Hepatitis B: Who should be treated?-managing patients with chronic hepatitis B during the immunetolerant and immunoactive phases
Miwa Kawanaka, Ken Nishino, Hirofumi Kawamoto, Ken Haruma
Abstract New hepatitis B virus (HBV) infections are decreasing owing to improved antiviral therapy and increased HBV vaccination worldwide; however, the number of HBV infections remains a major cause of liver carcinogenesis. HBV triggers cytotoxic immunity to eliminate HBV-infected cells. Therefore, the HBV pathophysiology changes in persistently infected individuals depending on host immune responses and HBV DNA proliferation state. To prevent liver cirrhosis and carcinogenesis caused by HBV, it is important to treat HBV infection at an early stage. Active treatment is recommended for the immunoactive hepatitis B surface-antigen-positive and -negative phase, but not during the immune-inactive phase or immune-tolerant phase; instead, follow-up is recommended. However,these patients should be monitored through regular blood tests to accurately diagnose the immune-inactive or -tolerant phases. The treatment regimen should be determined based on the age, sex, family history of liver cancer, and liver fibrosis status of patients. Early treatment is often recommended due to various problems during the immune-tolerant phase. This review compares the four major international practice guidelines, including those from the Japanese Society of Hepatology, and discusses strategies for chronic hepatitis B treatment during the immune-tolerant, immune-inactive, and resolved phases. Finally, recommended hepatitis B antiviral therapy and follow-up protocols are discussed.
Key Words: Hepatitis B; Immune tolerance; Immune-inactive; Anti-viral therapy;Hepatocellular carcinoma; Cirrhosis
INTRODUCTION
Chronic hepatitis B (CHB) is the leading cause of hepatocellular carcinoma (HCC), and it is estimated that 240 million individuals are persistently infected by the hepatitis B virus (HBV)[1 -4]. The prevalence of hepatitis B surface-antigen (HBsAg) is approximately 3 %-4 % worldwide; in addition, more than 880000 individuals die each year from HBV-derived liver damage[1 -4]. The high prevalence of hepatitis B in Asia and Africa is accompanied by high mortality, and infections in the Western Pacific region account for approximately 50 % of chronic HBV infections worldwide[1 ,5 ,6]. Therefore,prevention, diagnosis, evaluation, indication of treatment, and management of coinfected patients are important in these areas. HBV may exploit the immature neonatal immune system to establish a persistent infection. Following vertical or perinatal transmission, 90 % of neonates develop CHB, whereas children infected between 1 and 5 years of age have a 30 % chance of developing chronic infection. Studies on the natural history of HBV infection have shown that the timing of hepatitis B e-antigen(HBeAg) seroconversion varies from childhood to adulthood, with HBeAg seroconversion occurring primarily between 15 and 35 years of age[7 -9]. Natural HBeAg seroconversion has been reported to be 4 .6 %, 7 .1 %, and 28 % for those under 6 ,between 6 and 12 , and above 12 years of age, respectively[9]. Most patients with HBV can resolve their infections, but approximately 10 % continue to have viral activity,progress to cirrhosis at an annual rate of 2 % and develop HCC or liver failure[5 ,10 -14]. Since its discovery in 1965 , the gene structure and replication mechanism of HBV,its infection route, natural course, and pathophysiology have been clarified, and treatment methods have been advancing continuously. The timeline of HBV infection is complex and comprises various overlapping immune phases[2 ,3 ,10 ,13].
