Update on the applications and limitations of alpha-fetoprotein for hepatocellular carcinoma
Hira Hanif,Mukarram Jamat Ali,Ammu T Susheela,Iman Waheed Khan,Maria Alejandra Luna-Cuadros,Muzammil Muhammad Khan,Daryl Tan-Yeung Lau
Hira Hanif,Mukarram Jamat Ali,lman Waheed Khan,Maria Alejandra Luna-Cuadros,Muzammil Muhammad Khan,Daryl Tan-Yeung Lau,Liver Center,Department of Medicine,Beth Israel Deaconess Medical Center,Harvard Medical School,Boston,MA 02215,United States
Ammu T Susheela,Internal Medicine,Loyola MacNeal Hospital,Berwyn,PA 60402,United States
Abstract Alpha-fetoprotein (AFP) is an oncofetal glycoprotein that has been used as a tumor marker for hepatocellular carcinoma (HCC) in combination with ultrasound and other imaging modalities.Its utility is limited because of both low sensitivity and specificity,and discrepancies among the different methods of measurements.Moreover,its accuracy varies according to patient characteristics and the AFP cut-off values used.Combination of AFP with novel biomarkers such as AFP-L3,Golgi specific membrane protein (GP73) and des-gamma-carboxyprothrombin significantly improved its accuracy in detecting HCC.Increased AFP level could also signify severity of hepatic destruction and subsequent regeneration and is commonly observed in patients with acute and chronic liver conditions and cirrhosis.Hereditary and other non-hepatic disorders can also cause AFP elevation.
Key Words:Alpha-fetoprotein;Hepatocellular carcinoma;Alpha-fetoprotein-L3;Cirrhosis;Tumor markers;Hereditary persistence of alpha-fetoprotein
lNTRODUCTlON
During fetal and neonatal life,alpha-fetoprotein (AFP) is produced by yolk sac,fetal liver and gastrointestinal tract.Only a trace amount of AFP can be measured in adults due to its rapid decline in adults[1-4].The use of AFP as a tumor marker for hepatocellular carcinoma (HCC) was first proposed in 1960s.The utility of AFP as a surveillance and diagnostic test has been criticized due to both low sensitivity and specificity.AFP,however,continues to play a significant role for HCC surveillance in combination with ultrasound (US) and other imaging modalities[5-8].This review focused on both the clinical roles and limitations of AFP.In addition,the patterns of AFP elevation in various non-HCC etiologies were discussed.
BlOLOGY OF AFP
AFP is an oncofetal glycoprotein consisting of a single polypeptide chain of approximately 600 amino acids and nearly 4% carbohydrate.With molecular weight of 67500 dalton,it is a negatively charged protein with an isoelectric point of pH 4.57 and displays several charge isomers by extended agarose gel electrophoresis[1,2].During the first trimester,AFP is mainly produced by yolk sac.After the atresia of yolk sac by 11-12 wk,fetal liver becomes the predominant source of AFP.A trace amount is also produced by the gastrointestinal tract of the fetus[1].AFP in fetal serum can be detected as early as 29 d after conception and reaches its peak value of 3.0 × 106ng/mL by 14thweek of gestation.It declines to 2.0 × 105-3.0 × 105ng/mL by week 32 and further decreases to 20-120 ng/mL at term[3].By six months of life,serum AFP level is approximately 30 ng/mL.Thereafter,it is detectable between 3 and 15 ng/mL in adulthood[3,4].
AFP belongs to the family of serum albumin and the genes of which are present on the chromosome 4.It shares structure and physiochemical properties with its family members namely albumin,vitamin D-binding protein and afamin[9].As both albumin and AFP show significant amino acid homologies,AFP is suggested to be an embryonic analogue of albumin[10].Furthermore,because of its similarity to albumin,it has been postulated that AFP could be a carrier protein.In addition,its role as an immune-regulator and as a carrier protein for bilirubin has also been suggested[11].
AFP,being a principal serum binding protein in the fetus,plays a vital role in carrying various ligands such as fatty acids,hormones,minerals and bilirubin[12].Though it performs many physiological functions during fetal development,elevated levels in adults are frequently observed in liver carcinogenesis and various disease processes[13-15].Many biologic studies support the pro-oncogenic as well as antiapoptotic effects of AFP.AFP can stimulate cell proliferation,cell motility and invasive properties of HCC cell lines and there is evidence that apoptosis of cancer cells could be achieved by blocking AFP[16,17].On the other hand,a number of cancerous and non-cancerous causes involving both the liver and other organs can also lead to AFP elevation.AFP,therefore,is a non-specific marker of HCC[7] (Table 1).
