缓解期狼疮性肾炎患者小剂量激素和羟氯喹治疗下对计划妊娠结局及肾脏损害的影响
宁莉 王健 赵颖 姚琴 温华英
[關键词] 缓解期;狼疮性肾炎;小剂量激素;羟氯喹;计划妊娠结局;肾脏损害
[中图分类号] R692.3 [文献标识码] B [文章编号] 1673-9701(2021)18-0054-03
Effects of low-dose hormone and hydroxychloroquine on planned pregnancy outcome and renal injury in patients with lupus nephritis in remission
NING Li1 WANG Jian2 ZHAO Ying3 YAO Qin1 WEN Huaying1
1.Department of Obstetrics and Gynecology, the First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, China; 2.Department of Nephrology, the First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, China; 3.Department of Reproductive Medicine, the First Affiliated Hospital of Gannan Medical University,Ganzhou 341000, China
[Abstract] Objective To observe the influence of planned pregnancy on maternal safety and pregnancy outcome of patients with lupus nephritis (LN) in remission under the maintenance treatment of low-dose hormone and hydroxychloroquine, and to investigate the pregnancy time and drug use of LN patients. Methods A total of 23 patients with LN in remission were treated with low-dose prednisone (10 mg/day) and hydroxychloroquine (400 mg/ day) in our hospital from January 2013 to December 2018, and their pregnancy was planned under the guidance of obstetricians, reproductive medicine doctors and nephrologists. The general condition during pregnancy, blood and urine test results, Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score, fetal development and delivery were recorded. Results 1.There were 29 pregnancies and 6 spontaneous abortions in 23 patients,and 2 patients terminated their pregnancy due to severe lupus activity and preeclampsia in the second trimester of pregnancy. The abortion rate was 20.69%. The pregnancy success rate was 91.30% and the premature birth rate was 19.05%. There was no stillbirth, and the fetus developed well. 2.Before delivery,SLEDAI score and urine total protein of all patients were higher than those before pregnancy, with statistically significant difference(P<0.05). And the plasma albumin was lower than that before pregnancy, without statistically significant difference(P>0.05). The recurrence rate of nephritis was 43.47%, and the incidence of nephrotic syndrome was 21.74%. Conclusion LN patients in remission planning pregnancy with low dose of hormone and hydroxychloroquine can have a good control of the lupus activity and nephritis, and obtain satisfactory pregnancy outcome.