The European Association for the Study of Liver Disease (EASL), American Association for the Study of Liver Disease (AASLD), Asian-Pacific Association for the Study of the Liver (APASL), and the Japanese Society of Hepatology (JSG) have defined HBsAg loss as a CHB treatment goal[15 -18]. HBsAg loss is associated with improved clinical outcomes such as prevention of HCC and survival[19]. However,this endpoint is difficult to achieve with the existing antiviral therapies that include long-term nucleos(t)ide analog (NA) and pegylated interferon (Peg-IFN) therapies]. A recent study reported that a higher portion of patients showed HBsAg loss in response to combined treatment with tenofovir disoproxil fumarate (TDF) and Peg-IFN α-2 a for 48 wk than to TDF or Peg-IFN α-2 a monotherapy[20]. Therefore, NA and Peg-IFN combination therapies are being constantly used and developed to prevent cirrhosis and HCC[20 -22]. Several factors, such as the immune phase, genotype, race, degree of liver fibrosis, HCC family history[23 -25], age, and sex should be considered to determine the most efficient treatment for CHB. Moreover, the appropriate drug type and timing of drug administration are crucial[19 ,26]. CHB immune phases can be divided into five categories, including the immunotolerant phase, immunoactive HBeAg-positive phase, immune-inactive phase, immunoactive HBeAg-negative phase,and resolved CHB phase; each phase is identified according to immunological features, virology, biochemistry, and histology specific to the infection[3 ,5 ,7 ,13].Among these phases, phases 1 , 3 , and 5 are often not indicated for treatment, and instead, follow-up is often recommended[15 -18]. In any case, it remains uncertain whether follow-up is sufficient, especially for the immunotolerant phase.
CURRENT TREATMENT CONSIDERATIONS FOR HEPATITIS B PATIENTS
Indicators for initiating HBV treatment
The CHB treatment goals are to reduce liver disease mortality, improve survival, and enhance quality of life by preventing liver disease progression from fibrosis to cirrhosis and HCC. All global guidelines recommend initiating treatment based on the presence of HBV DNA and serum alanine aminotransferase (ALT) levels. Patients in either the immunoactive HBeAg-positive or -negative phase are likely to progress to cirrhosis and liver carcinogenesis. Considering the risk of developing cirrhosis and HCC associated with them, these phases are used as the main characteristics for initiating antiviral therapy[15 -18]. The following host indicators are also considered prior to treatment: Sex (male), age > 40 years, family history of HCC, place of birth(sub-Saharan Africa or Asia), presence of virus- or disease-related cirrhosis, HBV-DNA> 2000 IU/mL and elevated ALT levels, presence of HBeAg, and genotype C, which causes delayed HBeAg seroconversion[23 -28]. In patients treated using NA, HBsAg and HB core-related antigen (HBcrAg) levels are associated with HCC carcinogenesis,even at low levels of HBV DNA levels[29 -32]. Recently, modified PAGE-B scores,which are determined based on patient age, sex, baseline platelet count, and serum albumin levels were shown to predict HCC in patients receiving NA treatment[33].
The AASLD guidelines propose different HBV-DNA levels for antiviral therapy,depending on the HBeAg status[17]. According to the APASL guidelines, the HBV DNA levels considered for starting treatment depend on whether the patients are HBeAg-positive or -negative, regardless of the ALT levels[16]. In contrast, the EASL guidelines state that treatment determination should be based upon HBV-DNA and ALT levels, regardless of HBeAg status[15]. Furthermore, according to the JSG guidelines, an ALT level value of 31 or higher, which exceeds normal values in Japan,and HBV DNA levels ≥ 2000 IU/mL are indicated for antiviral treatment, regardless of the HBeAg status[18]. For HBV cirrhosis, antiviral treatment is recommended by all the global guidelines[15 -18] (Table 1 ).
Treatment indications for patients in the immune-tolerant phase
The first phase of CHB, the immune-tolerant phase, is characterized by minimal or no necroinflammatory activity, during which the risk of disease progression is minimal[8 ,34]; moreover, 90 % of patients infected in early childhood undergo seroconversion from HBeAg-positive to -negative at a young age, and the disease stabilizes in most cases[7 -9]. Thus, most clinical practice guidelines do not recommend antiviral therapy for these patients, and follow-up is recommended[15 -18]. Among these, the 2017 EASL guidelines[15] set the immune-tolerant phase as HBeAg-positive chronic HBV infection, and the treatment indications for the immune-tolerant phase are expanded compared to other guidelines. Furthermore, serum HBV DNA and HBsAg levels are associated with increased HCC risk and disease progression at serum ALT levels with or without HBeAg[26 ,27]. Early HBV treatment decreases mortality, improve transplantation outcomes, and decreases the risk of HCC[19]. Therefore, therapeutic intervention should be considered in cases of immune tolerance.
The HBV immune-tolerant phase exhibits high HBsAg and HBeAg titers, indicating high viral replication, and either normal or minimally elevated serum ALT levels. In this case, HBV proliferation is active but ‘tolerated’ as the host immune system does not recognize the viral antigen.
