Coexistence of situs inversus totalis and hepatocellular carcinoma: A series of nine cases and a literature review
Xiaowei Li, Zhigang Fu, Jiaming Zhong, Kunkun Cao, Xiaoxia Chen, Ning Ding, Li Liu,Jian Zhai, Zengqiang Qu
Department II of Interventional Radiology, Eastern Hepatobiliary Surgery Hospital, Shanghai, China
Keywords:Situs inversus totalis Hepatocellular carcinoma Treatment strategies
ABSTRACT Hepatocellular carcinoma (HCC) is the most commonly diagnosed carcinoma and one of the leading causes of cancer-related deaths worldwide.Situs inversus totalis(SIT)is a congenital condition where in the internal organs of the abdomen and thorax lie in mirror images of their normal position. Thus far, there are very few reports on cases of SIT coexisting with HCC. Our case series is probably the largest series in world literature. The cohort of this retrospective study included a total of nine patients diagnosed with SIT-HCC and treated in our hospital between January 2013 and May 2018. Clinical characteristics, prognostic factors, and outcomes were summarized. Treatment strategies included surgery, transarterial chemoembolization, and microwave ablation. The diagnosis and treatment of patients with SIT are challenging because of organ reversion. The current treatment strategies for different stages of liver cancer are safe and feasible for patients with SIT-HCC.
1. Introduction
Hepatocellular carcinoma (HCC) is the fourth most common cancer and the second most frequent cause of cancer-related deaths in China.1HCC typically develops in the background of chronic liver disease due to hepatitis B virus (HBV) infection, hepatitis C virus infection, alcohol abuse, and/or nonalcoholic fatty liver disease.2Chronic hepatitis is the major cause of primary liver cancer in China. Although considerable progress has been made in characterizing the genetic basis of HCC, its pathogenesis remains unclear.Situs inversus totalis(SIT)is an extremely rare congenital condition characterized by reversion or mirroring of the internal organs from their usual positions,with an incidence of one case per 5,000 to 10,000 persons.3There have been very few cases of SIT coexisting with HCC.Clinically,it is important for physicians to arrive at a diagnosis based on the relevant anatomical positions of the organs.Recognition of any situs anomaly is necessary to avoid misdiagnosis and unwanted consequences.4
Nine patients with HCC and SIT were admitted to our hospital between January 2013 and May 2018. The clinical characteristics, prognostic factors,and outcomes are discussed below.
2. Cases report
This case series was approved by the Ethics Committee of the Eastern Hepatobiliary Surgery Hospital of Naval Medical University (Shanghai,China).The requirement for informed consent was waived because of the retrospective design of the study.
The cohort of this retrospective study included a total of nine patients(eight men and one woman; mean age, 59.7 ± 9.1 years; age range,43-74 years) diagnosed with SIT-HCC and treated in our hospital between January 2013 and May 2018.A male patient with well-controlled HCC died of congenital heart disease. Two patients reported constant pain in the upper-left quadrant without induction, while HCC was detected in the other seven patients by B-ultrasound during physical examination.In the two patients who reported tenderness on the left side of the upper abdomen, a hard mass was palpable below the left costal margin and the range of activity was poor.The liver texture was slightly hard with non-smooth surfaces in patients with liver cirrhosis. None of the patients had jaundice or ascites.Electrocardiography indicated right axis deviation with a P-wave axis of >90,and chest radiography revealed dextrocardia. Abdominal ultrasonography revealed situs inversus, with the liver on the left side. Abdominal dynamic contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI)showed that the stomach and spleen were on the right side and the liver on the left side(Fig.1).The liver tumor showed typical characteristics of“rapid wash in and out” but no vascular anomalies or extrahepatic spread. Of the nine patients, eight (88.9%) tested positive for the HBV surface antigen. According to the Barcelona Clinic Liver Cancer staging criteria,there were seven cases of stage A and two cases of stage B.The Eastern Cooperative Oncology Group-Performance Status of the patient with complex congenital heart disease was 1 and that of the other eight cases was 0. The basic characteristics of the patients are summarized in Table 1.
Laboratory data were collected, including information on alphafetoprotein, albumin, total bilirubin, alanine aminotransferase, plasma prothrombin coagulation time, creatinine, serum HBV DNA levels and complete blood cell counts.Imaging data included the size and number of lesions,vascular invasion,and extrahepatic metastasis(Table 2).All nine patients were diagnosed with both SIT and HCC. The other diagnoses included HBV infection and liver cirrhosis. One patient was also diagnosed with complex congenital heart disease.
All patients received adequate treatment after a detailed clinical evaluation.Finally,five patients met the surgical criteria and underwent right hepatectomy in the reverse position.One patient was complicated with pleural effusion was discharged with active treatment. Microwave ablation(MWA)was used in two cases of postoperative recurrence and in two cases as the initial treatment. All nine patients underwent transcatheter arterial chemoembolization (TACE), including those with recurrence and complex congenital heart disease. A total of 14 TACE procedures were performed. There were no complications associated with MWA and TACE.