[Key words] Remission; Lupus nephritis; Low dose hormone; Hydroxychloroquine; Planned pregnancy outcome; Renal injury
系统性红斑狼疮(Systemic lupus erythematosus,SLE)是一种多系统受累的自身免疫性疾病,常见于年轻女性,其病程具有周期性缓解和复发的特点。狼疮性肾炎(Lupus nephritis,LN)是SLE的常见并发症,其发生率为50.7%[1],表现为蛋白尿、血清肌酐升高、高血压、血小板减少、贫血等。随着对疾病认识的深入和越来越多的青年狼疮性肾炎患者对于生育的渴望,提高狼疮性肾炎患者的安全妊娠成功率是近年来备受关注的研究内容。研究表明妊娠会增加SLE加重的风险,尤其是妊娠前病情未控或孕期病情活动者[2-3]。对于狼疮性肾炎稳定期患者在维持小剂量激素及羟氯喹治疗下,计划妊娠的安全性及妊娠结局报道较少。基于此,本研究选取我院2013年1月至2018年12月诊断为狼疮性肾炎且治疗后处于缓解期的计划妊娠妇女,在产科、生殖医学科及肾内科指导下用药及密切监测,研究妊娠结局及药物的安全性,为LN患者妊娠提供临床证据,现报道如下。
1 资料与方法
1.1 一般资料
选取2013年1月至2018年12月经我院诊断为狼疮性肾炎的青年女性患者23例,年龄21~32岁,平均(26.43±2.97)岁;病程2.82~7.15年,平均(4.41±1.19)年。纳入标准:①妊娠前病情稳定,无明显狼疮活动,系统性红斑狼疮的活动指数(SLEDAI)积分≤4分,且停用免疫抑制剂或胎儿致畸药物6个月以上;②24 h尿蛋白<1 g以下,血清肌酐<100 μmol/L;③糖皮质激素剂量≤10 mg/d,羟氯喹片剂量≤400 mg/d;④血压控制良好,<140/90 mmHg。排除标准:①狼疮性肾炎非计划怀孕者;②抗磷脂抗体阳性者;③合并其他系统疾病可威胁妊娠安全,如精神疾病、心脏疾病、凝血功能障碍、肿瘤、合并感染等。
1.2 方法
所有患者继续服用泼尼松片和羟氯喹片。泼尼松(上海信谊药厂有限公司,国药准字H31020675,规格:5 mg/片)1次/d,10 mg/次;羟氯喹片(上海上药中西制药有限公司,国药准字H19990263,规格:100 mg/片)2次/d,200 mg/次。有高血压者继续服用无致畸作用的降压药物,同时在生殖科医生指导下助孕,孕后需完成产科常规检查,每月定期检查尿分析、尿总蛋白、血液常规、肝肾功能电解质血糖、补体、血沉等检查。
1.3 观察指标及评价标准
观察患者妊娠、胎儿分娩及发育情况(流产率、妊娠成功率、早产率、出生孕周及婴儿发育情况),及狼疮活动和肾脏损害程度。①狼疮活动:根据患者临床表现及相关辅助检查结果计算妊娠前后系统性红斑狼疮的活动指数(SLEDAI)积分,0~4分基本无活动、5~9分轻度活动、10~14分中度活动、≥15分重度活动[4]。②肾脏损害程度评估:观察孕前及分娩前24 h尿总蛋白、血浆白蛋白、血清肌酐值变化,计算肾炎的复发率(尿总蛋白量>2 g)、肾病综合征发生率。留取24 h尿液,混匀后取尿液5 mL,并测量总尿量,送检我院检验科尿液分析仪检测计算尿总蛋白。抽取清晨空腹外周血5 mL送我院检验科,使用全自动生化分析仪(Cobas 8000-701)检测血浆白蛋白、血清肌酐,血液分析仪(SYSMEX XN-2000)检测血常规。
1.4 病情变化及处理
1.4.1 根据SLEDAI积分处理 ①狼疮轻度活动者:观察或据病情加大激素用量或酌情加用环孢素控制病情;②狼疮中度活动者:增加激素用量并加用环孢素,必要时终止妊娠;③狼疮重度活动者:增加激素用量并加用环孢素治疗,必要时激素或丙种球蛋白冲击治疗,据病情终止妊娠。
1.4.2 其他并发症处理 妊娠期常见并发症,如合并高血压、妊娠期糖尿病、先兆流产、妊娠晚期出血、多胎妊娠、巨大胎儿、羊水量异常、胎儿的发育异常及死胎、胎儿窘迫及胎膜早破等,由产科医师按诊疗常规处理。妊娠期若合并其他内科及外科疾病,请相关科室会诊后按诊疗规范积极处理。
1.5 统计学方法
采用SPSS 24.0统计学软件处理数据。计量资料以(x±s)表示,采用t檢验。P<0.05为差异有统计学意义。
2 结果
2.1 妊娠、胎儿分娩及发育情况
