药物涂层球囊治疗冠状动脉支架内再狭窄和小血管病变的临床疗效
徐海 何非 张艳梅 许邦龙


[關键词] 药物涂层球囊;药物涂层支架;支架内再狭窄;小血管病变;主要不良心血管事件
[中图分类号] R541.4 [文献标识码] A [文章编号] 1673-9701(2021)18-0019-04
Clinical efficacy of drug-coated balloon in treatment of coronary artery in-stent restenosis and small vessel disease
XU Hai HE Fei ZHANG Yanmei XU Banglong
Department of Cardiology, the Second Affiliated Hospital of Anhui Medical University, Hefei 230601, China
[Abstract] Objective To investigate the clinical efficacy of drug-coated balloon (DCB) in the treatment of coronary artery in-stent restenosis (ISR) and small vessel disease. Methods Forty-eight patients with coronary heart disease admitted to our hospital for DCB treatment from January 2018 to October 2019 were selected for retrospective analysis, with 22 patients with ISR and 26 patients with small vessel disease. Forty-eight patients with the same gender, diseased blood vessel and type, age, and underlying disease who were treated with drug-eluting stent (DES) were selected as the control group. The primary endpoints were the cardiac death, non-fatal acute myocardial infarction (AMI), target lesion revaseularization (TLR) and other major adverse cardiac events (MACE). The reexamination results of coronary angiography or coronary CT were recorded. Results The average follow-up time was (9.15±5.46) months. The incidence of MACE in the DES group was 8.34%, which was higher than that of (4.17%) in the DCB group , with no statistically significant difference (P>0.05). There was no cardiac death in the two groups. There was no non-fatal AMI in the DCB group, and one non-fatal AMI (2.08%) in the DES group, with no statistically significant difference between the two groups(P>0.05). The number of TLRs undergone in the DCB group was 2 (4.17%), which was lower than that of 4 (8.34%) in the DES group, with no statistically significant difference (P>0.05). In the DCB group at (9.24±4.02) months, 19 patients had reexamination of coronary angiography and 4 had reexamination of coronary CT, among whom 10 patients were with ISR (1 patient with 85% vascular stenosis), 13 patients were with small vessel disease (1 patient with 90% vascular stenosis). In the DES group at (8.34±5.28) months, 14 patients had reexamination of coronary angiography, among whom 6 patients were with ISR (1 