Table 2 presents the definition of immune tolerance and treatment guidelines[15 -18]. The ALT cutoff value during the immune tolerance phase depends on the global guidelines. The AASLD guidelines indicate cutoff values of 35 IU/L for men and 25 IU/L for women. The APASL and EASL guidelines set the cutoff at 40 IU/L, whereas the JSG guidelines recommend no treatment for ALT < 30 IU/L. High HBV DNA level cutoffs are important to distinguish immune-tolerant CHB from other phases. The HBV DNA criteria during the immune-tolerant phase differs between the EASL (≥2000 IU/mL), and the AASLD and APASL (≥ 20000 IU/mL for both). Moreover, the age limit for considering a liver biopsy or treatment in the immune-tolerant phase also depends on the guidelines: > 40 years old (both AASLD and JSG), > 35 years old(APASL), or > 30 years old (EASL). Furthermore, antiviral therapy is considered when ALT levels increase during monitoring. According to the AASLD guidelines, treatment is indicated for patients with liver fibrosis stage F2 or higher, especially for patients over 40 years of age. The EASL guidelines indicate treatment for patients with liverfibrosis stage F2 /A2 or higher (as determined using elastography and/or liver biopsy), over 30 years old, and who have liver stiffness of ≥ 12 kPa. The APASL guidelines simply recommend that patients with F2 /A2 or a higher score be considered for treatment. According to the JSG guidelines, determination of liver fibrosis (by liver biopsy or a non-invasive procedure) is recommended if the ALT level is intermittently elevated, HBV DNA is high, platelet counts are less than 15 × 104 /μL,and the patient is older than 40 years of age.
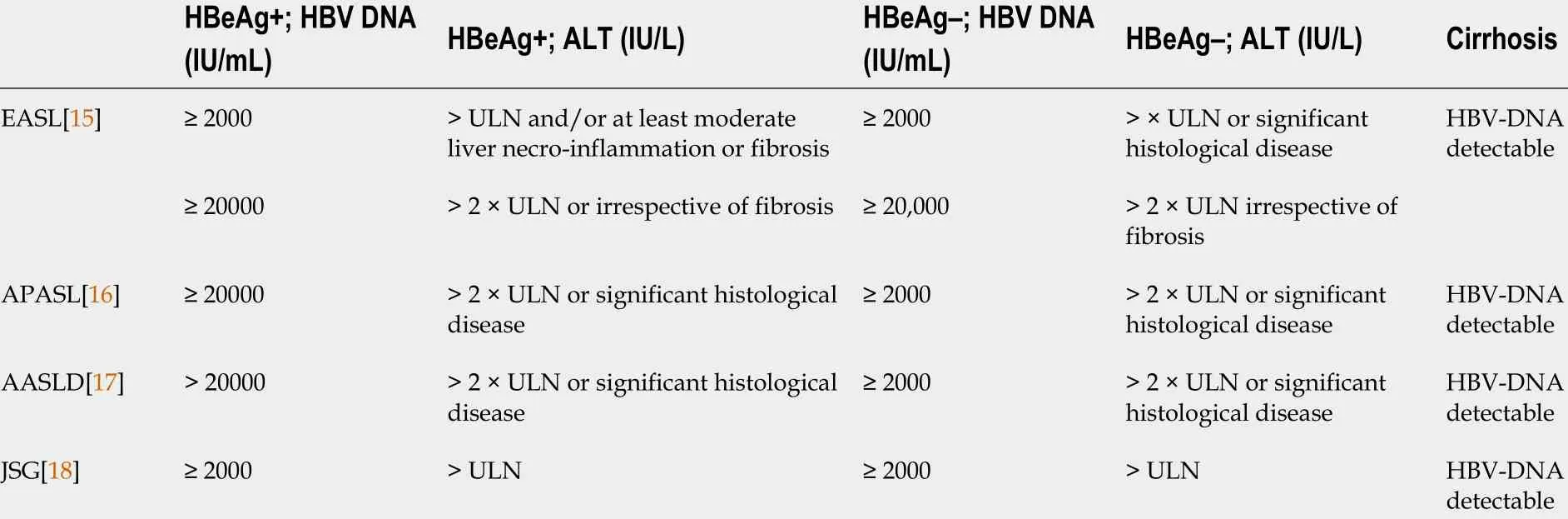
TabIe 1 Summary of treatment criteria for chronic hepatitis B
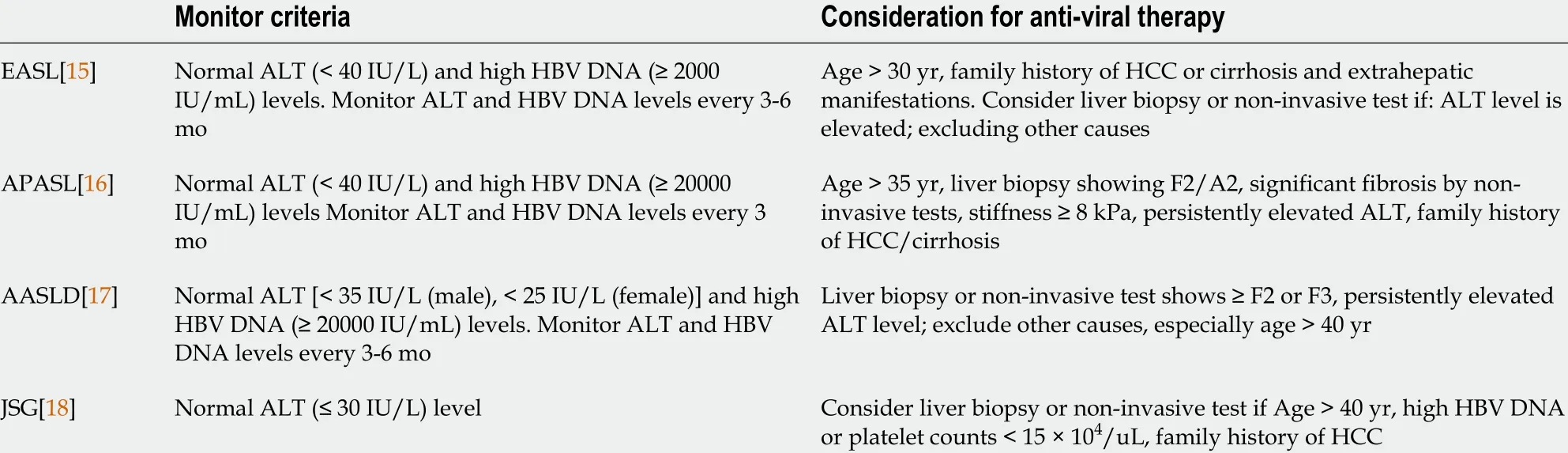
TabIe 2 Treatment indications for patients with hepatitis B e-antigen positive, aIanine aminotransferase < upper Iimit of normaI for chronic hepatitis B