共23例患者妊娠29次,其中6次自然流产,流产率为20.69%(6/29)。2例患者妊娠中期出现狼疮活动,表现为肾病综合征、肌酐升高,伴有高血压、头痛先兆子痫而中途终止妊娠。完成妊娠的21例患者中,3例中晚期出现狼疮活动及肾病综合征,给予增加激素剂量、加用环孢素、补充白蛋白及对症治疗,后病情控制,其中早产结束妊娠2例,无畸形及重大疾病。其余18例中早产2例,足月妊娠16例,胎儿均存活,无畸形及重大疾病。23例患者中成功妊娠21例,妊娠成功率为91.30%,早产率为19.05%(4/21),成功分娩孕龄为(37.81±1.72)周。
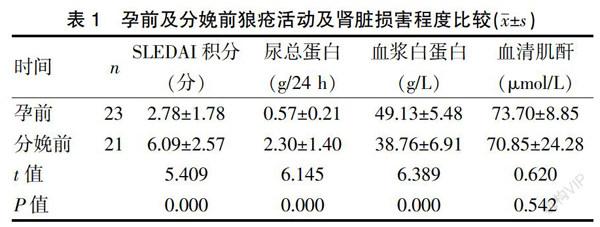
2.2 孕前及分娩前狼疮活动及肾脏损害程度比较
分娩前SLEDAI积分、尿总蛋白高于孕前,血浆白蛋白低于孕前,差异有统计学意义(P<0.05);分娩前血清肌酐均值略低于孕前,但差异无统计学意义(P>0.05)。见表1。10例患者因尿总蛋白量增加>2 g,增加了激素用量或加用了环孢素治疗,肾炎的复发率(尿总蛋白量>2 g)43.47%(10/23);5例患者表现为肾病综合征,发生率为21.74%(5/23)。
3 讨论
有研究发现,SLE活动期患者血清中大量免疫复合物及补体在胎盘沉积,血管内皮细胞受损,并激发凝血系统形成局部微血栓,导致管壁增厚,管腔狭窄,造成胎盘绒毛发育不良,影响交换功能,使胎儿供养减少,发生胎儿宫内生长受限甚至胎死宫内[5]。狼疮性肾炎为SLE患者妊娠SLE活动进展的独立危险因素[6-7],荟萃分析显示,SLE患者中狼疮性肾炎明显增加了不良妊娠结局和增加药物使用的风险[8]。狼疮性肾炎患者的药物治疗对于妊娠减少狼疮活动及并发症十分重要,但需考虑对胎儿的安全性[9]。钙神经素拮抗剂(环孢素、他克莫司)、抗代谢药物(硫唑嘌呤)是目前认为是相对安全的免疫抑制剂,而核苷酸合成抑制剂(环磷酰胺、甲氨蝶呤、环孢素、来氟米特等)在妊娠患者中被列为禁忌用药,已有临床研究显示该类药物有潜在的致畸作用[10-11]。羟氯喹在SLE合并妊娠患者中的宫内暴露效应,胎儿畸形率与普通人群无明显差异,且SLE孕期时间更长、复发率更低,糖皮质激素用量降低趋势[12]。妊娠期大剂量应用糖皮质激素可增加子痫前期、子宫胎盘功能减退、胎膜早破及糖耐量减低和感染的风险,同时可能导致新生儿肾上腺功能不全,而小剂量应用(5~10 mg/d)相对安全。
本研究选择狼疮性肾炎缓解期患者且继续服用小剂量激素和羟氯喹妊娠观察,结果显示胎儿的自然流产率为20.69%、早产率为19.05%及不成功妊娠率为8.70%,且无死胎及畸形等情况,低于Smyth等[13]研究报道,提示狼疮性肾炎缓解期患者使用小剂量激素和羟氯喹治疗下计划妊娠可提高妊娠成功率和妊娠质量。本研究结果显示,分娩前SLEDAI积分、尿总蛋白高于孕前,血浆白蛋白低于孕前,差异有统计学意义(P<0.05);分娩前血清肌酐略低于孕前,但差异无统计学意义(P>0.05);其中10例患者因尿总蛋白量增加>2 g,增加了激素用量或加用了环孢素治疗,肾炎的复发率(尿总蛋白量>2 g)43.47%,低于报道的复发率(50.7%)[1];5例患者表现为肾病综合征,发生率为21.74%。虽孕后患者整体上SLEDAI积分增加至轻度活动,43.47%的患者的尿总蛋白量明显增加,但表现为肾病综合征的发生率并不高,提示小剂量激素及羟氯喹方案下妊娠,狼疮活动及肾炎控制情况良好,为成功妊娠奠定了基础。Raimbourg等[14]认为,尽管妊娠可诱发狼疮活动,但如果将妊娠安排在最低风险期间且在治疗前后过程进行多学科密切监测,妊娠一般是成功和安全的。本研究结果显示,虽然妊娠增加狼疮活动,但在狼疮缓解期妊娠是可以获得活动良好的妊娠结局,与Raimbourg等[14]观点是一致的。
结合Bramham[15]及Naseri等[2]研究报道,狼疮性肾炎患者妊娠时机应为计划妊娠,狼疮性肾炎稳定缓解期,且停用免疫抑制及其他可能致畸药物至少半年,肌酐<100 μmol/L,尿蛋白<0.5 g/24 h,血壓≤140/90 mmHg。LN患者除了妊娠时机的选择及妊娠期的维持治疗外,妊娠期应密切进行定期产前检查,观察孕妇血压、体重指数、宫高、腹围的变化[16];还要定期监测各项血生化指标及相关免疫学指标的动态变化,评估SLE的活动程度,及时调整治疗方案。同时加强胎儿监护,如胎儿B超、胎儿心电图和超声心动图检查。若出现严重并发症危及母体健康,应及时终止妊娠。
综上所述,缓解期狼疮性肾炎患者维持小剂量激素和羟氯喹治疗下计划妊娠,狼疮活动及肾炎控制情况良好,可以获得较满意妊娠结局。本研究也存在不足,如样本量少、无婴幼儿长期随访情况等。
[参考文献]
[1] Koh JH,Ko HS,Lee J,et al. Pregnancy and patients with preexisting lupus nephritis:15 years of experience at a single center in Korea[J]. Lupus,2015,24(7):764-772.