patient with 80% vascular stenosis), and 8 patients were with small vessel disease (1 patient with 99% vascular stenosis as non-fatal AMI, and 2 patients with 75% and 80% vascular stenosis, respectively). Survival curve analysis showed that there was no significant difference in the MACE-free survival rate between the two groups during the follow-up period (P=0.406). Conclusion The clinical efficacy of drug-coated balloons is not inferior to that of drug-eluting stent in the treatment of coronary artery in-stent restenosis (ISR) and small vessel disease. It can be used as an important strategy for clinical coronary revascularization.
[Key words] Drug-coated balloon; Drug-eluting stent; In-stent restenosis; Small vessel disease; Major adverse cardiac event
经皮冠状动脉介入治疗(Percutaneous coronary intervention,PCI)作为目前经典治疗冠心病手段取得了巨大的进展,从冠状动脉腔内成形术(Percutaneous transluminal coronary angioplasty,PTCA)到金属裸支架(Bare metal stent,BMS)再到药物洗脱支架(Drug eluting stent,DES),极大地改善了冠心病患者的生活質量。但支架植入也带来了新的问题,如DES导致的血管内皮愈合延迟、支架内再狭窄(In-stent restenosis,ISR)和支架内血栓形成等[1],小血管病变植入支架后易发生管腔丢失和远期再狭窄[2]。药物涂层球囊(Drug-coated balloon,DCB)作为冠脉介入治疗的一项创新技术,因其仅输送抗平滑肌细胞增殖药物,无金属置入物且术后双联抗血小板治疗时间短、并发症少等特点,为冠心病的治疗提供了新的方法。基于此,DCB得到了中外指南和共识推荐[3-5],并将DCB治疗ISR列为ⅠA类推荐,但其在中国人群中的应用相关报道并不多见,且在小血管病变中的疗效并不确切。因此本研究搜集和随访我院使用DCB治疗ISR和小血管病变的患者48例,并得到部分患者复查冠脉造影和冠脉CT的结果,希望进一步说明DCB在我国人群中治疗ISR和小血管病变的疗效,现报道如下。
1 资料与方法
1.1一般资料
回顾性分析2018年1月至2019年10月入住我院行DCB治疗的冠心病患者48例,其中ISR 22例,小血管病变26例。另选取性别、病变血管及类型相同且年龄、合并基础疾病等相近的行DES治疗患者48例作为对照组。纳入标准:①成年男性或未孕女性;②临床有胸闷、胸痛等心肌缺血表现且冠状动脉造影见靶血管病变狭窄超过70%的冠心病确诊病例[6],血管类型为ISR、小血管病变;③靶血管直径≥2 mm,小血管病变定义为血管直径≤2.75 mm;④预计寿命>1年。排除标准:①靶血管严重钙化或扭曲,不适合使用球囊扩张的病变者;②伴有严重心力衰竭症状不能平卧者或左心室射血分数(Left ventricular ejection fraction,LVEF)<35%者;③严重肝肾功能不全者;④有严重出血倾向或抗血小板药和抗凝药使用禁忌证者等;⑤合并恶性肿瘤或其他严重疾病,预计寿命<1年者。所有患者均签署手术知情同意书。
1.2 方法
DCB组行冠脉造影确定病变部位后使用传统或半顺应性球囊预扩张,球囊/血管直径比率0.8~1.0,确认无血管夹层或仅限于A、B型夹层(NHLBI分型),TIMI血流Ⅲ级且残余狭窄<30%[3],经指引导丝送入DCB(Se Quent Please,B. Braun Melsungen AG,Germany)覆盖预处理部位长度并超出边缘各2~3 mm,定位完成后扩张30~60 s。若术中出现C型及以上夹层,则补救性植入DES。术后均服用阿司匹林100 mg/d(Bayer S.p.A,国药准字 J20130078,规格:100 mg/片)、氯吡格雷75 mg/d(Sanofi Winthrop Industrie,国药准字 J20180029,规格:75 mg/片)或替格瑞洛90 mg/bid(AstraZeneca AB,国药准字J20171077,规格:90 mg/片),持续1~3个月,其他治疗药物及额外抗血小板治疗时间由主治医师决定。DES组病变血管经预扩张处理后植入直径和长度合适的支架,术后双联抗血小板治疗12个月。
1.3 观察指标
