Are patients recovering from Kawasaki disease at increased risk for accelerated atherosclerosis? A meta-analysis
Yuan-Yuan Zeng ·Feng Chen ·Yong Zhang ·Xing Ji
Abstract
Background Recent studies have suggested that Kawasaki disease (KD) may cause endothelial dysfunction, which can potentially induce atherosclerosis.However, there is still no consensus on the relationship between KD and atherosclerosis.This article aimed to determine whether patients with a history of KD may be at increased risk for accelerated atherosclerosis via a meta-analysis.
Methods The PubMed, Embase, and SpringerLink databases were systematically searched.Studies on risk factors for atherosclerosis were included.A meta-analysis of case–control studies was performed using RevMan 5.3 software.
Results Twenty studies were included with a total of 1684 subjects (990 patients after KD and 694 controls).The metaanalysis showed that the level of carotid intima-media thickness (cIMT) (95% CI: 0.01, 0.03; P = 0.005) and high-sensitivity C-reactive protein (hsCRP) (95% CI: 0.00, 0.10; P = 0.03) were significantly higher in patients after KD than controls,whereas flow-mediated dilatation (FMD) (95% CI: − 5.14, − 1.26; P = 0.001) in patients after KD was significantly lower.There were no significant differences in total cholesterol (TC) (95% CI: − 0.13, 5.92; P = 0.06), low-density lipoprotein cholesterol (LDL) (95% CI: − 0.65, 2.08; P = 0.31), or triglycerides (TG) (95% CI: − 1.94, 8.03; P = 0.23).
Conclusion Endothelial dysfunction and inflammatory processes may exist in patients with a history of KD, which are risk factors for the development of atherosclerosis.
Keywords Atherosclerosis ·Endothelial dysfunction ·Kawasaki disease ·Meta-analysis
Introduction
Kawasaki disease (KD) is a form of idiopathic vasculitis that affects small-or medium-sized vessels throughout the body, with onset usually in infancy and childhood [1].It is considered one of the most common vasculitic disorders and is a leading cause of acquired heart disease in children living in industrialized countries [2].Recent studies [3,4] noted that KD may cause endothelial dysfunction and thus possibly contribute to atherosclerosis.There are many studies on coronary artery abnormalities (CAAs) related to KD, yet not enough is known about other associated complications of KD, especially atherosclerosis.While more than 50 years have passed since KD was first reported,there is currently still no consensus on the relationship between KD and atherosclerosis.In this article, we aimed to determine whether patients with a history of KD may be at increased risk for accelerated atherosclerosis via a meta-analysis.
Methods
Search strategy
The study protocol was designed and conducted based on Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.The PubMed,Embase, and SpringerLink databases were systematically searched from the study establishment date to August 1,2020 using the terms “mucocutaneous lymph node syndrome” or “Kawasaki disease” paired with the terms “atherosclerosis” or “atheroscleroses” or “atherogenesis”.The reference lists of the included studies were also scanned for additional relevant studies.The search was limited to studies written in English.
Study selection
The inclusion criteria of this meta-analysis were as follows:(1) case–control studies focusing on evaluating the risk factors for atherosclerosis in patients with a history of KD; (2)patients with KD as the case group and patients without KD(or healthy people) as the control group; (3) KD diagnosed clinically according to the Japan Kawasaki Disease Research Committee or American Heart Association's diagnostic criteria; (4) the selected study reported at least one of the following risk factors (predictive factors) of atherosclerosis: carotid intima-media thickness (cIMT), flow-mediated dilatation (FMD), lipid profiles (total cholesterol (TC), lowdensity lipoprotein cholesterol (LDL), triglycerides (TG)) or high-sensitivity C-reactive protein (hsCRP).Reviews, metaarticles, case reports, animal studies, and studies in which the outcomes of interest were not available were excluded from the current study.
Data extraction and quality assessment
Two independent investigators performed the literature search, data extraction, and quality assessment according to the inclusion and exclusion criteria.Any discrepancies in the process of data extraction and quality assessment were independently resolved by a third investigator.
The extracted data included the author, year of publication, country, age and gender of patients, number of subjects in the case and control groups, follow-up years, and outcomes.The quality of the included studies was evaluated using the Newcastle–Ottawa Scale (NOS) [5], which assesses the studies according to three categories: selection,exposure, and comparability.This assessment scale has a total score of 9.A score ≥ 7 was considered high-quality,3–7 was considered medium-quality, and ≤ 3 was considered low-quality.