All nine patients were followed up for a median duration of 25.0 months. Only three patients survived as of January 1, 2020, (Table 1),and the 1-, 2-, 3-, and 5-year survival rates were 100%, 55%, 33%, and 22%, respectively. The patient with complex congenital heart disease eventually died of a heart attack.
3. Discussion
SIT is a rare congenital syndrome in which the thoracic and abdominal organs are reversed or mirrored from their normal position. To the best of our knowledge, the exact cause of SIT remains inconclusive but may be related to family genetics, changes in chromosome structure or number, and/or gene mutations.5Guo et al. reported four cases of primary ciliary dyskinesia with DNAAF3 mutations and SIT.6The absence of Cerberus-like 2 (Cerl2), an inhibitor of Nodal, and zinc fingers in cerebellum 3(ZIC3)missense mutations,results in malformations commonly known as heterotaxy syndrome,including SIT,which is characterized by mirror images of usually asymmetric paired organs and reversed orientation of at least one organ.7,8An embryologic and genetic study conducted by Bartram et al. reported that SIT results from disruption of the process of normal left-right axis specification during embryogenesis.9
Therefore, attention should be paid to comorbid diseases in patients with SIT-HCC. SITs can occur in isolation or in conjunction with other diseases.10In another study of 155 children with SIT,the most common comorbid diseases were congenital heart defects (CHDs) (46.5%) and primary ciliary dyskinesia (12.3%).11During physical examination,mirror-image dextrocardia is diagnosed as a deviation from the normal position of the heart.Early cardiac MRI aids in accurately diagnosing and monitoring heart defects.Information derived from cardiac MRI is useful for improving the quality of life of patients with SIT-HCC and CHD.12Pan et al. reported a case of previously unrecognized SIT in a patient with left-upper quadrant pain that was diagnosed as acute myocardial infarction. However, massive bleeding from a previously undiagnosed hepatic lesion resulted in the death of the patient during treatment.4Among our patients, one with congenital heart disease affected the choice of follow-up treatment for hepatomas, and the patient was deemed unsuitable for radical surgery. Finally, TACE was performed.Therefore, for patients with SIT-HCC, more attention should be paid to coexisting diseases such as CHD, primary ciliary dyskinesia, renal disorders,biliary atresia,and skeletal dysplasia.
4. SIT-HCC
In 1983, Kanematsu reported the first case of SIT with HCC in a patient who was successfully treated with right hepatectomy. The patient died of recurrence 18 months after the surgery.13A literature search in the PubMed and Google Scholar databases resulted in only 20 cases of SIT-HCC previously reported in the English literature.Our case series is probably the largest series in world literature.
The two patients with left-upper quadrant pain in the present series were misdiagnosed with “stomach disease,” although the clinical symptoms, signs, and location were exactly contrary to those seen in the normal positions.There is a high chance of misdiagnosing SIT,which can result in accidental injury during surgery. Therefore, special attention should be paid to the physical and imaging examinations. Seven of our patients had no obvious symptoms,possibly due to early tumor detection,although a high percentage of cases were positive for HBV.