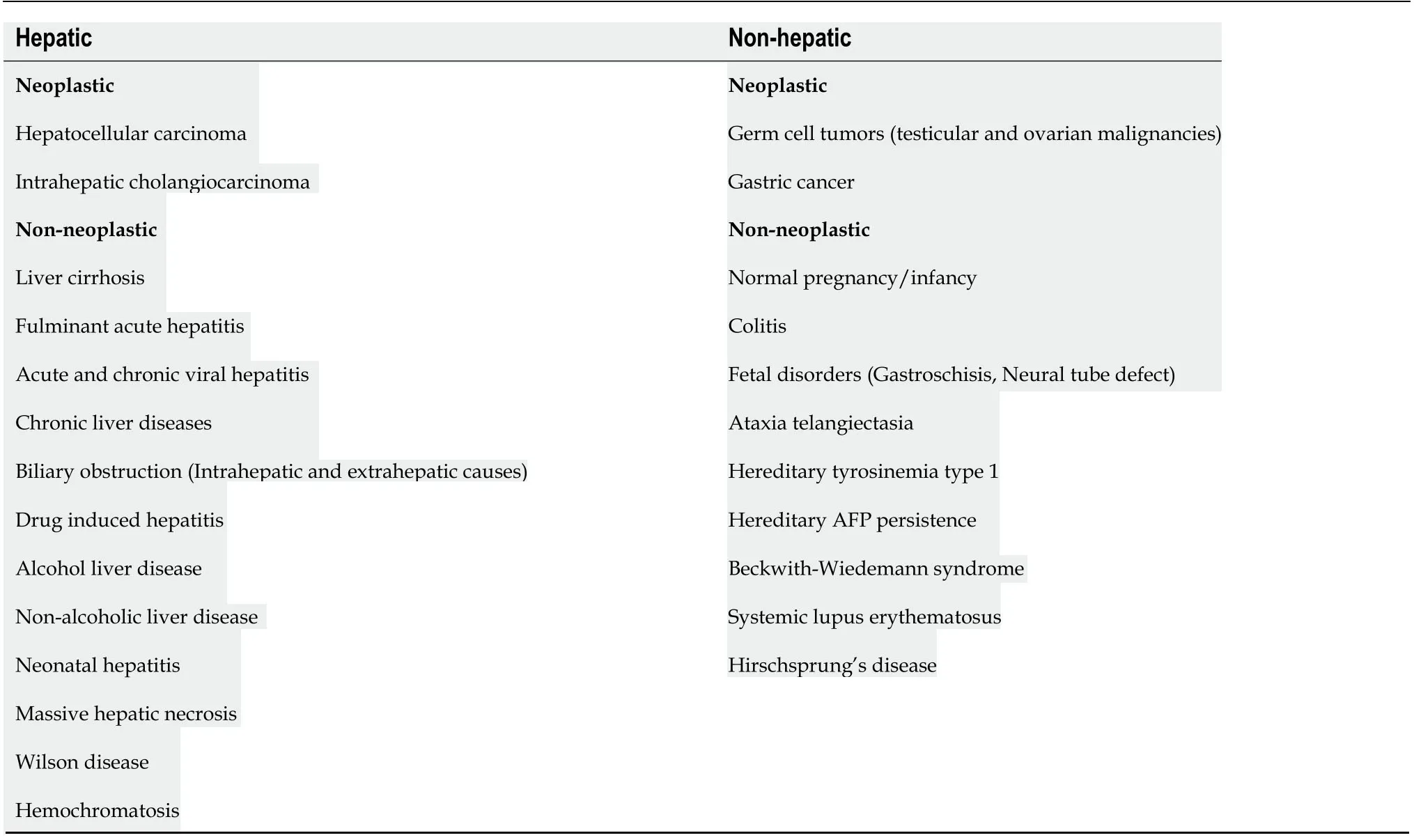
Table 1 Causes of alpha-fetoprotein elevation[13-15]
HOW lS AFP MEASURED?