Statistical analysis
RevMan5.3 software was used for data analysis.Publication bias was assessed via funnel plot analysis, and a symmetrical plot indicated no publication bias.Heterogeneity between studies was estimated byχ2 tests.A random-effects model was selected when significant heterogeneity was indicated(I2 > 50%), and a fixed-effects model was used when heterogeneity was not significant (I2 ≤ 50%).The weighted mean difference (WMD) with a 95% confidence interval (95% CI)was used for continuous outcomes.Significant heterogeneity was considered forP< 0.05.
Results
Search results
After searching the above databases, 1120 studies (174 from PubMed, 411 from Embase, and 535 from SpringerLink)were selected.After removing duplicates and screening titles and abstracts, 1063 studies (316 duplicate studies, 703 irrelevant studies, 9 reviews, 1 meta-article, 16 case reports,10 studies without available full text, and 8 animal studies)were excluded.After reading the full text, 20 relevant studies on risk factors for atherosclerosis in patients after KD were finally obtained.Details of the search process are shown in Fig.1.

Fig.1 Flow chart: details of the search process
Characteristics, quality and bias analysis of the included studies
Ultimately, we identified 20 case–control studies [6– 25]performed throughout the world from 2005 to 2018.The characteristics of the included studies are summarized in Table 1.After the Newcastle–Ottawa quality assessment was conducted, all of the studies obtained a score ≥ 7, which was considered high-quality (Table 2).Publication bias was assessed via funnel plot analysis.Overall, the plots were distributed symmetrically, suggesting no publication bias in the meta-analysis (Supplemental Fig.1).
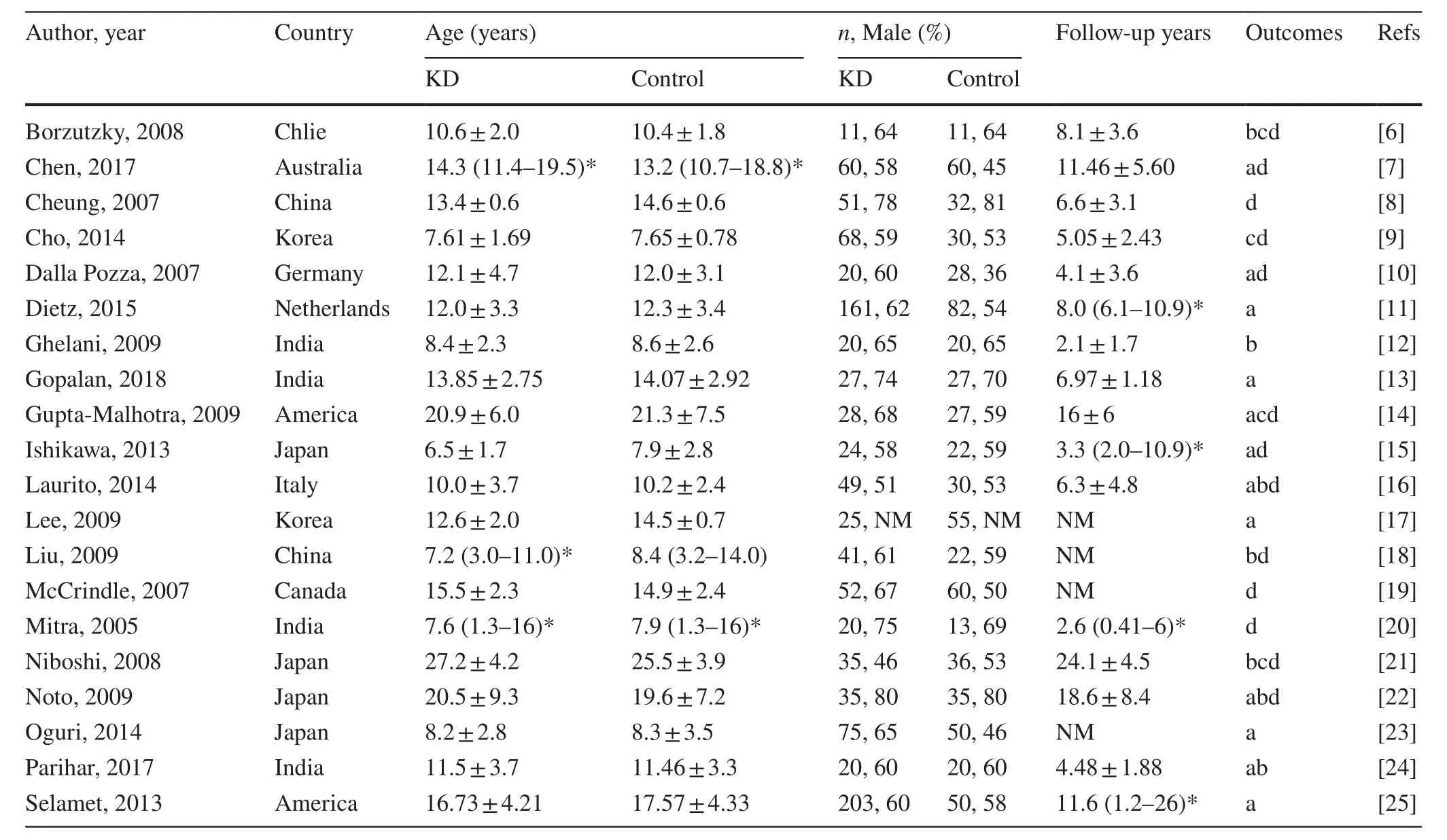
Table 1 Characteristics of included studies
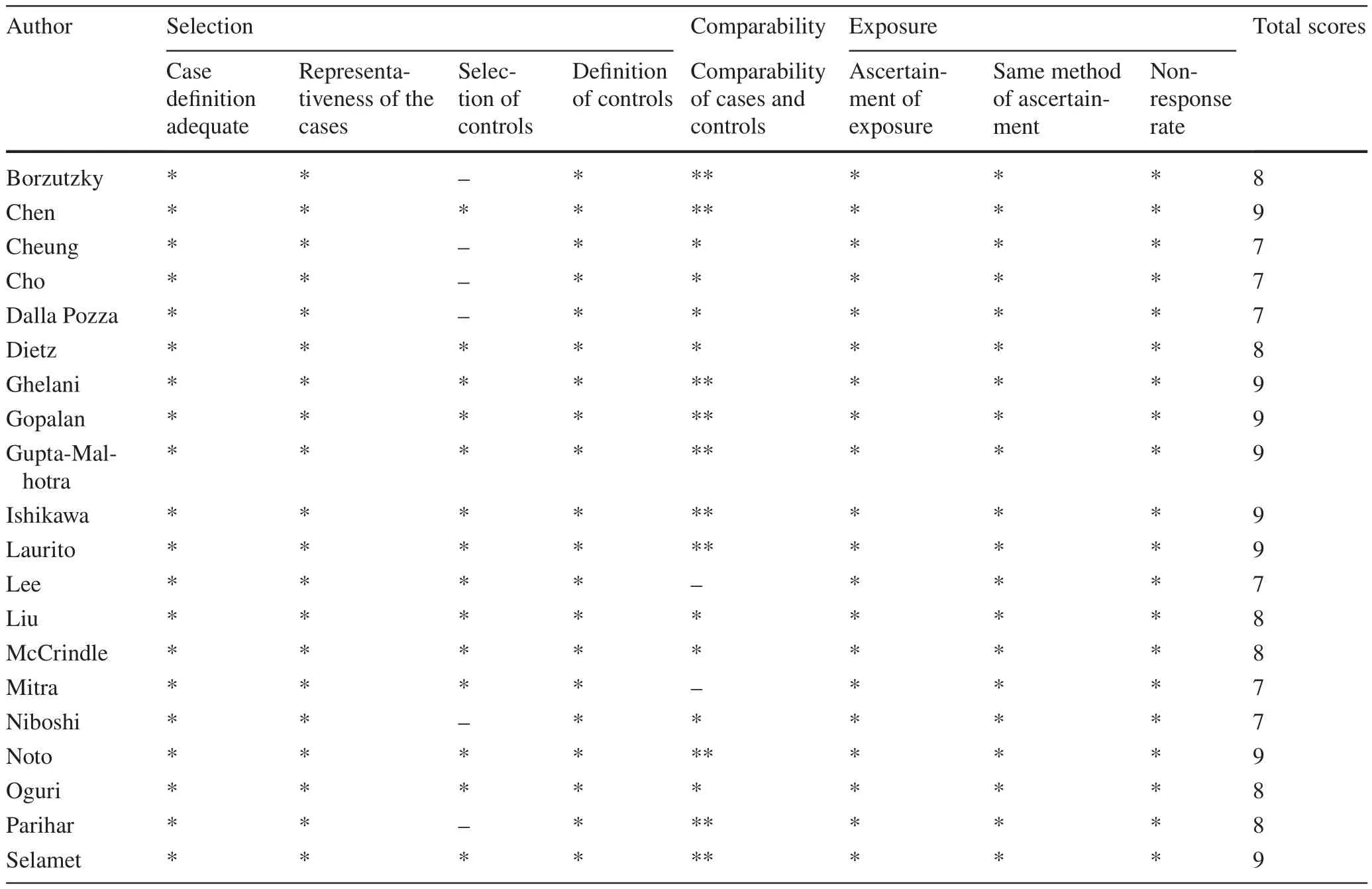
Table 2 Newcastle–Ottawa quality assessment of case–control studies included in the meta-analysis
Results of meta-analysis
Comparisons of cIMT between patients after KD and controls
Twelve [7, 10, 11, 13– 17, 22– 25] out of 20 studies included data on comparisons of cIMT between patients after KD and controls, involving 692 patients after KD and 470 controls.The heterogeneity test result was as follows:I2 = 84%,P< 0.001, indicating significant heterogeneity.To assess the influence of individual studies on the results, we conducted a sensitivity analysis by omitting one study in each turn.However, there was no change in the result, which confirmed the stability of our study.A random-effects model was then applied.The results showed a significantly higher level of cIMT in patients after KD than controls (95% CI: 0.01, 0.03;P= 0.005) (Fig.2 a).
