).The fibers were then washed for 3 times with double distilled water and freeze-dried.The blank fibers(BF)were prepared following the same procedure.
Preparation of drug-loaded hydrogel/staple fiber composite
release of CA4P and DOX from the composite was characterized by incubating a dialysis bag containing 2 mL of G/Fcomposite in a 50-mL centrifuge tube in a water bath at 37 ℃until hydrogel formation.After that,40 mL of PBS was added into each tube and all the samples were shaken at 100 r/min.At predetermined time points,1 mL of the release liquid was withdrawn,and 1 mL of fresh PBS was added in the tube for further incubation.The amount of CA4P and DOX release was measured using an ultraviolet spectrophotometer [UV-5800 (PC),Chengdu Century Ark Technology Co.,Ltd]and a fluorospectrophotometer,respectively.
In prison, holidays are the worst. Birthdays, anniversaries, Thanksgiving, Christmas, even Valentine s Day can be a bummer. It s difficult and painful to be away from those we love-to be left out of the celebrations and the memory making. Many times, we feel a little forgotten or overlooked.
In the Cupid and Psyche tale as recorded by Apuleius, Psyche is pregnant throughout her search for the missing Cupid. The baby, named Pleasure, is born after she is reunited with Cupid. Later versions of the tale, such as the one by Thomas Bulfinch, omit this detail.
Characterization of the composite
The thermo-sensitivity of this composite was determined using the test tube inverting method.Briefly,20 mg of Ffibers were dispersed into 25 mL of aqueous solution containing both CA4P and PLGA-PEG-PLGA polymer,and the mixture was incubated at 37 ℃for 15 min.The specimen was considered to form a gel until no visible flow was observed,and photographs before and after solidification were taken with a digital camera.
In vitro thermo-sensitivity test of the composite
We measured the length of the staple fibers on optical microscopic images (×400 magnification) and calculated the average value using an e-ruler.The length distribution was determined by calculating the ratios of the staple fibers with different lengths in every 100 staple fibers in 5 different areas on inverted phase-contrast microscopic images (Olympus CK40,Japan).The distribution of DOX in Fwas observed using a fluorescence microscope (Olympus IX71,Japan).The encapsulation efficiency and loading amount of Fwere determined using a fluorospectrophotometer (Hitachi F-7000,Japan).
I understood that. I had to go on. But the prospect14 of hairpin15 turns and sheer drop-offs made it impossible for me to eat any supper. Mac tried to keep the conversation breezy, but it didn t help. I excused myself early and went to bed, exhausted16.。。U。,。,,。
In vitro drug release from GCA4P/FDOX composite
To fabricate the hydrogel/staple fiber composite,we first prepared CA4P-loaded hydrogel.Briefly,CA4P (15 mg)and PLGA-PEG-PLGA(100 mg)were dispersed together in 5 mL of PBS under continuous stirring at 25 ℃until a clear solution was obtained(G).Ffibers(20 mg)were then dispersed into 25 mL of Gsolution to prepare the drug-loaded hydrogel/staple fiber composite with a theoretical CA4P to DOX ratio of 5∶1(m/m).To facilitate homogeneous dispersion of the staple fibers in PLGA-PEG-PLGA copolymer solution,2% sodium alginate was added.After ultra-sonication for 10 min,the hydrogel/staple fiber composite loaded with both CA4P and DOX (G/F) was obtained and stored at 4 ℃for later use.