To summarize the global guidelines: Age, family history of developing HCC or cirrhosis, and liver fibrosis are important factors for deciding the best therapeutic strategy during the immune-tolerant phase.
Arguments against treatment during the immune-tolerant phase
There are various opinions regarding the need to treat patients in the HBV immunetolerant phase. This phase is characterized by high viral replication, the presence of HBeAg, and normal or minimally elevated serum ALT and/or aspartate aminotransferase levels[3 ,5 ,10 ,13]. The immune-tolerant phase is usually identified in patients below 30 years of age. Very mild non-specific hepatitis has also been reported in patients in immune-tolerant phase who are between the ages of 10 and 12 years,although the 5 years progression of liver damage is minimal among patients who remain in the immune-tolerant phase[8 ,34].
Immune-active HBeAg-positive CHB that occurs in adolescence is associated with continued hepatitis activity. Some patients develop fibrosis or cirrhosis during the HBeAg-positive phase, but most show decreased serum HBV DNA levels and HBeAg seroconversion, resulting in an immunoactive HBeAg-negative CHB phase. This phase is characterized by persistent normal serum ALT levels and low HBV DNA load. Some patients show spontaneous HBeAg antibody positivity and may not require antiviral therapy. Patients who spontaneously show HBeAg seroconversion before the age of 30 years usually have a good prognosis[35 ,36]. In fact, approximately 90 % of patients will either be cured, or the hepatitis will not progress into adulthood. For instance, Tadaet al[35] examined 408 HBV carriers who did not receive NA and found that individuals under the age of 40 with HBeAg seroconversion had a better prognosis than those without HBeAg seroconversion, even when matched by sex and age.