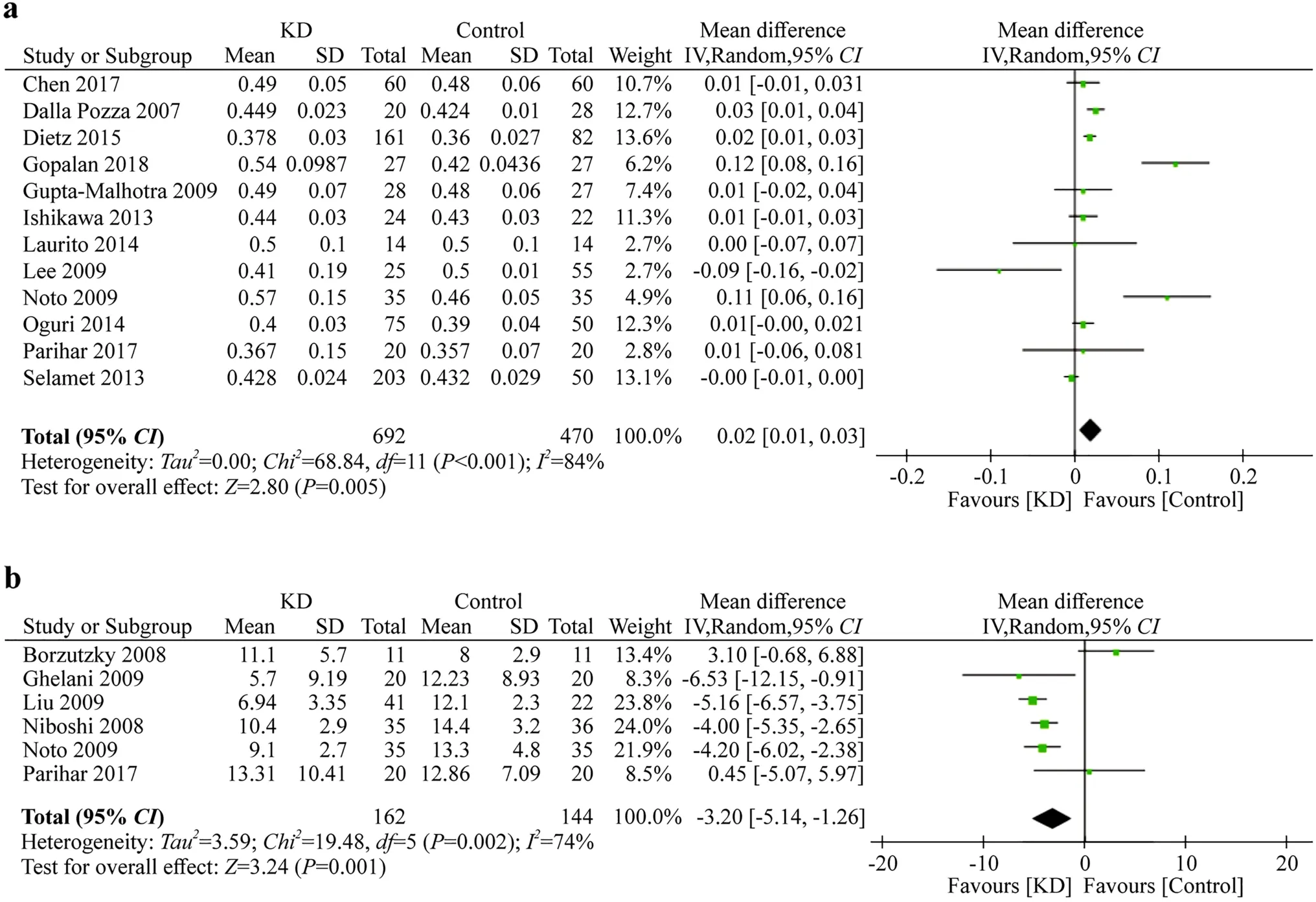
Fig.2 a Forest plots comparing on cIMT between KD patients and controls; b Forest plots comparing on FMD between KD patients and controls
Comparisons of FMD between patients after KD and controls
Seven [6, 12, 16, 18, 21, 22, 24] out of 20 studies investigated FMD between patients after KD and controls.The heterogeneity test result was as follows:I2 = 87%,P< 0.00001, indicating significant heterogeneity.A sensitivity analysis was also conducted.As a result, we excluded the study by Laurito [16], and the subsequent heterogeneity result wasI2 = 74%,P< 0.002.We found that none of the patients with KD enrolled in Laurito’s study had any coronary abnormalities, which was different from other studies.Finally, the remaining 6 studies, including 162 patients after KD and 144 controls, were included in the meta-analysis, and a random effects model was applied.The results showed a significant lower level of FMD in patients after KD than controls (95% CI: − 5.14, − 1.26;P= 0.001) (Fig.2 b).
Comparisons of hsCRP between patients after KD and controls
Four [6, 9, 14, 21] out of 20 studies recorded data on hsCRP between patients after KD and controls and involved 142 patients after KD and 104 controls.The heterogeneity test result was as follows:I2 = 0%,P= 0.40, indicating no significant heterogeneity.Afixed effects model was used, and the result showed a significantly higher level of hsCRP in patients after KD than controls (95% CI: 0.00, 0.10;P= 0.03) (Fig.3 a).