In vitro cytotoxicity test
We used a female Balb/c mouse model bearing subcutaneous mouse breast cancer 4T1 cell xenograft to investigate the antitumor effect of G/Fcomposite.At 7 days after tumor cell inoculation,the tumors reached a volume of~50 mm.The tumor-bearing mice were randomly divided into 3 groups (=8 per group) for intratumoral injections of 200 μL of normal saline,F,or G/F.The doses of CA4P and DOX were equivalent to 20.0 and 4.0 mg/kg,respectively.The tumor volume was calculated by measuring the length and width of tumors with a Vernier caliper,and the body weight was also monitored for 30 days.On day 14,the tumors were dissected and fixed in 10% neutral formaldehyde,and then embedded in paraffin blocks and sectioned at a thickness of 4 μm.The obtained tissue sections were stained with hematoxylin and eosin (HE).To investigate the proliferation and apoptosis of the tumor cells,immunohistochemistry (IHC) for Ki-67 and tetramethylrhodamine (TRITC)-labeled terminal deoxynucleotidyl transferase dUTP nick end labeling(TUNEL) were performed following the manufacturer's instructions,and the images of HE staining and IHC were obtained with a light microscope (Nikon Eclipse E400,Japan),and TUNEL staining was observed using a fluorescence microscope.The rates of cell proliferation and apoptosis were calculated using Image J software.
Assessment of in vivo gel formation
All animal experiments were carried out in accordance with the Guide for the Care and the Use of Laboratory Animals as promulgated by the National Institute of Health.Three male Balb/c mice(6-8 weeks old,18-22 g)were used forgel formation test of the composite.The hair on the right back of each mouse was removed with 10% NaS before subcutaneous injection of 100 μL of PBS,For G/Fsuspensions,and at 12 and 24 h after the injection,the volume of the pimple at the injection site was qualitatively monitored and photographed with a digital camera.
Assessment of in vivo antitumor effect of the composite
We testedcytotoxicity of G/Fcomposite using Cell Counting Kit-8 (CCK-8) reagent in human breast cancer MCF-7 cells and mouse breast cancer 4T1 cells,provided by the Cell Bank of Chinese Academy of Sciences (Shanghai,China) and maintained in our laboratory.Briefly,the cells in logarithmic growth phase were seeded in 48-well plates at a density of 1×10cells per well.After incubation for 24 h to allow cell attachment,the sterilized samples of G/F,F,blank hydrogel (BG) and blank fiber (BF) were added in the wells.The doses of CA4P and DOX in G/Fwas equivalent to 5.0 μmol/L and 1.0 μmol/L,respectively.The cells without any treatment were used as the control.After the cells were incubated with the samples for 24,48 and 72 h,the medium and samples were carefully removed.The cells in each well were washed for 3 times with PBS and then incubated with 300 μL of fresh RPMI 1640 culture medium and 30 μL of CCK-8 reagent,with 300 μL of fresh RPMI 1640 containing 30 μL of CCK-8 reagent but without cells as the blank control.After 4 h of incubation,100 μL of incubation solution was pipetted from each well and transferred into a new 96-well plate for measurement.The absorbance at 450 nm of each well was determined using an automated microplate spectrophotometer (Multiskan GO1510,Thermo Fisher Scienticic Co.,Ltd.USA.)and the relatively cell viability was calculated.
Statistics analysis
I fell in love with the minister s son the winter I turned fourteen. He was not Chinese, but as white as Mary in the manger. For Christmas I prayed for this blond-haired boy, Robert, and a slim new American nose. When I found out that my parents had invited the minister s family over for Christmas Eve dinner, I cried. What would Robert think of our shabby Chinese Christmas? What would he think of our noisy Chinese relatives who lacked proper American manners? What terrible disappointment would he feel upon seeing not a roasted turkey and sweet potatoes but Chinese food?
RESULTS AND DISCUSSION
Characterizations of hydrogel/staple fiber composite
The administration schedule was an important factor in combined therapy with VDAs and other chemotherapeutic drugs.Studies suggested that the administration of VDAs prior to chemotherapeutics caused a delay of the latter to reach the tumor 'core',and the effects of the additional chemotherapeutic could be further potentiated through VDAs-mediated 'trapping' of the drug within the tumor.As an excellent thermo-sensitive material,PLGA-PEG-PLGA tri-block copolymer is often used to carry hydrophilic and hydrophobic chemotherapeutic agent for local cancer therapy.