Furthermore, the HBeAg seroconversion rate is very low even if antiviral treatment is administered during the immune-tolerant phase[37 -39]. Patients in the immunetolerant phase requires continuous NA treatment due to high HBsAg levels; moreover,the HBeAg seroconversion rate is low, and serum clearance of HBsAg is rarely achieved[19 ,39].
In another example, Chanet al[39] administered TDF or a combination of TDF and entecavir (ETV) to 126 HBeAg-positive patients with normal ALT levels, who were close to the immune-tolerant phase and found that only 5 % of patients receiving treatment showed HBeAg seroconversion. Although none of these cases were in the immune-tolerant phase, other reports have shown that HBeAg seroconversion is high in cases with elevated ALT levels[20]. In general, the higher the ALT level, the better the seroconversion. As ALT levels are naturally low during the immune-tolerant phase, HBeAg seroconversion is not expected.
Several patients in the HBV immune-tolerant phase are young and the NA treatment period is extensive. Treatment is also complicated by several factors,including the development of viral resistance, treatment cost, and long-term safety issues. Andreaniet al[8] also showed that patients with normal ALT levels and high HBV DNA (107 copies/mL) do not require liver biopsies as liver tissue-related changes are minimal during the immune-tolerant phase. In conclusion, there is little evidence to support that treatment alters the clinical outcome in these patients, though some guidelines recommend follow-up[40].
Recommendations for treating patients in the HBV immune-tolerant phase
Earlier, most clinical practice guidelines did not recommend antiviral therapy for patients in the immune-tolerant phase. However, it was recently reported that antiviral treatment during the immune-tolerant phase reduces the risk of HCC, liver transplantation, and death. Thus, some evidence supports antiviral therapy for patients in the immune-tolerant phase[41]. Studies have reported that increase in HBV DNA levels is a risk factor for cirrhosis and HCC[26 -28]; moreover, HBV infection itself may lead to HCC. Patients infected with HBV treated with antiviral NA therapy can achieve remarkable viral suppression[39 ,42]. Further, combined Peg-IFN and NA therapy is more effective in children who are in immune-tolerant phase than in adults[43 -45]. A randomized control study evaluated the usefulness of IFN with lamivudine combined therapy for naive HBV infection for patients in immune-tolerant phase, aged 1 -16 years, and the results showed reduced HBV DNA load, improved HBeAg seroconversion, and improved rate of HBsAg loss[45]. Management of hepatitis B in children has also been recently reported[46 ,47]. In fact, hepatitis B vaccination for infants and young children has markedly reduced HBV infections in the vaccinated younger generation, but a significant number of children are still infected with HBV.Most HBV infections in children are in a phase of immune tolerance, and therefore,many are followed up. Most chronically HBV-infected children have mild disease, but a small number may develop undetected fibrosis, cirrhosis, or HCC[47]. There are insufficient data to identify high-risk groups for HCC among children. In fact, children with HBV-associated HCC do not have cirrhosis and have normal alfa-fetoprotein levels, which should be considered for the duration of follow-up and indications for treatment[48].
In recent years, advances in understanding the immunopathogenicity of CHB have questioned whether treatment should be administered at an early stage of CHB regardless of ALT level or severity of liver disease. The immune-tolerant phase is not associated with immunological tolerance, and the results question whether good follow-up as benign is good[49].
Antiviral therapy may also suppress the risk of disease spread from patients with hepatitis B to other individuals. Indeed, antiviral therapy reduces the risk of horizontal transfer of HBV infection from immunotolerant patients with very high viral load, as well as vertical HBV transmission by mothers with high viral load. Cases without hepatitis B immune globulin and a vaccine occur almost exclusively in HBeAg-positive women with high HBV DNA levels (> 200000 IU/mL) and HBsAg levels exceeding 4 -4 .5 logs/mL. Mother-to-child HBV transmission rates (MTCTs) were 0 % in HBsAgpositive pregnant patients showing high HBV DNA levels (> 200000 IU/mL), who were treated with TDF at 28 gestational weeks[50]. In a meta-analysis based on 595 articles, the administration of antiviral drugs during pregnancy, especially TDF, was deemed safe in helping prevent MTCTs[51 ,52]. In addition to TDF, tenofovir alafenamide fumarate is administered to pregnant women at 24 -35 wk gestation, and the safety of the pregnant women and infants as well as the prevention of MTCT were reported recently[53].