AFP was originally measured by immunoelectophoresis,but this method was not verysensitive.In the 1970s and 1980s,new techniques such as radioimmunoassay and enzyme immunoassays were used.Subsequently,a quantitative automated chemiluminescent enzyme immunoassay was developed,which replaced and refined the previous clinical assays[18,19].In this method,the serum sample is placed on a magnetic plate which is already bound by an anti-AFP antibody.A second chemiluminescent detection antibody,added to the same magnetic plate,then binds to all the AFP that is present in excess.All the unbound detection antibody is washed off and an organic substrate called as developer is added which emits light and become luminescent (Figure 1A).A chemiluminometer is used to detect the antibody,and quantification of the results is done against the known AFP standards.However,measurement interference may occur.In a single step method of AFP detection,sometimes interfering antibodies would bind to both the capture and detect antibodies leading to a false positive result (Figure 1B).Conversely,the interfering antibodies may blind to the reagents and inhibiting the proper interaction of AFP with the specific anti-AFP antibodies[20] (Figure 1C).

Figure 1 ELlSA measures.A:ELISA measures alpha-fetoprotein (AFP) by detecting reactivity with two anti-AFP antibodies;B:Interfering antibodies that bind directly to the capture and detect reagents without the target AFP (no analytes).This binding would emit light and become luminescent causing false positive results and high values;C:Interfering antibodies can inhibit reactivity of the ELISA by binding to the reagents and prevent the detection of AFP by the anti-AFP antibodies;that leads to a false negative result.AFP:Alpha-fetoprotein.
AFP as a diagnostic marker for HCC
The association between AFP and HCC is well recognized;however,the sensitivity and specificity of the AFP assay varies according to patient characteristics,design of the study,and the AFP cut-off values used[21,22] (Table 2).A systematic review of studies using AFP at a threshold value of 20 ng/mL in patients with cirrhosis,the sensitivity and specificity of detecting HCC were 41%-65% and 80%-94%,respectively[22].Lowering the cut-off can increase the sensitivity of AFP but at the cost of higher false positives.By increasing the AFP value from 20 to 50 ng/mL,the specificity increased to 96% with a positive predictive value of 75% but sensitivity was reduced to 47%[23].AFP values also vary according to the tumor size.The correlation of AFP to the size of the tumor was evaluated by Saffroyet al[24].The bigger tumors generally had higher AFP values.The sensitivity of AFP,therefore,decreased from 52% for HCC> 3 cm to 25% for those < 3 cm in diameter[24].
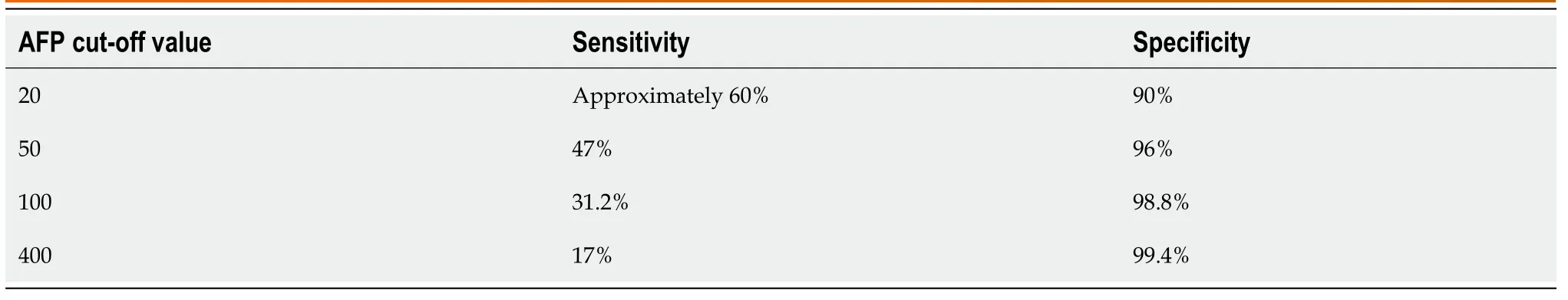
Table 2 Sensitivity and specificity of alpha-fetoprotein at different cut-off values[22-24]
For AFP-producing HCC,AFP plays an important role in initiating monitoring and terminating HCC therapy.A complete response of the treatment can be expected if preceding levels of AFP decrease to normal on follow ups.AFP,however,cannot be applied to monitor treatment response if its levels were not elevated prior to treatment[25-27].Approximately one-third of the patients with HCC have no AFP elevation[28].Nomuraet al[29] characterized those HCCs with low or no elevation of AFP.These patients generally have favorable prognosis with low probability of HCC recurrence and improved survival as compared to those with elevated AFP levels[29,30].In a large retrospective study including 1800 patients with HCC,42% had AFP < 20 ng/mL whereas 16% had AFP levels between 20 and 100 ng/mL.Thus,a total of 58% had AFP< 100 ng/mL.The authors observed that 67% of patients with HCC smaller than 5 cm had AFP ≤ 100 ng/mLvsonly 49% of the patients with HCC larger than 5 cm had AFP≤ 100 ng/mL.In addition,HCCs without AFP elevation (≤ 100 ng/mL) were less likely to develop portal vein thrombosis[31].