PLGA-PEG-PLGA solution is in a sol state at room temperature and transforms into a water insoluble gel at body temperature due to the hydrophobic interaction between PEG chains at 37 ℃.As shown in Fig.1C,at room temperature,the staple fibers were well dispersed in PLGA-PEG-PLGA polymer solution containing CA4P,which could flow easily.However,when the temperature increased to 37 ℃,the dispersions became solidified and formed hydrogel,and could not flow.These results indicate that the addition of Ffibers had no significant effect on the thermo-sensitivity of G,and the G/Fcomposite could be used as a potential injectable formulation for local tumor therapy.
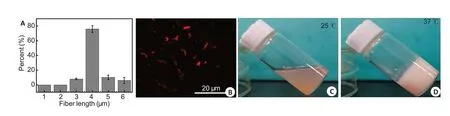
In vitro release of CA4P and DOX
As shown in Fig.1A,the length of Fwas mainly distributed between 3 μm and 5 μm,and the fibers 4 μm in length accounts for 76%;the average length of Fwas 4.0±1.3 μm.Due to the spontaneous fluorescence characteristic of DOX,we observed the drug distribution with a fluorescence microscope.Fig.1B shows no apparent aggregation of the staple fibers,and DOX is homogeneously distributed on the fibers.To ensure the good antitumor efficacy of the fibers,we tested the loading amount and the encapsulation efficiency of DOX.The loading amount of DOX was(2.69±0.35)%and the encapsulation efficiency was (89.70±0.12)% in F.There was about 10%of drug loss,possibly as a result of a small amount of drug release from the fiber surface when soaking the fiber in water during the cryo-cutting process.
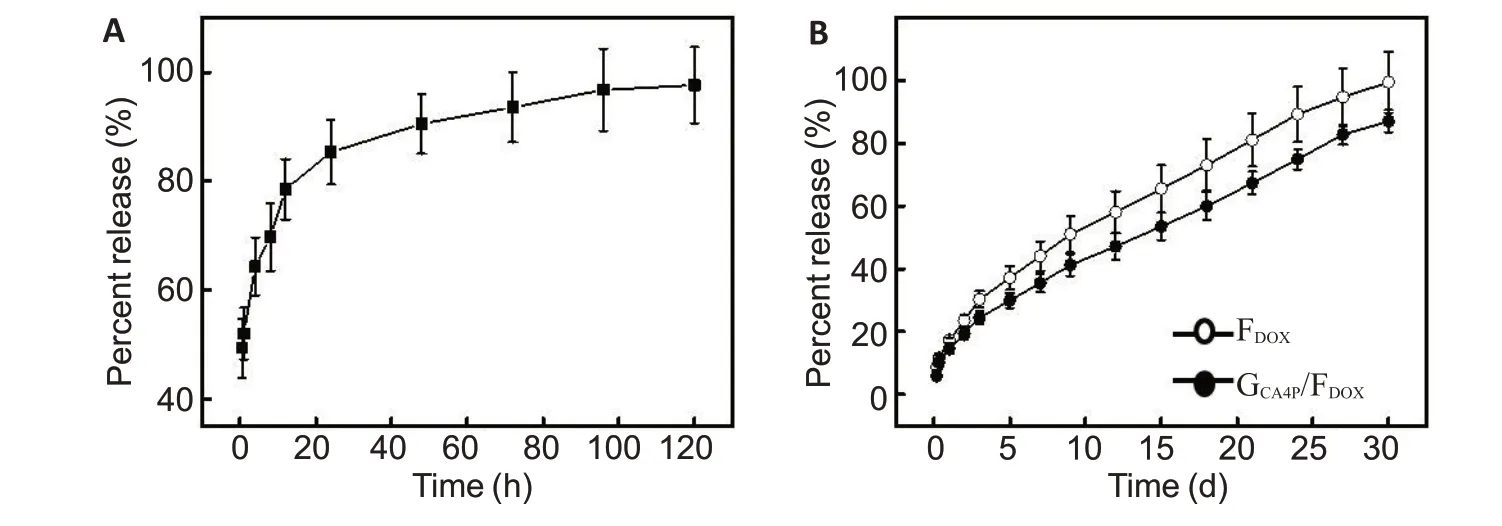
As shown in Fig.2A,an early burst release followed by sustained release of CA4P occurred when incubating G/Fin PBS at 37 ℃.Approximately 64.3%of CA4P was released from the composite within 4 h,and almost complete CA4P release occurred in 5 days.This can be attributed to the fact that CA4P has a high water solubility and its release from PLGA-PEG-PLGA mainly depends on the diffusion-controlled process.However,the release profile of DOX was different from that of CA4P,and no obvious burst release of DOX was detected within 24 h,approximately 87% of DOX was released from G/Fwithin 30 days.The release mechanism of DOX not only depends on drug diffusion but also on the degradation of the composite matrix,thus resulting in a slower release rate of DOX from the G/Fcomposite than from F(Fig.2B).