The WHO advocates administration of TDF to infected pregnant women with high HBV load (≥ 5 .3 log 10 IU/mL; or ≥ 200000 IU/mL) from the 28thweek of pregnancy till delivery. This treatment regimen is recommended to prevent MTCT. The WHO also suggests three hepatitis B vaccinations for newborns, including one dose at birth[54].
Standard follow-up of the immune-tolerant phase may not identify the transition to the immunoactive phase. Thus, evaluating the progression of liver fibrosis and liver carcinogenesis during follow-up is important.
Challenges associated with immune-tolerant phase-diagnosis, liver fibrosis, and liver carcinogenesis
Liver damage caused by HBV causes hepatocellular regeneration associated with chronic necrotizing inflammation, which leads to HCC. The onset of HCC in HBV may arise from immunopathogenic factors[11 ,55]. In addition, adult serum ALT levels and HBV DNA levels are associated with liver carcinogenesis. Active HBV DNA replication is strongly associated with HCC development and cirrhosis, regardless of ALT levels[26 -28 ,56]. The cumulative incidences of HCC and liver-related diseases in patients who have been in the immune-tolerant phase for over 10 years is 2 .7 % and 12 .7 %, respectively[41]. Lee et al[57] examined the cumulative HCC risk over a 10 -year period in immunologically active patients who achieved a virological response with antivirals in comparison with that in untreated patients in immune-tolerant phase.Surprisingly, the HCC risk was similar between these two groups of patients. In this study, the immune-tolerant phase was diagnosed by regular blood chemistry tests and serum HBV DNA tests every 3 -6 mo. Additionally, liver stiffness measured by transient elastography was used to strictly determine whether patients were in the immune-tolerant phase. Thus, this report indicates that HCC carcinogenesis is as high during the immune tolerance period as in the immunologically active phase.
To clarify these points, it is important to determine whether the subject is truly in the immune-tolerant phase. One study found significant fibrosis in 60 % of patients with a high viral load and normal or slightly elevated serum ALT for at least 12 mo[58]. Another study found that 37 % of HBeAg-positive patients aged 35 years or above, with ALT greater than 0 .5 × ULN, had progressive fibrosis, as assessed by transient elastography[59]. Therefore, patients with normal ALT levels and high HBV DNA levels are more likely to be immune-tolerant, subject to the status of their liver fibrosis status[60].
Patients with ALT and HBV DNA greater than 10 ,000 copies/mL should be carefully evaluated and monitored, even if they appear normal. Necrotic inflammation of the liver and/or fibrosis is observed or progresses unnoticed in certain cases, even in patients with persistently normal ALT levels[56 ,59 -61]. Serum ALT levels cannot be used as a surrogate marker for hepatocyte damage to assess the severity of hepatitis activity.
For this reason, the 2017 EASL guidelines renamed this phase to “HBeAg-positive chronic HBV infection” instead of the “immune tolerance phase,” to avoid confusion and the need for early treatment[15]. The AASLD guidelines suggest that ALT levels should be tested every 6 mo at least, even if the patient is in the “immune-tolerant phase,” to monitor the potential for progression to “immunoactive or immune-inactive phase”[17]. Various global guidelines recommend regular evaluation of ALT level and HBV DNA load every 3 -6 mo in patients who are in the immune-tolerant phase(Table 3 ). A previous study showed that 4 .6 % children (up to 12 years of age) progress from the immune tolerance to the immunoclearance phase; therefore, it may be helpful to evaluate ALT levels and HBV DNA load once every 6 -12 mo in such children[9].
