Environmental exposure during pregnancy and the risk of childhood allergic diseases
Ming-Zhi Zhang ·Shan-Shan Chu ·Yan-Kai Xia ·Dan-Dan Wang ·Xu Wang
Abstract
Background Allergic diseases are one of the most common and important diseases that can exert hazardous effects on children's health.The prevalence of allergic diseases in childhood is gradually increasing all over the world in recent decades.Known causes of these diseases include anomalous immune responses and allergic inflammatory reactions, but the causes of allergic diseases in childhood are complex.
Data sources PubMed, Cochrane Library, Embase and Web of Science were searched for articles focusing on environmental exposure during pregnancy and the risk of childhood allergic diseases, including asthma and atopic dermatitis, and the possible underlying mechanism.
Results In terms of environmental factors, allergic diseases in childhood are closely related to environmental chemical exposure during pregnancy, including bisphenols, phthalates acid esters, perfluorochemicals, polybrominated diphenyl ethers,and polychlorinated biphenyls.However, allergic diseases in childhood are also closely associated with maternal dietary nutrition, maternal intake of drugs, such as acetylsalicylic acid (aspirin), paracetamol and antibiotics, and maternal lifestyle.
Conclusions Several harmful environmental factors during pregnancy can result in the interruption of the function of helper T cells (Th1/Th2), cytokines and immunoglobulins and may activate allergic reactions, which can lead to allergic diseases during childhood.
Keywords Allergic diseases ·Children ·Environment ·Pregnancy
Introduction
The causes of allergic diseases in childhood are complex and involve hereditary and environmental factors [1, 2].Epidemiological researches have explored some risk factors of allergic diseases in childhood and have provided prevention and treatment strategies; however, there are still many factors that need to be explored further.Common allergic diseases in childhood include eczema, food allergy (FA), asthma and allergic rhinitis (AR).The onset of FA and eczema typically occurs shortly after birth.Eczema may then develop into wheezing or AR, and persistent allergic wheezing may progress to asthma [3].Given the rapid increase in allergic diseases in recent decades, these diseases have been recognized as public health challenges [4].
Pregnancy is an important period for the development of fetal tissues and organs.During pregnancy, individuals are extremely sensitive to stimulation from the external environment.Developmental Origin of Health and Disease theory indicates that exposure to various environmental factors during pregnancy is an important cause of long-term illness [5].Furthermore, fetuses are more susceptible to harmful environmental chemicals because their systems are still under development and may not be able to process or remove certain chemicals.
Environmental chemicals are widely found in pesticides,herbicides, flame retardants and personal care products.The high stability of some harmful environmental chemicals makes it possible to have relatively high rates and levels of detection in polluted water, air and soil after several years of discharge.Pregnant women can be exposed to diverse environmental chemicals through their occupations, diets, medical products and household cleaning products by the respiratory tract, digestive tract and skin contact [6].Maternal exposure can be transmitted to fetuses and infants through the placenta, umbilical cord blood, and breast milk [7].Some harmful environmental chemicals may have immunedisrupting effects and influence the risk of allergic diseases.These chemicals may interrupt the functions of helper T cells (Th1/Th2), cytokines and immunoglobulin levels and may trigger allergic reactions [8, 9].
In addition to being associated with exposure to environmental chemicals during pregnancy, children’s allergies are also affected by maternal dietary nutrition, drugs intake and lifestyle.This review aims to summarize existing knowledge on environmental exposure during pregnancy and the risk of childhood allergic diseases, including asthma and atopic dermatitis (Table 1, Fig.1).In addition, this review aims to summarize the underlying mechanism, mainly focusing on knowledge gaps and how to combine recent developments in different research areas to prevent allergic diseases in childhood.