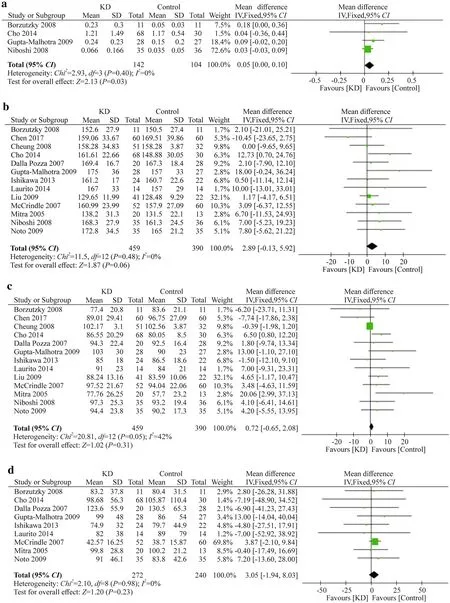
Fig.3 a Forest plots comparing on hsCRP between KD patients and controls; b Forest plots comparing on TC between KD patients and controls; c Forest plots comparing on LDL between KD patients and controls; d Forest plots comparing on TG between KD patients and controls
Comparisons of TC between patients after KD and controls
Thirteen [6– 10, 14– 16, 18– 22] out of 20 studies included data on TC between patients after KD and controls and involved 459 patients after KD and 390 controls.The heterogeneity test result was as follows:I2 = 0%,P= 0.48, indicating no significant heterogeneity.A fixed-effects model was used, and the result showed no significant difference in TC between patients with KD and controls (95% CI: − 0.13,5.92;P= 0.06) (Fig.3 b).
Comparisons of LDL between patients after KD and controls
Thirteen [6– 10, 14– 16, 18– 22] out of 20 studies included data on LDL between patients after KD and controls and involved 459 KD patients and 390 controls.The heterogeneity test result was as follows:I2 = 42%,P= 0.05, indicating no significant heterogeneity.A fixed-effects model was used, and the result showed no significant difference in LDL between patients after KD and controls (95% CI: − 0.65,2.08;P= 0.31) (Fig.3 c).