AFP-L3 and other HCC biomarkers
Based on the binding capacity of AFP to lens culinaris agglutinin (LCA),three separated bands of AFP glycoforms can be identified with the Western blotting.These are AFP-L1 (non-binding),AFP-L2 (intermediate binding) and AFP-L3 (LCA-reactive).AFP-L1 generally correlates with hepatic inflammation in chronic hepatitis while AFPL3 is more specific for HCC.AFP-L2 is derived from yolk sac and is detectable in the maternal serum during pregnancy[32] (Table 3).

Table 3 Overview of the diagnostic parameters for hepatocellular carcinoma
AFP-L3 is calculated as a fraction of AFP-L3 to total AFP.The cut-off values most commonly used for a positive AFP-L3 test for patients with HCC is 10% though levels above 15% are more specific[33].It is secreted in the initial tumor stages and thus can be used as an early HCC diagnostic marker[32,34].AFP-L3 level can also distinguish the histological differentiation of tumors[25].In patients with total AFP level ≤ 200 ng/mL,AFP-L3 specificity may reach 100% for HCC if it increases more than 35% of the total AFP[35].In a large multicenter prospective study of hepatitis C virus related HCC,the specificity of AFP-L3 was observed to be 92% but its sensitivity was fairly low at 37%,irrespective of the tumor stage[36].On the contrary,a number of recent studies reported a much higher sensitivity of AFP-L3 for diagnosing HCC[37-39].Ibrahimet al[39] evaluated the diagnostic efficacy of AFP-L3 among 20 healthy individuals,40 patients of chronic active hepatitis and 40 HCC patients with underlying chronic hepatitis B (CHB) or C.Among the HCC patients,30 (75%) had tumor size > 5 cm.At a cut-off point of > 12.3 ng/mL,AFP-L3 was 100% accurate in diagnosing the HCC[39].In a study by Ibrahimet al[39],20 healthy individuals,20 chronic liver disease patients and 40 patients HCV-induced HCC were included in theanalysis.A large proportion (65%) of the HCC patients had advanced stage of HCC.By using a cut-off value of 23 ng/mL,AFP-L3 had a sensitivity of 97.5% and specificity of 100% in predicting HCC at[37].Cerbanet al[38] investigated the diagnostic performance of AFP,AFP-L3,PIVKA-II and GPC-3 for HCC in a cohort including 52 cirrhotic and 101 HCC patients.AFP-L3 at a cut-off point of > 13.5 ng/mL was found to have a higher sensitivity of 84.7%,compared to other biomarkers[38].The sensitivity of AFP-L3 for HCC detection can be affected by its cut-off values,as well as the tumor size and stage[40].Data suggested that AFP-L3 could potentially be a valuable prognostic tool.The persistent elevation of AFP-L3 after HCC therapy was found to be associated with shorter survival[25].
Recently,a highly-sensitive AFP-L3 or hs-AFP-L3 was developed.Toyoda el al.determined the performance of hs-AFP-L3 among patients with 44 patients with chronic hepatitis or cirrhosis,and 54 patients with HCC.The sensitivity and specificity of hs-AFP-L3 were 84.9% and 88.6%,respectively[41].
Since both total AFP and AFP-L3 have limitations for the detection of HCC,studies have been conducted to combine AFP and AFP-L3 with other novel immunoassays to improve their performance.Des-gamma-carboxyprothrombin (DCP),also known as PIVKA-II (Protein Induced by vitamin K absence or antagonist-II),is a promising HCC biomarker.PIVKA-II is an abnormal product of liver carboxylation that reflects oncogenesis and HCC progression and is undetectable in healthy patients[25,42].
A systematic review noted that AFP,AFP-L3 combined with DCP enhanced their individual HCC predictive values with pooled sensitivity and specificity of 88% and 79%,respectively[43,44].Since 2002,Japan has included these 3 biomarkers in their HCC surveillance programs and they noted improved rates of early HCC identification and prognosis[43].When applying the GALAD score (age,sex,AFP,AFP-L3 and DCP),the HCC diagnostic accuracy was even higher [area under curve (AUC)0.976][45,46].A recent meta-analysis reported that AFP combined with GP73 (a Golgi specific membrane protein found in epithelial cells of bile ducts) has favorable sensitivity (84%) and specificity (92%) in diagnosing HCC with an AUROC value of 0.93[47].