[2] Naseri EP,Surita FG,Borovac-Pinheiro A,et al. Systemic lupus erythematosus and pregnancy:A single-center observational study of 69 pregnancies[J]. Rev Bras Ginecol Obstet,2018,40(10):587-592.
[3] Nahal SK,Selmi C,Gershwin ME. Safety issues and recommendations for successful pregnancy outcome in systemic lupus erythematosus[J]. J Autoimmun,2018,93:16-23.
[4] Gladman DD,Iba?觡ez D,Urowitz MB. Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol,2002,29(2):288-291.
[5] Ostensen M,Clowse M. Pathogenesis of pregnancy complications in systemic lupus erythematosus[J]. Curr Opin Rheumatol,2013,25(5):591-596.
[6] Saavedra MA,Cruz-Reyes C,Vera-Lastra O,et al. Impact of previous lupus nephritis on maternal and fetal outcomes during pregnancy[J]. Clin Rheumatol,2012,31(5):813-819.
[7] Fatemi A,Fard RM, Sayedbonakdar Z, et al. The role of lupus nephritis in development of adverse maternal and fetal outcomes during pregnancy[J]. Int J Prev Med,2013, 4(9):1004-1010.
[8] Wu J,Ma J,Zhang WH,et al. Management and outcomes of pregnancy with or without lupus nephritis:A systematic review and meta-analysis[J]. Ther Clin Risk Manag,2018, 14:885-901.
[9] Parikh SV,Almaani S,Brodsky S,et al. Update on lupus nephritis: Core curriculum 2020[J]. Am J Kidney Dis,2020,6386(19):31170-31179.
[10] Kalok A,Abdul CR,Indirayani I,et al. Pregnancy outcomes in systemic lupus erythematosus (SLE) women[J]. Horm Mol Biol Clin Investig,2019,40(3):/j/hmbci.
[11] Webster P,Wardle A,Bramham K,et al. Tacrolimus is an effective treatment for lupus nephritis in pregnancy[J]. Lupus,2014,23(11):1192-1196.
[12] Kroese SJ,de Hair M,Limper M,et al. Hydroxychloroquine use in lupus patients during pregnancy is associated with longer pregnancy duration in preterm births[J]. J Immunol Res,2017,2017:2810 202.
[13] Smyth A,Oliveira GH,Lahr BD,et al. A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis[J]. Clin J Am Soc Nephrol,2010,5(11):2060-2068.
[14] Raimbourg Q,Daugas ■. Lupus nephritis[J]. Nephrol Ther,2019,15(3):174-189.
[15] Bramham K,Soh MC,Nelson-Piercy C. Pregnancy and renal outcomes in lupus nephritis:An update and guide to management[J]. Lupus,2012,21(12):1271-1283.
[16] Lateef A,Petri M. Systemic lupus erythematosus and pregnancy[J]. Rheum Dis Clin North Am,2017,43(2):215-226.
(收稿日期:2020-09-17)