HBV infection is a major cause of chronic hepatitis,liver cirrhosis,and HCC in China. Patients with SIT and hepatitis B are at a particularly increased risk of HCC,especially in men aged >40 years.Early screening of the liver by ultrasonography and serum alpha-fetoprotein levels facilitates early diagnosis of HCC and is recommended every 6 months for high-risk patients.14
HCC is a major cause of cancer-related mortality. Several therapies are available for HCC, and the therapy type is determined based on the patient's clinical status and liver function.Radical treatment options for early-stage HCC include surgical resection, liver transplantation, and radiofrequency ablation or microwave ablation. The treatment options for advanced HCC include TACE, systemic therapy, and moleculartargeted agents.15
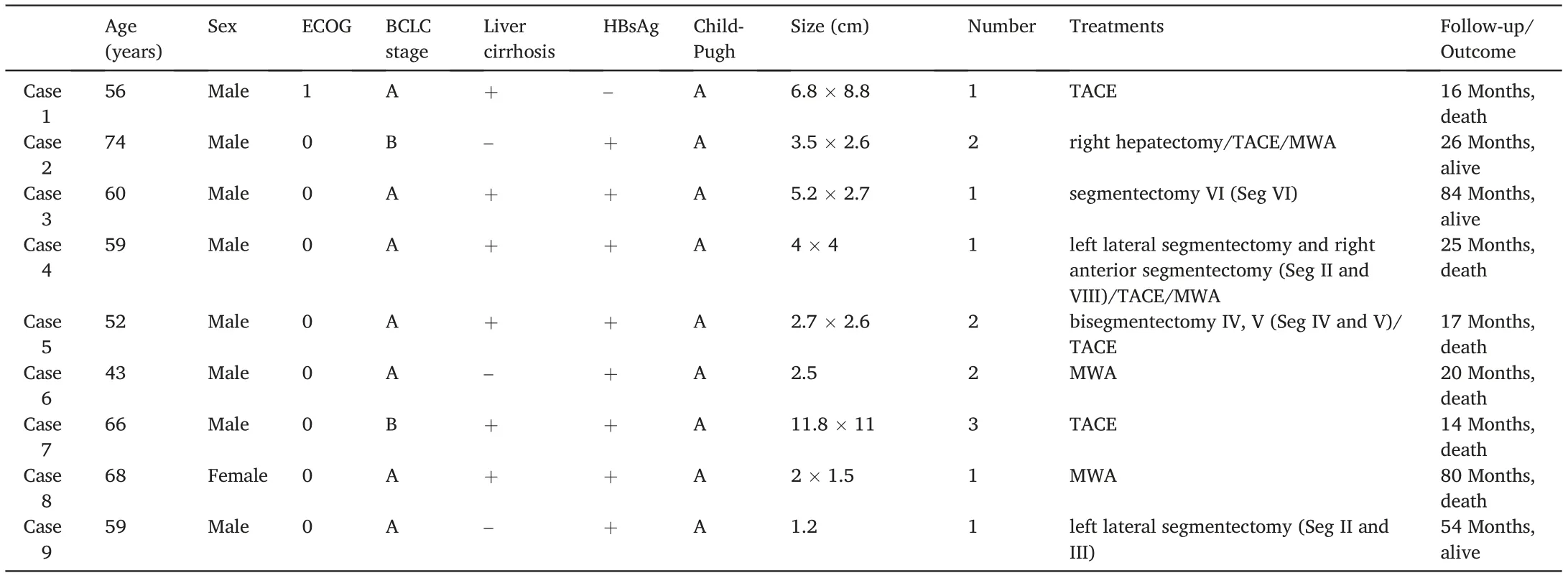
Table 1 Clinical characteristics.
For the 20 SIT-HCC cases reported in the literature, treatments included surgery, TACE, and MWA. Of these previous reports and the nine cases assessed in the present report,16 patients underwent surgery to remove malignant hepatic tumors.For patients with SIT-HCC,surgery is associated with particular complications because the anatomy is completely contrary and there is a possibility of associated vascular and hepatobiliary abnormalities. Hence, more thorough anatomical and functional assessments will allow for better surgical selection. Surgical options for HCC include the liver-hanging maneuver and Glissonean pedicle transection,16right hemihepatectomy through the anterior approach,17right hepatectomy,18left hepatic segmentectomy, hepatic trisegmentectomy,lower posterior segmentectomy,partial hepatectomy of segment VII, partial hepatectomy of segment II,3pure laparoscopic right hepatectomy,19liver resection with concomitant splenectomy,20and hepatectomy with reference to computer-generated mirror images.21Among the cases in the present series, the treatments included right hepatectomy,left lateral segmentectomy(segments II and III),left lateral segmentectomy with right anterior segmentectomy (segments II and VIII), bisegmentectomy (segments IV and V), and segmentectomy(segment VI).All these options of hepatic surgery are feasible in patients with SIT-HCC.3
Owing to the unusual mirror-image anatomy,MWA in a patient with SIT-HCC can be technically challenging. Details on the minimally invasive treatment of liver cancer in patients with SIT,including MWA,have seldom been published. In the present series, four patients underwent WMA: two with postoperative recurrence and two with the initial treatment. Considering the contrasting anatomy, the patient was positioned with the left side facing up.As in laparoscopic right hepatectomy in an SIT patient,19the position of the ultrasound system and that of the surgeons is an important consideration.In these cases,the operator stood on the right side of the patient, and the assistant and the ultrasound system were placed on the left side. The operator could reverse the ultrasonic probe,which was helpful for the surgeon to place the puncture needle at the center of the tumor during surgery. Puncture points for thermal ablation were inserted from the intercostal space on the left sideof the patient. The surgery was conducted gently and slowly to avoid damage to the adjacent organs.MWA is a feasible procedure for SIT-HCC when performed by an experienced surgeon.