Lately,a new HCC diagnostic marker,the long noncoding RNAs (lncRNAs),was developed[48].LncRNAs are transcribed by RNA polymerase II and play a role in the regulation of transcription and translation of proteins.Small extracellular vesicles (EV)transfer proteins,DNA,and RNA between tumor and nontumor cells.The dysregulated lncRNAs including EV-derived lncRNAs contribute to HCC progression and metastasis.EV-derived lncRNAs are,therefore,potential novel serum biomarkers.Kimet al[48] evaluated LINC00853,an EV-derived lncRNA in 90 patients with HCC and 92 without HCC in a cohort study.The AUROC of LINC00853 was 0.935 for identifying all-stage HCC and 0.969 for detecting early-stage HCC.These results were significantly better compared to AFP[48].In another study by Yuet al[49] reported that the combination of AFP with 2-lncRNA had a higher discriminative power than that of AFP alone in the diagnosis of HCC[49].
AFP ELEVATlON lN LlVER DlSEASES AND ClRRHOSlS
Rise in AFP has been recorded in different chronic liver diseases without HCC and other malignancies,hence,the results of AFP levels should be interpreted with caution[50].AFP is known to have a role in liver regeneration,inflammation and liver fibrosis.Less pronounced AFP elevation > 10 ng/mL has been reported in 15%-58% of chronic hepatitis and 11%-47% of cirrhosis[51].The usual cut off for differentiating benignvsmalignant liver conditions was at 500 ng/mL but can be variable[52].Studies have reported a progressive rise in serum AFP levels with increased histological severity from inflammation to cirrhosis to HCC[53].
ACUTE HEPATlTlS
The degree of AFP elevation in acute hepatitis is related to the severity of hepatic destruction[50,54].The levels range from 10 ng/mL-1000 ng/mL with occasional higher value from 3000 to 7190 ng/mL has been reported.Among children with acute hepatitis B,AFP was detected within 1 wk of the onset of clinical hepatitis and returned to normal by the time of recovery with loss of HBsAg[55].The possible mechanisms of AFP elevation include acute phase reaction to the liver injury,hepatocyte regeneration,or viral control or mediated AFP synthesis[56].AFP elevation after significant alanine aminotransferase (ALT) elevation is most likely due to liver regeneration and there is generally a latent period of 5-16 d[57].AFP generally peaks at a time when liver destruction is subsiding and hepatic remodeling begins[57].Hence,the highest level of AFP in acute hepatitis generally occurs during the recovery phase of illness and is an indicator of the liver regenerative process[58].
CHB
Elevated AFP levels are frequently observed during the course of CHB without HCC.The commonest cause of AFP elevation was the exacerbation of the underlying liver disease with or without changes in the status of hepatitis B virus (HBV) replication[41,52].High AFP levels associated with hepatitis flare were also found to be predictive of HBeAg to anti-HBe seroconversion[59,60].AFP levels usually decrease within 12 mo on antiviral therapy[61].Kimet al[61] reported that AFP normalization (< 20 ng/mL)was achieved in 89.5% of treated patients but remained abnormal in 40.6% of antiviral treatment naïve patients[61].
Persistent elevation of AFP > 100 ng/mL without a parallel increase in ALT level was reported to be a predictor of HCC with a sensitivity of 98.7% and specificity of 66.7%[59].Yuanet al[62] conducted a retrospective study of 302 treatment naive CHB patients with AFP positive status.After antiviral therapy,they found that there was a 6.35-fold increased HCC risk among those with persistently elevated AFP compared to those with normalized AFP levels[62].