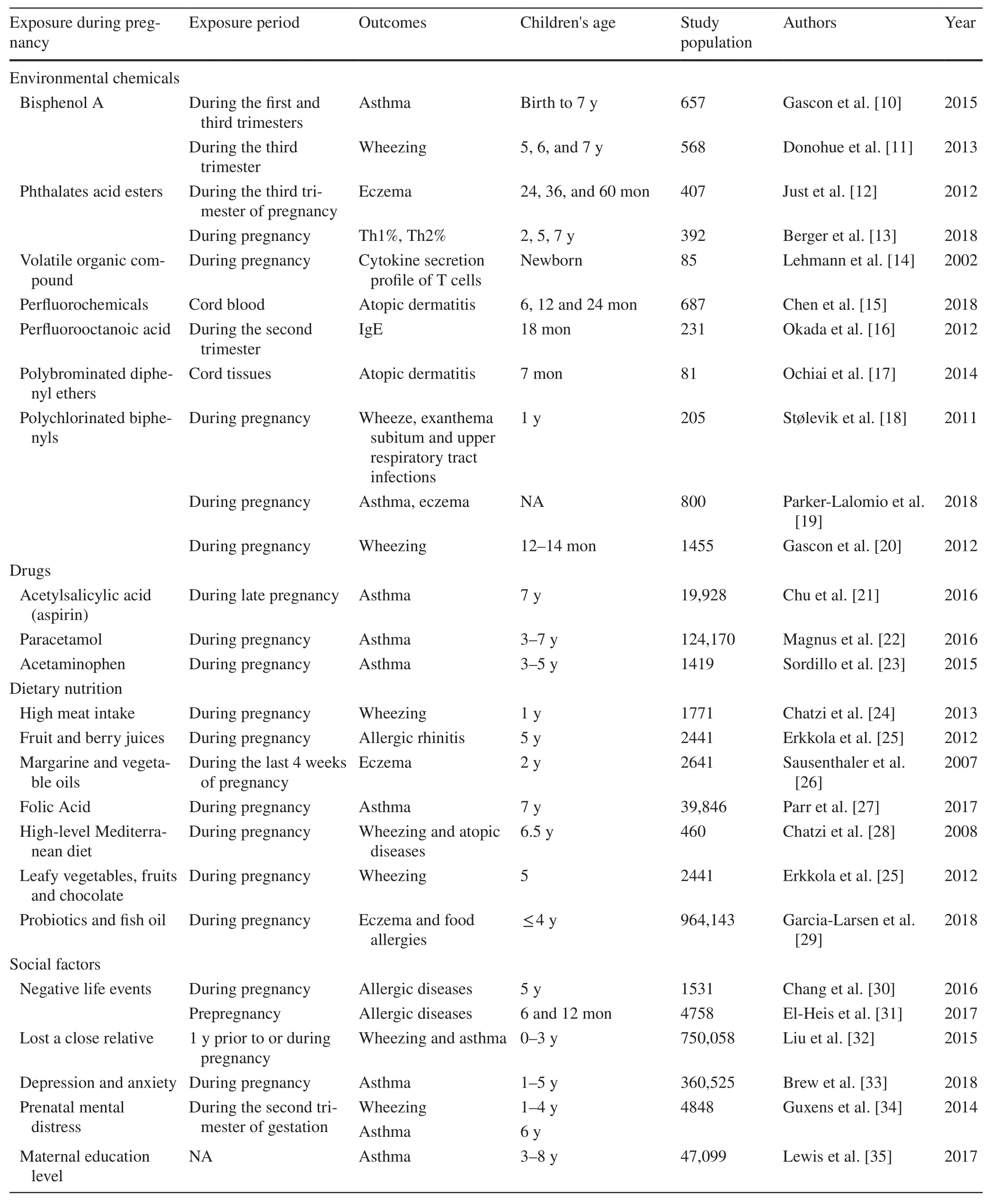
Table 1 Research report on the correlation between environmental exposure during pregnancy and allergic diseases in children
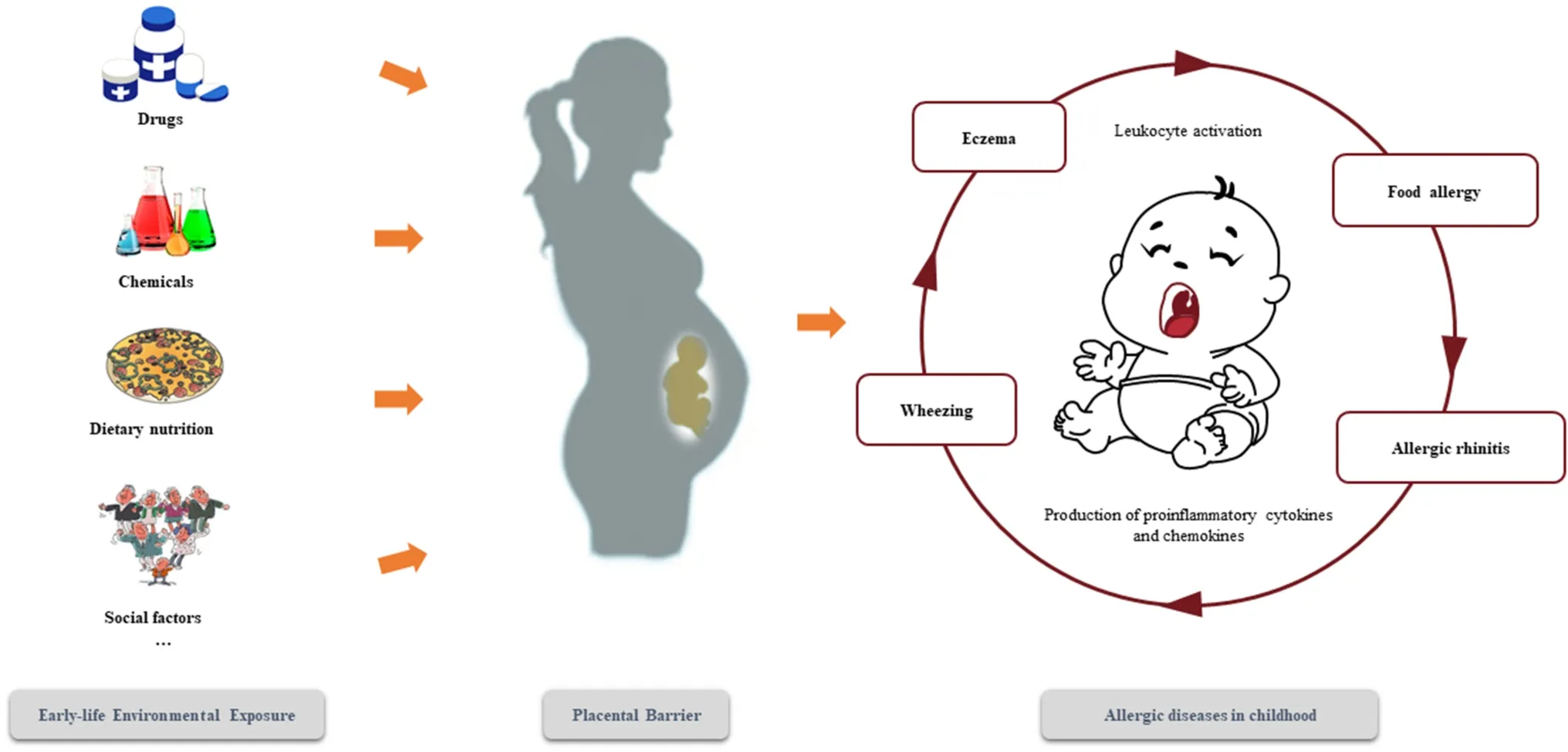
Fig.1 The overview of this review
Environmental chemicals exposure during pregnancy and childhood allergic diseases
Environmental chemicals, which are harmful, include short half-lived chemicals and persistent organic pollutants(POPs).Bisphenols are common existing harmful short half-lived chemicals.As the basic raw materials of organic chemical industry, bisphenols are widely used in industrial and agricultural production and in daily life.People may have long-term or short-term exposure to bisphenols through food packaging, dental materials, medical equipment, thermal paper, toys and some consumer care products [36– 38].Representative environmental phenolic chemicals, such as bisphenol A (BPA), have attracted special attention worldwide owing to their high yield, wide distribution and wide use, as well as their potential adverse biological effects.In 2015, Gascon et al.found that maternal BPA exposure during pregnancy could increase the risk of asthma in childhood [10], whereas another study found that BPA exposure in pregnant women was negatively correlated with the incidence of wheezing in their children [11].Because the exposure window in the second study was in late pregnancy,while mid pregnancy is the key period for bronchial maturation, BPA exposure levels at mid pregnancy might more accurately reflect BPA exposure during pregnancy and child respiratory allergic reaction [11].
Phthalate acid esters (PAEs) are a classic type of endocrine-disrupting chemicals, the main components of which are alkyl and 1, 2-dicarboxylic acid or dialkyl esters.PAEs are mainly used as plastic additives (plasticizers) added to plastics and perfumes and are widely contained in food products, cosmetics, consumer products and personal care products [39, 40].With more and more extensive usage and with increased production of PAEs, PAEs are accumulating and have become ubiquitous in the environment.Human beings have inevitably been exposed to PAEs for a long time.The adverse health effects exerted by PAEs have become a focus of attention of many scholars in recent years, especially for PAE’s reproductive and developmental toxicity [41].A positive relationship was observed between mono-benzyl phthalate (MBzP), a metabolite of PAEs, and increased risk of developing eczema in early childhood [12].In addition,maternal urinary concentration of MBzP was found to be associated with increased risk of childhood wheeze [10].The changed levels of Th1 and Th2 cells detected in children’s blood, which are linked with maternal exposure to phthalate during pregnancy, could result in immune dysregulation [13].In addition, prenatal exposure to a mixture of volatile organic compound may lead to the alternation of cytokine secretion profile of cord-blood T cells [14].