To diagnose the immune tolerance period accurately, constant monitoring of HBsAg levels, HBeAg levels, and HBV DNA, and ALT levels is required. Chanet al[62]performed transient elastography on 161 patients with HBV infection and determined liver stiffness cutoffs associated with normal and elevated ALT levels (> 1 -5 -foldULN). These patients were divided into reassurance, observation, liver biopsy, and treatment consideration groups; notably, 58 % and 62 % of patients with normal and elevated ALT levels (> 1 -5 times ULN), respectively, did not require a liver biopsy. In addition to measuring HBsAg, ALT levels, HBV DNA load, and liver fibrosis should be constantly monitored to diagnose true immune tolerance. Recently, non-invasive diagnostic methods for diagnosing fibrosis, such as transient elastography, and markers for liver fibrosis have been developed[63 ,64]. These methods must be used to accurately diagnose HBV and develop future policies for clinical management of patients with HBV infection.
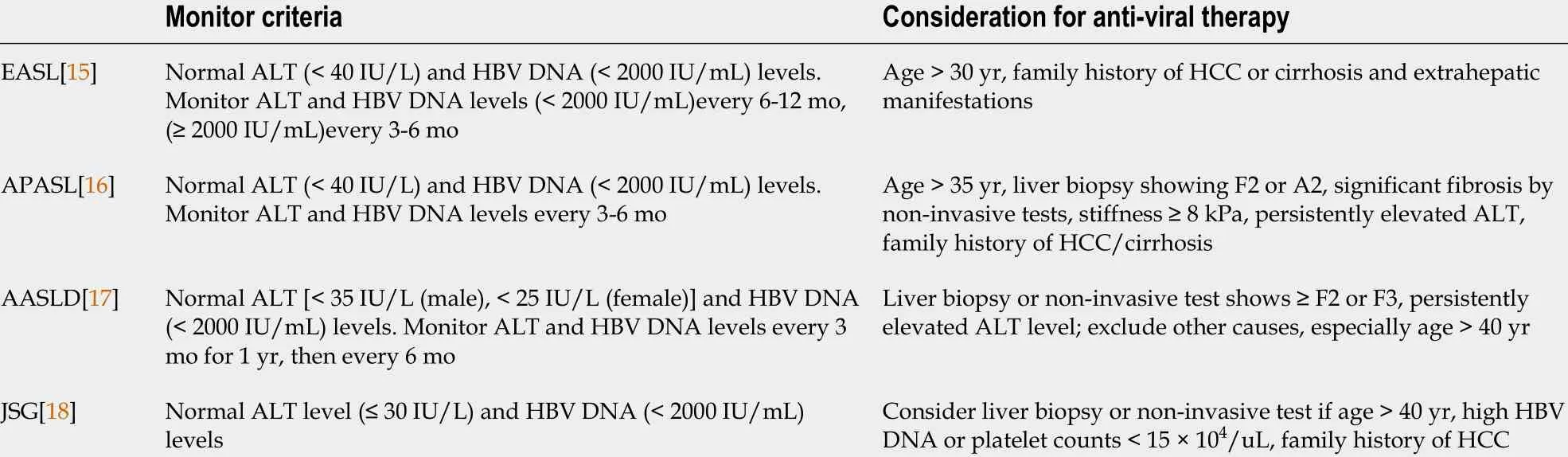
Table 3 Treatment indications for patients in the hepatitis B e-antigen-negative immune-inactive phase
Antiviral treatment during the immune-inactive phase
The third phase of CHB, which is the immune-inactive phase, is characterized by low HBV DNA load (usually < 2000 IU/mL) and ALT levels within the normal range.HBeAg seroconversion often reduces hepatitis symptoms, however, in 20 %-30 % of these patients, HBV re-proliferates, hepatitis relapses, and the third immunoactive HBeAg phase transitions into the immune-negative phase. When HBV does not repopulate, it leads to a decrease in HBV DNA load as well as reduction in HBsAg;then, CHB progresses to the HBsAg-negative resolved phase[2 ,5 ,7 ,13]. JSG guidelines define the immune-inactive phase (phase 3 ) when the patient is HBeAg negative at least three times over 1 -year follow-up period, with HBV DNA levels < 2000 IU/mL,and ALT ≤ 30 IU/L. This guideline is based on the fact that histologically favorable liver disease is rare when HBeAg is negative three or more times during follow-up for 1 year or more. In this case, HBV DNA is usually < 2000 IU/mL and ALT is typically <40 IU/L. Although liver biopsy is not required at this time, lifelong monitoring is indeed required. However, even under these conditions, patients with advanced fibrosis are at increased risk of liver carcinogenesis. Thus, treatment should be considered if liver fibrosis is suspected as recommendedperthe AASLD, EASL, and APASL guidelines. During this phase, antiviral treatment is recommended if the patient has a family history of HCC or cirrhosis or if significant histological findings are noted on the liver biopsy. Thus, in this phase, age, family history of cirrhosis and HCC, and fibrosis progression are important factors for consideration.