In a metanalysis,Penget al[63] concluded that among HBV-related HCCs with low AFP levels,circulating miRNAs could be potential valuable biomarkers.For patients with AFP levels < 400 ng/mL,miR-125b and miR-205 demonstrated a sensitivity of 90% while combination of miR-15b and miR-130b had > 90% sensitivity and specificity.For AFP < 20 ng/mL,miR-26a,27a,7b and combination of miR-122 and miR-7b exhibited a sensitivity of 80% while combination of mir-29a,29c,133a,143,145,192 and 505 produced a specificity of > 80%.Additionally,the combination of miR-15b and miR-130b showed high diagnostic accuracy with sensitivity and specificity exceeding 90%.For differentiating HCC patients with low AFP levels (< 20 ng/mL)from non-HCC patients,the overall sensitivity and specificity of miRNAs were 0.85 and 0.74,respectively with AUC of 0.88 (95%CI:0.85-0.90).For patients with AFP <400ng/mL,the overall sensitivity and specificity were 0.84 and 0.76 with AUC of 0.88(95%CI:0.84-0.90).Hence,miRNAs are attractive HCC markers to detect HBVassociated HCC with low AFP levels[63].
Dickkopf WNT signaling pathway inhibitor 1 (DKK-1) is a glycoprotein that is expressed in various malignancies.Shenet al[64] conducted a study on 424 HCC,98 CHB,96 cirrhosis and 213 healthy controls and measured their DKK-1 Levels.The diagnostic cut-off was established at 2.153 ng/mL.DKK-1 proved useful in the detection of AFP-negative HCC with 70.4% sensitivity and 90.0% specificity.These values were validated in another cohort.When combined with AFP,DKK-1 increased detection rate of early-stage HCC with 73.1% sensitivity and 90.0% specificity.Additionally,elevated DKK-1 Levels can help differentiate HCC from other liver diseases such as CHB and cirrhosis with 69.1% sensitivity and 84.7% specificity[64,65].
Hepatitis B flare is defined as an abrupt elevation of serum ALT to 5 times the ULN or greater than 3-fold increase from baseline[66].During hepatitis flare,peak AFP level was usually observed 1-2 wk after peak ALT rise.Significant AFP elevation to > 2500 ng/mL had been documented with hepatitis flare.The normalization of AFP might take up to 3-12 mo[66].
The presentation varies from asymptomatic to overt hepatitis with decompensation and liver failure.AFP elevation was noted in 25%-30% of the patients with hepatitis flares.A study reported the annual incidence of hepatitis flares to be 27% in HBeAgpositive patients and 10% in HBeAg-negative patients with a mean follow-up period of 2 years.Changet al[67] reported that patients with AFP > 100 ng/mL during flare cleared HBeAg at a rate of 31% in 3 mo,62% in 12 mo and 72% in 18 mo.In contrast,the corresponding HBeAg clearance rates for those with AFP < 100 ng/mL were only 4%,15% and 19% in 3,12 and 18 mo respectively[67].Patients with bridging hepatic necrosis (BHN) had increased activation of the AFP-producing oval cell.BHN was noted in 80% of the cases with AFP levels > 100 mg/dL[53].BHN,AFP > 100 ng/mL and decreasing HBV DNA titers were identified as good prognostic indicators of an effective immune control with HBV DNA suppression and/or HBeAg clearance.
Severe and repeated hepatitis flares could also lead to development of cirrhosis or hepatic decompensation.Patients with severe hepatitis flare with BHN or AFP > 100 ng/mL but fail to suppress HBV DNA should be treated promptly with antiviral therapy.
CHRONlC HEPATlTlS C
AFP elevation is more greatly associated with HCV-associated HCC than HBVassociated HCC[64].The incidence of elevated AFP in chronic hepatitis C (CHC)patients range from 10%-43%[61].Elevated AFP > 20 ng/dL in CHC is associated with female gender,black race,increased age,genotype 1b,low albumin level,elevated aspartate aminotransferase (AST),elevated AST/ALT ratio,low platelet,prolonged PT,and increased ferritin levels[68,69].Yanget al[70] evaluated 279 CHC patients and found no correlation between AFP and the levels of HCV RNA[70].In the HALT C(Hepatitis C Antiviral Long-term Treatment) study,Di Bisceglieet al[71] observed AFP> 20 ng/mL in 16.6% of patients without HCC;it was associated with cirrhosis,female and Black patients[71].Black patients with CHC tend to have higher AFP elevation compared to other racial groups[71].Generally,HCV-related HCC does not have significant AFP elevation.Thus,AFP has especially low sensitivity to identify HCC in Black populations[71].
Fouadet al[72] reported that sustained virological response with direct-acting antiviral agents (DAA) therapy was associated with a significant reduction in serum AFP and might be used as a predictor of treatment response[72].In another study,60%of the DAA treated patients normalized AFP compared to only 23% without therapy[61].
Therapeutic phlebotomy has also been reported to reduce AFP levels in CHC[44].It has been postulated that iron mediated oxidative stress is associated with hepatic injury;iron depletion decreases the oxidative stress and indirectly lowers the AFP level[73].