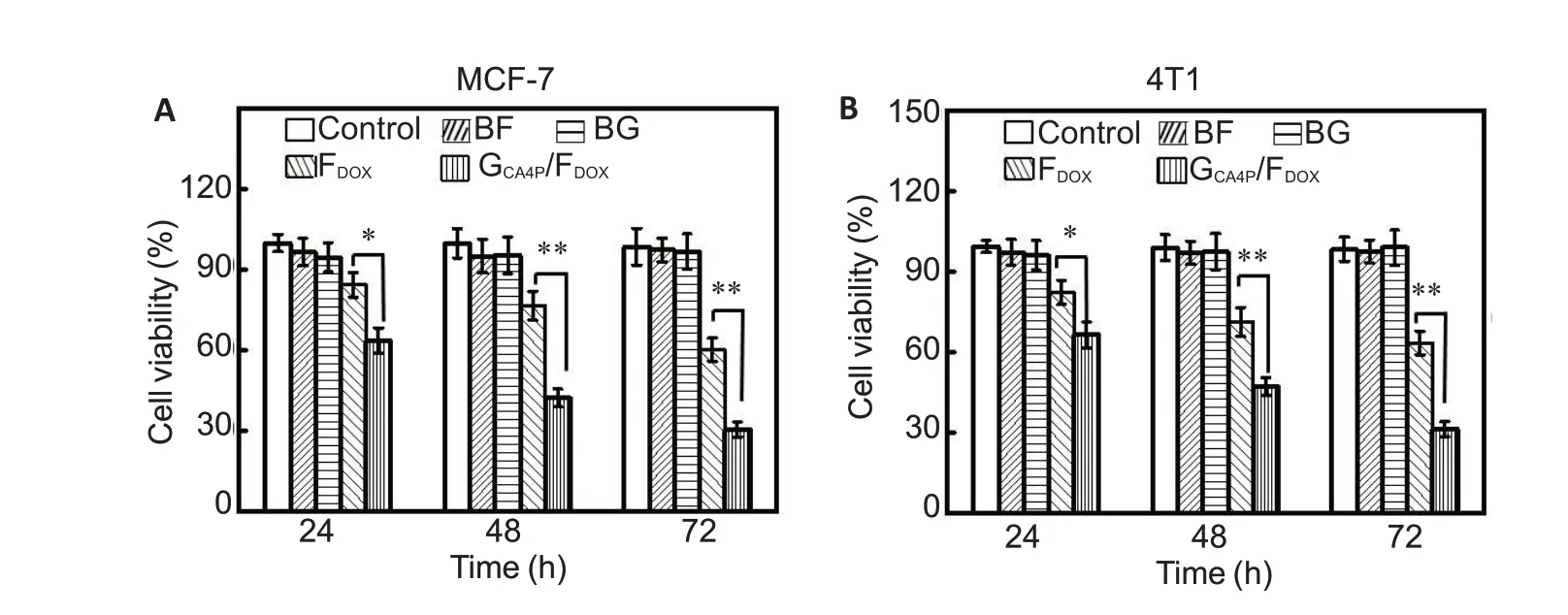
In vitro cytotoxicity of GCA4P/FDOX
As a water-soluble prodrug,CA4P can rapidly metabolize into combretastatin A4 (CA4).We previously found that CA4-loaded fibers could improve the antitumor efficacy of chemotherapeutic drugs by inhibiting tube formation of vascular endothelial cells.Here we examined the cytotoxicity of the G/Fcomposite using CCK-8 assay.As shown in Fig.3,both MCF-7 cells(Fig.3A) and 4T1 cells (Fig.3B) showed no significant reduction of cell viability in the presence of BG or BF even at 72 h,but the cell viability decreased progressively after incubation with G/Fand Ffor 24,48,and 72 h.Due to the sustained release of CA4P and DOX,only 30.6%of MCF-7 cells and 28.9%of 4T1 cells still remained viable after incubation with G/Ffor 72 h,and these rates were higher than those of cells incubated with F.These results demonstrate an strong tumor inhibition efficacy of G/Fcomposite.