Maternal exposure to some harmful environmental chemicals other than short half-lived chemicals also can affect children’s allergic reactions.Per-and poly fluoroalkyl substances (PFAS) are categorized as POPs, mainly including perfluorooctanoic acid (PFOA), perfluorooctane sulfonate acid (PFOS), perfluorodecanoic acid (PFDA), perfluorododecanoic acid (PFDoA) and perfluorohexane sulfonic acid (PFHxS), which are synthetic compounds with strong fluorocarbon covalent bonds [42].PFAS are widely used in non-stick cooking pots, leather, textiles, surfactants and other household products owing to the strong thermal, biological and chemical stability of these chemicals [43, 44].Previous studies found that PFOA and PFOS exposure could lead to immunosuppression in humans [45], but the conclusions were inconsistent [46].Recent epidemiological studies suggested that PFOA, PFDA, PFDoA and PFHxS exposure during pregnancy might result in increased risk of atopic dermatitis in infants [15].Another study found that prenatal PFOA exposure was closely associated with decreased immunoglobulin E (IgE) level in umbilical cord blood [16].
Polybrominated diphenyl ethers (PBDEs), a kind of POP belonging to brominated flame retardants, are organobromine compounds widely used in industrial applications, such as electronics, building materials, textiles, plastics and other materials [47].Penta-BDEs, octa-BDEs, and deca-BDE are the three main commercial compounds of technological PBDEs.PBDEs can gradually release to the surrounding environment owing to their non-reactivity, and they have been extensively detected in sea fish, sediment, air, soil and so on.PBDEs have been detected in serum samples from pregnant women.In addition, increases in PBDE concentrations in breast milk have been found in Canada and in the US during the last decade of the twentieth century [48,49].Infants aged 7 months old showed an alternation of the risk of atopic dermatitis development with prenatal PBDEs exposure [17].
Polychlorinated biphenyls (PCBs), which are divided into non-dioxin-like PCBs and dioxin-like PCBs, are used in electrical apparatus, carbonless copy paper and heat transfer fluids as dielectric and coolant fluids owing to their chemical stability [50, 51].PCBs were banned or strictly limited worldwide after the 1960s when they were found to contain extensive environmental toxicity [52].However, due to the continued persistence and ubiquity of PCBs, they remain a threat to human health.Positive associations were observed between maternal PCBs exposure levels, exanthema subitum and upper respiratory tract infections in the first year of life[18].In addition, prenatal exposure to PCBs increased the risks for asthma and eczema in offspring [19], as well as wheeze [20].
Recent population-based studies found an association between air pollution exposure during pregnancy and the development of childhood asthma and wheezing; however,the association included gender differences and was influenced by other factors, such as psychological stress [53, 54].Furthermore, air quality varies greatly between countries with different economic conditions, which could affect air pollution levels of exposure during pregnancy.
Drugs exposure during pregnancy and childhood allergic diseases
During pregnancy, mothers may take recommended medications with appropriate doses due to illnesses, such as trauma, infection, fever and cold.However, in such a sensitive period, even taking widely recognized drugs will cause related adverse reactions, and may even affect the growth and development of the children.
Acetylsalicylic acid (aspirin), which is widely used as an analgesic, antipyretic and anti-inflammatory medication in the general population, is one of the most important medications in the basic health system.In pregnant patients, low doses of acetylsalicylic acid are commonly prescribed to prevent antiphospholipid syndrome-related miscarriage and preeclampsia [55].However, during pregnancy exposure to therapeutic doses of aspirin was related to childhood asthma at 7 years of age as reported in 2016 by a prospective cohort study in the US [21].
Paracetamol, the commonly used non-anti-inflammatory antipyretic and analgesic, is similar to aspirin.It is also a recommended analgesic/antipyretic for pregnant women.The Norwegian Mother and Child Cohort Study provided evidence that prenatal paracetamol exposure had an independent association with asthma in children aged 3 and 7 years [22], while another longitudinal cohort study found that prenatal non-anti-inflammatory antipyretic and analgesic use was linked to increased asthma during aged 3–5 years but not during aged 7–10 years [23].