Comparisons of TG between patients after KD and controls
Nine [6, 9, 10, 14– 16, 19, 20, 22] out of 20 studies included data on TG between patients after KD and controls and involved 272 patients after KD and 240 controls.The heterogeneity test result was as follows:I2 = 0%,P= 0.98, indicating no significant heterogeneity.A fixed effects model was used, and the result showed no significant difference in TG between patients after KD and controls (95% CI: − 1.94,8.03;P= 0.23) (Fig.3 d).
Discussion
There are still many unknown aspects regarding the longterm prognosis of patients with a history of KD, especially with regard to atherosclerosis.The lipid profile [26], cIMT[27, 28], FMD [21], and inflammatory biomarkers, including C-reactive protein (CRP) [29], are potential markers of the presence of atherosclerosis.On the other hand, the above markers of atherosclerosis also appear in patients with a history of KD.Nevertheless, there is still no consensus on the relationship between KD and atherosclerosis.
To our knowledge, there has been only one meta-analysis [30] conducted on this topic previously, which included 16 case–control studies and involved 870 subjects (421 patients after KD and 449 non-KD controls).This previous study investigated the FMD and lipid profile of cases and controls and found that TC levels, LDL levels, and FMD were significantly different between patients after KD and healthy people.Our study updated the previous meta-analysis by including 20 available case–control studies with a total of 1684 subjects (990 patients after KD and 694 non-KD controls) and compared six atherosclerosis risk factors(cIMT, FMD, hsCRP, TC, LDL and TG) between cases and controls.We found that endothelial dysfunction may exist in patients with a history of KD, as cIMT and FMD were significantly different between patients after KD and healthy people.Moreover, the sensitivity analysis on FMD between patients after KD and controls indicated that KD patients with CAAs may be more likely to have a risk of atherosclerosis than others without CAAs.This view is consistent with studies by Ishikawa et al.[15] and Liu et al.[18].These authors categorized the participants into three groups for comparisons: group 1 with CAAs, group 2 without, and group 3 comprised healthy controls.They both found that the FMD differed significantly among the three groups.Additionally, we found that hsCRP was significantly increased in patients with KD, indicating that patients after KD may be at increased risk of inflammation-induced endothelial dysfunction.However, unlike the previous meta-analysis, we found no statistically signifi-cant differences between patients after KD and controls in TC, LDL and TG.This difference may be caused by duplicate data in the previous article when compared to the indices of TC and LDL.
Our study still has the following limitations.(1) There is currently an increasing number of incomplete (atypical) KD patients currently, as the diagnosis of KD varies.However,in our study, we included only those who had been diagnosed clinically according to the Japan Kawasaki Disease Research Committee or American Heart Association’s diagnostic criteria.(2) The 2017 American Heart Association guidelines [31] use coronary artery Z scores to classify KD patients into five risk levels.Most of the included studies only described the presence of CAAs in patients but did not stratify them based on risk categories.Including more highrisk patients with CAAs would be more desirable to evaluate the risk of atherosclerosis.If more studies stratify the KD patients based on risk categories be conducted in the future,then subgroup analysis can be performed and the results can be more reliable.
In conclusion, we found that endothelial dysfunction and inflammatory processes may exist in patients with a history of KD.These are risk factors for the development of atherosclerosis.However, these results should be interpreted cautiously and should be further validated by prospective studies.
Author contributionsConceptualization: YYZ; writing—original draft preparation: YYZ and FC; writing—review and editing: YYZ, FC, XJ and YZ; funding acquisition: FC.All authors have read and agreed to the published version of the manuscript.
FundingThis research was supported by the Specially Appointed Medical Expert Project of Jiangsu Commission of Health (2019) and the Medical Science and Technique Foundation of Nanjing Health Commission (YKK19104).
Data availability statementThis article data are available to authorized users.
Compliance with ethical standards
Ethical approvalNot needed for the meta-analysis.
Conflict of interestThe authors declare no conflicts of interest.
 World Journal of Pediatrics2021年5期
World Journal of Pediatrics2021年5期
- World Journal of Pediatrics的其它文章
- Role of ultrasound in the diagnosis of cervical tuberculous lymphadenitis in children
- Serum vitamin E concentration is negatively associated with body mass index change in girls not boys during adolescence
- Pediatric upper extremity firearm injuries: an analysis of demographic factors and recurring mechanisms of injury
- Nasogastric or nasojejunal feeding in pediatric acute pancreatitis:a randomized controlled trial
- Febrile infants: written guidelines to reduce non-essential hospitalizations
- Acute generalized exanthematous pustulosis as a manifestation of Kawasaki disease