In vivo thermo-sensitivity of GCA4P/FDOX composite
In PLGA-PEG-PLGA hydrogel,a proportion of the hydrophobic and hydrophilic groups interact as the temperature changes.Under the lower critical temperature (LCST),the gel swells in aqueous solution,but once the temperature rises to the LCST,the gel shrinks with volume changes.Fig.4 shows that after subcutaneous injection 100 μL of G/Fsuspension,gel formationoccurred due to the body temperature of the mice,and the volume of the formed gel at the subcutaneous layer was smaller than that of saline and F.Even at 24 h,no apparent change of the gel volume was observed due to the slow degradation of PLGA-PEG-PLGA polymer.

Tumor growth inhibition and body weight change
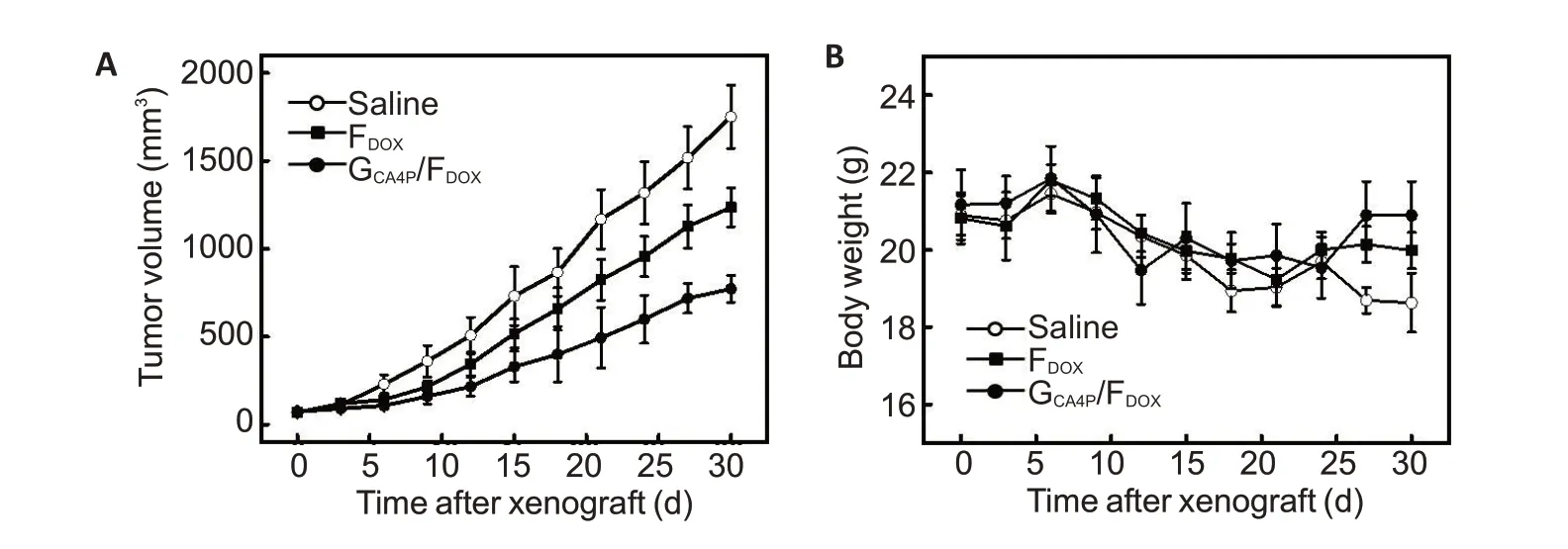
CA4P is one of the most potent VDAs,which can specifically block the existing blood vessels of the tumor and causes necrosis of the tumor tissue.We assessed the antitumor efficacy of intratumoral injection of G/Fcomposite in a mouse model bearing subcutaneous 4T1 cell xenograft.Fig.5 shows the changes in tumor volume and body weight of the mice after intratumoral injection of G/Fand F.Compared with those in saline treatment group,tumors in G/Fand Ftreatment groups grew more slowly.At 30 days,the tumor volume in G/Ftreatment group reached 771.9±76.9 mm,significantly smaller than that in Fand saline treatment groups(1235.7±111.2 mmand 1751.0±179.4 mm,respectively;Fig.5A).To investigate the adverse effect of local injection of G/Fand F,we monitored body weight changes of the mice within 30 days after the treatments.As shown in Fig.5B,all the tumor-bearing mice showed weight loss after modeling,and a roughly 10% weight loss was observed in the treatment groups.
Histological,immunochemical and immunofluorescence evaluation
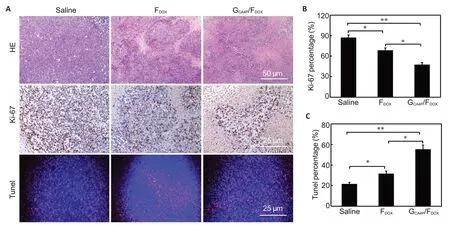