In addition, antibiotics have an infection-fighting effect by inhibiting or killing bacteria.In 2018, one retrospective cohort study reported a dose-dependent association between maternal antibiotic use and asthma risk in childhood, but there was no evidence to determine which specific antibiotic was responsible for the association [56].The importance of using real-world and randomized controlled trials evidence to evaluate safety of drug use during pregnancy for the fetus and child should be highlighted [57, 58].
Dietary exposure during pregnancy and childhood allergic diseases
The diet of pregnant women not only provides nutrition for the development of the fetus, but diet may also lead to childhood allergic diseases.Dietary factors include overall dietary intake patterns, specific food consumptions ( fish,fruits, vegetables) and individual immune regulating nutrient intakes [59].Several previous studies focused on the relationship between maternal nutritional dietary and allergic diseases in childhood.
Maternal total dietary intake patterns can affect the immune responses of their offspring as it was found that high maternal intake of meat may increase the risk of asthma in the first year of life [24].Also, certain foods consumed during pregnancy were proved to be associated with allergic diseases in childhood.It was observed that maternal consumption of fruit and berry juices was positively associated with elevated risk of AR in 5-year-old children [25].Intake of vegetable oils and margarine during the last four weeks of pregnancy could increase the incidence rate of eczema in their offspring in the first two years of life [26].Folic acid, as the recommended medication to prevent neural tube defects, has also been found to pose potential risks for childhood asthma.Pregnant women taking supplemental folic acid at or above the recommended dose, combined with a diet rich in folate,could reach excessive levels of folate intake, which may lead to a slightly increased risk of asthma in childhood [27].
Different from other exposures, dietary exposure during pregnancy is more likely to be controlled by individuals.Rational dietary structure during pregnancy can be a protective factor for childhood allergic diseases.A high-level,Mediterranean dietary pattern during pregnancy had a protective effect on wheezing and on other atopic diseases in childhood, which reflected fetal exposure to several antioxidant compounds, such as rich antioxidants in cereals(vitamin E, phenolic acids and phytic acid) that might help protect the respiratory tract from oxidative damage in childhood [28].Moreover, another study indicated that specific nutrients during pregnancy were more relevant to childhood allergic outcomes, not overall diet quality [60].Certain nutrients, such as oligosaccharides (soluble liber),antioxidants, polyunsaturated fatty acids, folic acid and other vitamins, have been shown to protect the immune system in childhood [61].
Current evidence suggested that maternal intake of nutrients (vitamin D, vitamin E, and zinc) had a protective effect on childhood wheezing, but the effect was inconclusive on asthma or other allergic diseases [62].Maternal consumption of leafy vegetables, fruits and chocolate during pregnancy might protect against wheezing in children at 5 years of age [25].Supplements of probiotics and fish oil during pregnancy could reduce the risk of eczema and food allergies [29].Therefore, dietary status during pregnancy is closely related to childhood allergic diseases, and a reasonable dietary structure (e.g., a Mediterranean dietary pattern with abundant antioxidants) during pregnancy will contribute to children’s immune system.
Social factors exposure during pregnancy and childhood allergic diseases
As modern medicine has transformed into a biopsychosocial model, an increasing number of studies have focused on social factors, which generally include psychological factors, education, sleep quality, income, and so on.Numerous studies suggested that gestational psychology and maternal education levels are risk factors for allergic diseases in their children [35, 63].Maternal psychological factors mainly refer to stress, anxiety, depression and distress and are possibly caused by negative life events.Childhood allergic diseases, possibly owing to chronic high cortisol levels and oxidative stress, are likely to originate from maternal psychological factors [30, 31].
A meta-analysis indicated that prenatal maternal stress(PNMS) might have an adverse impact on the development of respiratory system, thus causing the morbidity of respiratory system in childhood, including wheezing and asthma[64].Additionally, previous research indicated that PNMS was associated with asthma in children aged 0–3 years, but not 4–15 years [32].However, PNMS exposure was usually measured through self-reported questionnaires, which can potentially deviate from the actual levels of exposure [65].A systematic review elucidated that PNMS exposure during the third trimester was more influential to allergic diseases in childhood than exposure during the first and second trimesters [66], while another study indicated that the exact time of critical windows was not easy to assess [67].Apart from PNMS, a Swedish population-based study indicated that cumulative exposure to depression or anxiety during pregnancy was a possible cause of childhood asthma after controlling for confounding factors from fathers and sibling [33].