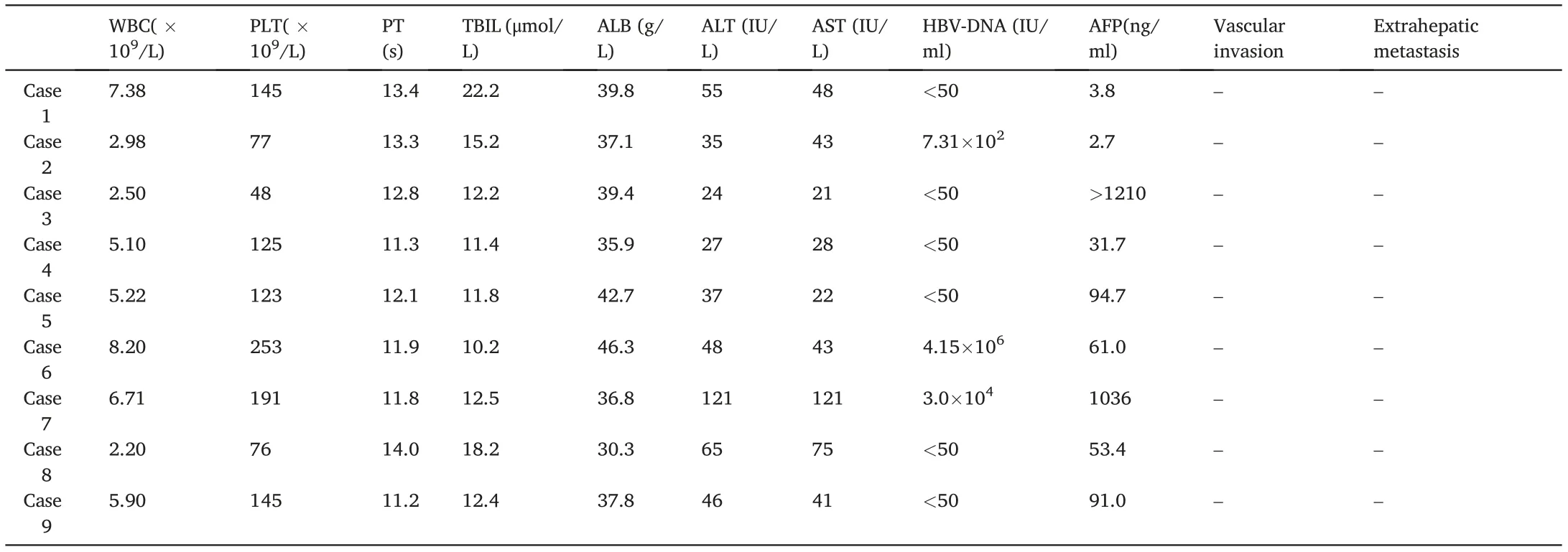
Table 2 Laboratory and imaging data.
Transarterial chemoembolization was performed in all nine cases,including those with recurrence and complex congenital heart disease.The TACE procedure for SIT-HCC patients was not significantly different from normal patients. The catheter can be rotated slightly to the left during celiac trunk angiography,which is conducive for full visualization of the feeding artery of the tumor. Therefore, microcatheters are recommended for superselection. TACE can be performed in patients with SIT-HCC who have complicated congenital diseases and are otherwise unfit for surgery.
5. Conclusions
In this report,we summarized nine cases of SIT-HCC and reviewed 11 other cases.The diagnosis and treatment of SIT are challenging because of the mirror images of the organs. Current treatment strategies for different stages of liver cancer are indicated for patients with a“normal”anatomy and a mirror-image anatomy. Although surgery and MWA for SIT-HCC patients are technically challenging owing to visceral inversion,these techniques are feasible as long as the positions of the operator and equipment could be changed. During TACE, the catheter can be rotated slightly to the left during celiac trunk angiography. TACE is used to reduce tumor bulk,improve survival,and palliate symptoms in patients with unresectable HCC or who are unfit for surgery.
Author contributions
Jian Zhai,Zengqiang Qu:Conceptualization,Methodology,Software.Xiaowei Li: Data curation, Writing-Original draft preparation. Zhigang Fu, Jiaming Zhong, Xiaoxia Chen: Visualization, Investigation. Zengqiang Qu: Supervision. Kunkun Cao, Ning Ding: Software, Validation.Xiaowei Li, Li Liu:Writing-Reviewing and Editing.
Declaration of competing interest
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
 Journal of Interventional Medicine2022年1期
Journal of Interventional Medicine2022年1期
- Journal of Interventional Medicine的其它文章
- Safety and efficacy of Endovascular Management of high-grade blunt renal injury
- Molecular targeted therapy causes hepatic encephalopathy in patients after Transjugular intrahepatic portosystemic shunt (TIPS): A case report and literature review
- A low-grade cerebral arteriovenous malformation suspected of being a metastatic tumor: A case report and literature review
- Angiography findings and endovascular management of acute nonvariceal gastrointestinal bleeding: A pictorial essay
- Comparison of tumor response following conventional versus drug-eluting bead transarterial chemoembolization in early- and very early-stage hepatocellular carcinoma
- Complications from port-a-cath system implantation in adults with malignant tumors: A 10-year single-center retrospective study