Loss of HBsAg is an ideal endpoint and antiviral therapy during the immuneinactive phase may promote HBsAg clearance and lead to low HBsAg levels. The annual incidence of HCC and liver-related deaths among patients in this phase are higher and this trend may be reduced by antiviral treatment. However, treatment should be carefully considered, as chances of HBsAg loss can still increase naturally during the immune stage compared to other stages. It is also believed that antiviral treatment is not necessary and should only be considered in exceptional circumstance.If antiviral treatment is provided, the administration time during the immune-inactive period will be shorter than that during the immune tolerance period.
Need for treatment in the resolved phase of CHB
In the resolved phase of CHB, the patient tests negative for HBsAg, HBV DNA is not detected, ALT level is normalized, and liver inflammation disappears. This condition is the goal of hepatitis B treatment and no longer requires NA therapy. However, in cases where treatment is initiated with NA(s), AASLD guidelines recommend that patients consider discontinuing treatment when HBsAg is negative, and cirrhosis is absent[20]. The EASL guidelines may consider long-term (i.e., 3 years or longer) NA treatment after the loss of HBsAg, with or without HBsAg positivity. However, the EASL guidelines do not consider cirrhosis at this stage[15]. The APASL guidelines recommend treatment discontinuation if HBsAg level decreases, antibody reversal is observed, and HBV DNA is not detected for at least two years at three separate followup visits every six months. Nevertheless, it is recommended that lifelong NA therapy be continued for patients with cirrhosis[16]. Although the JSG guidelines also set criteria for discontinuing NA therapy based on HBsAg levels and HBcrAg[18],treatment discontinuation in the resolved CHB phase is not specified. However, for liver cirrhosis, relapse after discontinuation of NA treatment has a risk of inducing liver failure; therefore, treatment is generally continued lifelong.
If HBsAg is absent, treatment discontinuation remains an option; however, this is not recommended since results on the long-term prognosis of patients with discontinued treatment are currently unavailable. Thus, further therapy is not required if the HBsAg test yields negative results; however, indefinite treatment is recommended for patients with liver cirrhosis.
CONCLUSION
In summary, hepatitis B should be followed up or treated according to the hepatitis B disease course. Toward that end, the treatment selection, as well as mode and timing of drug administration are important for improving HBV prognosis. It is necessary to determine whether patients are in the immune-tolerant or immune-inactive phase to recommend appropriate follow-up and assess their need for antiviral therapy.Furthermore, a major consideration during the course of HBV treatment is to determine the true extent of immune inactivity and immune resistance, for which it is necessary to devise non-invasive evaluation of continuous ALT and HBV DNA level changes, and liver fibrosis. In addition, it is important to consider clinically relevant factors such as age, sex, and genotype during the treatment decision-making process.The option of early treatment also needs to be discussed during the immune tolerance stage. As these factors are not yet clarified in the global guidelines, future research is warranted to elucidate treatment options and prognosis according to the cirrhosis and HCC risk profiles of HBV-infected patients.
ACKNOWLEDGEMENTS
Thanks for Masayuki Kurosaki at Misasino Red Cross Hospital, Tokyo, Japan.
 World Journal of Gastroenterology2021年43期
World Journal of Gastroenterology2021年43期
- World Journal of Gastroenterology的其它文章
- Survivin-positive circulating tumor cells as a marker for metastasis of hepatocellular carcinoma
- Minimum sample size estimates for trials in inflammatory bowel disease: A systematic review of a support resource
- Immunoglobulin G in non-alcoholic steatohepatitis predicts clinical outcome: A prospective multi-centre cohort study
- Genome-wide map of N6 -methyladenosine circular RNAs identified in mice model of severe acute pancreatitis
- Liver injury changes the biological characters of serum small extracellular vesicles and reprograms hepatic macrophages in mice
- Recent advances in artificial intelligence for pancreatic ductal adenocarcinoma