Prenatal psychological factors can lead to allergic diseases in childhood [34].In addition, maternal education level and other social factors are also associated with allergic diseases in childhood [68, 69].In ten integrated European birth cohort studies, children of mothers in the lowest education level were more likely to have asthma than those born to mothers with the highest education level.The possibility of higher exposure to risk factors may explain the vulnerability of allergic diseases in children with less educated mothers [35].For less educated women, it is beneficial to grasp relevant knowledge about potential adverse exposures and to avoid them.
In addition, employment and family conditions during pregnancy also need to be seriously considered as risk factors for childhood allergic diseases.To support early prevention strategies and therapeutic interventions for allergic diseases in childhood, further studies exploring the combined effects of social factors and other environmental factors are still required [67, 70].
Possible mechanism
The adsorbed components of environmental chemicals may pass through the placental barrier to the fetus from the mother’s blood.Some environmental chemicals have been reported to induce Th2 cell differentiation.The imbalance of Th1 and Th2 cells makes Th2 cells secrete more allergy cytokines, such as interleukin (IL)-4 and IL-5, and increases the production of IgE, which may induce allergic diseases and allergic reactions [71].In addition, IL-9 and IL-10 are also associated with allergic diseases, but the role of environmental chemicals on IL-9 and IL-10 needs to be further explored [72, 73].Environmental chemicals may exacerbate autoimmune responses.Low-dose exposure to some harmful environmental chemicals during pregnancy can accelerate the differentiation of Th17 cells, increasing the secretion of cytokines IL-17 and IL-21 [74].Th17 cells are involved in assisting Th1 and Th2 cell lineages, mediating the occurrence of various autoimmune and inflammatory diseases.Immune cells (mast cells, lymphocytes, etc.),stimulated by environmental estrogen-like chemicals, may express an estrogen receptor-mediated degranulation effect of mast cells and basophilic cells [75].In addition, some chemicals, such as BPA, also can be presented as allergens directly and cause allergic reactions.
Hypothesized mechanisms through which psychological factors may increase the risk of childhood allergic diseases are thought to overlap with a disrupted balance of immune,neuroendocrine, and autonomic nervous systems by intrauterine programming of the hypothalamic–pituitary–adrenal axis [34, 76].The influence of environmental factors on allergic diseases is mediated partly by epigenetics.Epigenetics involves a variety of mechanisms, including DNA methylation, histone modification, and microRNAs that modify translation [77].Epigenetic modifications play a key role in the differentiation of T cell lineages and affect the balance between different Th cells [78].Evidence indicates that epigenetics is also critical to the regulation of airway epithelial cells.The diet of pregnant women can alter children's epigenetics.Changes in histone acetylation in the placenta of mothers who regularly eat fish or olive oil may affect the immunity of newborns [79].In addition, unhealthy maternal psychology during pregnancy may impair the growth of fetal lung and airways due to intrauterine growth restriction, but this hypothesis remains controversial [34].
Conclusions
In recent years the prevalence of childhood allergic diseases has increased worldwide, becoming a threat to children's health.More and more studies have shown that various harmful environmental factors during pregnancy may be important risk factors for allergic diseases in childhood.The association between these factors and allergic diseases needs to be explored in more cohort studies with large sample sizes.Avoidance of harmful environmental factors during pregnancy can prevent allergic diseases and reduce the burden of allergic diseases in childhood.
Author contributionsZMZ and CSS contributed equally to this work.ZMZ contributed to the writing of the original draft.CSS contributed to reviewing and editing.XYK contributed to conceptualization.WDD contributed to conceptualization.WX contributed to revision and supervision.All the authors approved the final version of the manuscript to be published.
FundingNot applicable.
Compliance with ethical standards
Ethical approvalNot needed.
Conflict of interestNofinancial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
Data availabilityData sharing not applicable to this article as no datasets were generated or analysed during the current study.
 World Journal of Pediatrics2021年5期
World Journal of Pediatrics2021年5期
- World Journal of Pediatrics的其它文章
- Acute generalized exanthematous pustulosis as a manifestation of Kawasaki disease
- Febrile infants: written guidelines to reduce non-essential hospitalizations
- Rising serum potassium and creatinine concentrations after prescribing renin–angiotensin–aldosterone system blockade:how much should we worry?
- Role of ultrasound in the diagnosis of cervical tuberculous lymphadenitis in children
- Nasogastric or nasojejunal feeding in pediatric acute pancreatitis:a randomized controlled trial
- Pediatric upper extremity firearm injuries: an analysis of demographic factors and recurring mechanisms of injury