NONALCOHOLlC FATTY LlVER DlSEASE
Nonalcoholic fatty liver disease (NAFLD) has become the most common liver disease in the Western world with about 10%-30% progress to cirrhosis[74].It is estimated that 6 million people in the United States have NASH with 1%-2% incidence of HCC annually.Published reports estimated that over 25% of NASH-related HCC occurred in patients without cirrhosis.With the high prevalence of NAFLD,risk stratification is essential to implement HCC surveillance programs[75].Currently,no surveillance of NALFD patients for HCC is recommended by AASLD[76].However,it has been suggested that NAFLD patients with cirrhosis or possible fibrosis or diabetes mellitus should have 6 monthly surveillancesviaultrasound (US) and tumor markers (AFP,AFP-L3 and DCP).Abdominal fat can be a hindrance,hence,patients with obesity can be alternatively surveilled using CT-Scan or magnetic resonance imaging[77].
An association between AFP elevation and NAFLD was first established by Babalıet al[78] in 2009.This study demonstrated a significant increase in AFP levels in patients suffering from NAFLD (4.09 ± 1.68) in comparison to the control group (2.95 ± 0.41)withPvalue < 0.05.Additionally,three subgroups of NAFLD were created based on the liver ultrasonography findings with presence of hepatorenal contrast or bright liver corresponding to grade 1,both hepatorenal contrast and bright liver signifying grade 2,and both pre-mentioned findings with bright liver being severe representing grade 3.The results showed a significant increase in AFP in grade 3 NAFLD (5.43 ±1.51) in comparison to grade 2 (3.97 ± 1.45) and grade 1 (2.92 ± 1.06) with aPvalue of 0.001.Triglyceride,cholesterol,low density lipoprotein,high-density lipoprotein,glucose and ALT levels were not significantly different in these groups[78].
Bestet al[79] published a case control study on German centers in 2020 describing the relationship between HCC and NASH using AFP,AFP-L3,DCP and the GALAD score for assessment.125 NASH patients with HCC and 231 NASH control patients without HCC were taken.The GALAD score recognized patients with HCC at any stage with an AUC of 0.96 which was superior to AUC of AFP (AUC 0.88),AFP-L3(AUC 0.86) and DCP (AUC 0.87) levels withP< 0.001 at a cut off about -0.63.The sensitivity was 84.8% and specificity was 95.2% at this cut off.They also conducted Japanese cohort study on 392 patients with NAFLD out of which 28 patients developed HCC.The mean GALAD score in these 28 patients predicted occurrence of HCC 1.5 years before its diagnosis.GALAD score was considerably higher in these patients compared to NASH patients who did not develop HCC[79].
EARLY VS ADVANCED LlVER ClRRHOSlS WlTH DECOMPENSATlON
Arrietaet al[80] reported that AFP ≥ 200 and 400 ng/mL had a sensitivity of 36.3% and 20.2% in determining HCC with 100% specificity.Improved method of analysis using progressive elevation of AFP ≥ 7 ng/mL/mo among cirrhotic patients increased the sensitivity to 71.4% with 100% specificity.This method was successful even when AFP values were below 200 ng/mL[80].
AFP can be elevated in patients with CHC or cirrhosis without any evidence of HCC[81].A persistent AFP value of 17.8 ng/mL was noted to have a 98.6% specificity,35%sensitivity and a positive predictive value of 97.7% in identifying patients with cirrhosis[82].Sudden fluctuations in AFP levels in patients with cirrhosis can be indicative of hepatitis flare,deterioration of liver disease and development of HCC[83].AFP has been applied routinely for HCC surveillance in cirrhotic patients.Haradaet al[83] showed that 40% of cirrhotic patients had AFP levels > 20 mg/dL[83].Manucet al[84] reported in a study of 2068 CHC patients with cirrhosis,30.1% without HCC had AFP > 15 ng/mL due to advanced age,severe liver injury with raised AST and ALT levels and low platelets[84].
In patients with cirrhosis,both the sensitivity and specificity of AFP for detection of early-stage HCC diagnosis can be enhanced by combining it with US.In a metaanalysis,the pooled sensitivity of AFP and US for any stage and early-stage HCC were 95% (83%-100%) and 60% (45%-74%) respectively,compared to only 72% (56%-86%)and 40% (22%-58%) for US only[85].Surveillance with AFP and ultrasonography in cirrhotic patients having an annual risk of HCC > 0.4% is cost-effective[86].