To further evaluate the antitumor efficacy of G/F,we examined the tumor tissues using HE staining,IHC staining and immunofluorescence assay on day 21 after the treatments.HE staining (Fig.6A) showed more obvious necrosis in the tumors after treatments with Fand G/Fthan after saline treatment.G/Ftreatment resulted in the largest necrotic area(pink area)along with vacuolar degeneration of the tumor cells.IHC staining and TUNEL assay showed the lowest positivity for Ki-67 and the most apoptosis cells(red fluorescence)in the tumor in G/Ftreatment group (Fig.6B and 6C).Compared with other treatment,G/Ftreatment resulted in a cell proliferation rate of(47.2±3.2)%in the tumor cells,significantly lower than those in saline group[(85.4±6.1)%,<0.01]and Ftreatment group[(68.5±4.1)%,<0.05].G/Ftreatment also caused an apoptosis rate of(54.4±3.9)%in the tumor cells,the highest among the 3 groups.These results demonstrate that G/Fhas the strongest ability to inhibit proliferation and induce apoptosis of the tumor cells after local injection in the tumor-bearing mice.
One evening, with the help of the night clerk at our quaint1 hotel, we found a tiny cafe known only to locals. Nestled inside a dark passage, its unlit sign read, Chez Maurice. We peeked2 in the small window on the door to see a small room with half a dozen tables, each with enough chairs for eight patrons. We opened the heavy door and went inside.
Conclusion
We prepared an injectable hydrogel/staple fiber composite by physically mixing CA4P-loaded PLGA-PEG-PLGA hydrogel with DOX-loaded staple fibers.This dual drug delivery system is thermo-sensitive and can solidify at 37 ℃to achieve sustained release of CA4P and DOX and enhanced cytotoxicity.After subcutaneous injection in mice,the composite can quickly forms gels.Compared with F,local injection of G/Fcomposite results in a stronger antitumor efficacy,suggesting its potential as a dual drug delivery system for local chemotherapy of solid tumors.