There are many risk scores that have been developed to predict HCC development among patients with chronic hepatitis and cirrhosis.However,many of them have not been standardized or carefully validated in different patient populations.Ideally,HCC prediction models should be developed for treated and untreated patients taking into account the patient ethnicity,significant comorbid conditions and ideally the molecular biomarkers[87].
PERSlSTENT AFP ELEVATlON lN THE ABSENCE OF LlVER DlSEASE
AFP is an important screening test for HCC and is also used in the diagnostic evaluation of other hepatic and non-hepatic conditions.Persistent AFP elevation has also been reported in patients without malignant or nonmalignant conditions.Hereditary persistence of AFP (HPAFP),a benign autosomal dominant disorder with no apparent disease or abnormality,should be considered as one of the differential diagnoses in patients with unclear etiology of persistent AFP elevation[88].HPAFP is a rare condition with only 20 reported cases in the literature[89].In contrast to malignant tumors with AFP usually > 500 ng/mL,the AFP concentration in HPAFP is mostly below 200 ng/mL,but levels up to 1500 ng/mL have been reported in some cases[88,90,91].The molecular mechanism of HPAFP can differ in unrelated families.Specific heterozygous point mutations are frequently found in the promoter region of the AFP gene related to hepatocyte nuclear factor 1 (HNF1) binding sites[92,93].These mutations usually result in an increased affinity for HNF1 and subsequently lead to increased AFP promoter activity and AFP gene transcription[94].Two-point mutations have been identified;the upstream substitution of cytosine (C) with adenosine (A) at amino acid position of 55 (-55 C > A) in the proximal HNF-1 binding site and upstream mutation caused by the substitution of Guanine (G) by Adenosine (A) at position 119 (-119 G > A) in the distal HNF-1 binding site[95,96].The first case of HPAFP was reported in 1984 by Greenberget al[91] in a Scottish family where a 38-year-old woman was noted to have persistently elevated AFP during post-partum[91].The AFP concentration of her amniotic fluid was normal and HPAFP was later confirmed by evaluating serum AFP levels and molecular testing in family members.In another report of 20 HPAFP cases,2 patients underwent unnecessary surgery and 3 had unnecessary chemotherapy due to their persistently elevated AFP[96].Though rare,hereditary causes should be considered in patients with unexplained and persistent AFP elevation.In a recent study by Jeonet al[89] on 4 Korean patients with persistently elevated AFP levels from 12.1 to 186.1 ng/mL for > 1 year,1 patient was found to have a hereditary cause by pedigree analysis even though the typical mutation of the AFP gene in the promoter region was absent.This case elucidated the heterogeneous nature of persistent AFP elevation and HPAFP is not always the result of mutation in the AFP transcription regulatory regions[89].
CONCLUSlON
AFP has been used for HCC surveillance widely in clinical practice.It,however,has limited sensitivity and specificity for HCC detection,and a proportion of patients with advanced HCC do not have AFP secretion.Moreover,patients with chronic liver diseases,especially those with cirrhosis are commonly identified with persistent AFP elevation without radiological evidence of HCC.For all these reasons,AFP is not recommended to be used as a sole marker alone for HCC surveillance.The diagnostic potential of AFP for early diagnosis of HCC can be enhanced by combining it with other novel diagnostic markers such as AFP-L3,PIVKA-II,and GP73.Although many have already endorsed diagnostic value,large number of multicenter studies encompassing larger cohorts and long-term assessment are required to confirm clinical utility.Additionally,algorithms integrating these serum markers with noninvasive diagnostic imaging modalities are needed to be developed for the early and accurate diagnosis of HCC.
 World Journal of Gastroenterology2022年2期
World Journal of Gastroenterology2022年2期
- World Journal of Gastroenterology的其它文章
- Nanotheranostics:A powerful next-generation solution to tackle hepatocellular carcinoma
- Multiple subcellular localizations and functions of protein kinase Cδ in liver cancer
- Observational Study ldentification of functional tumor necrosis factor-alpha promoter variants associated with Helicobacter pylori infection in the Sudanese population:Computational approach
- Prospective Study Outreach onsite treatment with a simplified pangenotypic directacting anti-viral regimen for hepatitis C virus microelimination in a prison
- Therapeutic endoscopy for the treatment of post-bariatric surgery complications
- Case Control Study Obesity is associated with decreased risk of microscopic colitis in women