搜集患者临床基线资料及造影数据。所有患者均以门诊或电话或住院方式进行随访。记录心源性死亡、非致死性急性心肌梗死(Acute myocardial infarction,AMI)、靶病变再次血运重建(Target lesion revaseularization,TLR)等主要不良心血管事件(Major adverse cardiac events,MACE),对有临床心肌缺血证据或有意愿复查造影患者进行冠脉造影或冠脉CT并记录复查结果。
1.4 统计学方法
采用SPSS 18.0统计学软件进行数据分析。计量资料以均数±标准差(x±s)表示,组间比较采用独立样本t检验,计数资料以[n(%)]表示,组间比较采用χ2检验或Fisher确切概率法,Kaplan Meier曲线用于生存分析,P<0.05为差异有统计学意义。
2 结果
2.1 两组患者基础资料比较
DCB组和DES组各纳入48例患者,两组患者在性别、年龄、吸烟史、饮酒史、合并高血压病、糖尿病、稳定型心绞痛比例、总胆固醇、高密度脂蛋白胆固醇(High density lipoprotein cholesterol,HDL-C)、低密度脂蛋白胆固醇(Low density lipoprotein cholesterol,LDL-C)、肌酐、左心室射血分数(LVEF)及服用药物方面比较,差异无统计学意义(P>0.05)。见表1。
2.2 两组患者冠脉病变情况比较
两组患者均经由桡动脉行冠脉介入治疗,DCB组和DES组中ISR患者22例,小血管病变患者26例。两组患者在血管病变类型、血管病变支数、病变部位、病变血管直径和长度、A/B型夹层和植入DCB/DES数量上比较,差异无统计学意义(P>0.05)。见表2。两组手术过程中均未出现C型及以上夹层,即刻手术成功率为100%,住院期间无心肌梗死等不良事件发生。
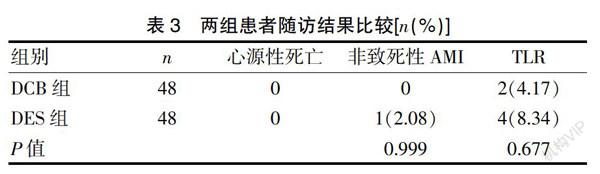
2.3两组患者随访结果比较
平均随访(9.15±5.46)个月,DES组MACE发生率(10.42%)高于DCB组(4.17%),但差异无统计学意义(P>0.05);两组均未发生心源性死亡病例,DCB组无非致死性AMI,DES组发生1例(2.08%),差异无统计学意义(P>0.05);DCB组行TLR 2例(4.17%),低于DES组4例(8.34%),但差异无统计学意义(P>0.05)。DCB组在(9.24±4.02)个月有19例患者复查冠脉造影和4例复查冠脉CT,ISR患者10例(1例血管狭窄85%),小血管病变13例(1例血管狭窄90%);DES组在(8.34±5.28)个月有14例复查冠脉造影,ISR患者6例(1例血管狭窄80%),小血管病变8例(1例血管狭窄99%的非致死性AMI,2例血管狭窄75%和80%)。见表3。生存曲线分析显示,两组在随访过程中无MACE生存率比较,差异无统计学意义(P=0.406)。见封三图1。
3 讨论
本研究结果提示,药物涂层球囊在临床上应用具有良好的疗效,与既往研究结果[7]相仿。目前临床上多用的是紫杉醇涂层球囊,将紫杉醇和碘普罗胺混合的药物涂层方法,可显著减少PCI后的血管狭窄率[8]。在PCI治疗过程中,DCB在血管狭窄部位扩张时快速撕裂病变血管内膜,短时间内抗细胞增殖药物可释放到病变血管壁并被组织吸收,从而可恢复腔内血管直径,同时治疗动脉粥样硬化、预防支架内再狭窄及发挥长期抗血管内膜增生的作用[9]。
DCB治疗ISR的效果是最先得到公认的。21世纪初,有学者[8]首先发表了研究结果,表明DCB在输送抗细胞增殖药物后可预防PTCA引起ISR的有效性,随后开启积累DCB治疗ISR循证医学证据历程。PEPCAD China ISR研究[10]结果显示,DCB相比于DES治疗组在9个月再狭窄发生率和12个月復合临床事件发生率无显著差异,2年后随访结果证实DCB治疗ISR仍然是安全和有效的[11]。最近的一项Meta[12]分析也表明,使用DCB和DES治疗ISR患者在长达2年的随访中发生MACE均较低,其差异无统计学意义(P>0.05)。本研究纳入22例ISR患者行DCB治疗,随访(9.15±5.46)个月时行TLR发生率为4.17%,与谢秀峰等[13]研究结果DES治疗ISR随访至1年行TLR发生率相近,表明DCB在治疗ISR时是一种有效策略。2020年发表的共识[5]再次将DCB治疗ISR推荐为IA类方案也直接证明了其临床应用价值。
目前对冠脉小血管病变没有明确定义,一般认为冠脉小血管的内径≤2.75 mm或<3 mm[5],本研究纳入小血管病变内径一般为2.00~2.75 mm,由于冠脉小血管管径小,支架植入后更容易发生远期管腔丢失,ISR发生率仍然很高。PEPCAD等研究[14]结果显示,随访(6.4±1.3)个月时DCB组和DCB加裸支架组比较,晚期管腔丢失分别为[(0.16±0.38)mm和(0.62±0.73)mm,P<0.0001],再狭窄发生率分别为(6%和45%,P<0.0001),在接下来的1~3年随访过程中[15],DCB组没有重大MACE发生,且与对照组相比降低了靶病变的再狭窄率,表明DCB治疗小血管病变的有效性和安全性,另一项纳入了230例患者的多中心随机对照研究[16]结果显示,DCB治疗小血管病变的疗效与DES无明显差异。本研究入选26例小血管病变患者,仅有1例在(9.24±4.02)个月出现心绞痛症状,复查造影提示靶血管狭窄90%,与DES治疗小血管病变患者结果相比,差异无统计学意义(P>0.05),提示在治疗小血管病变时,DCB扩张术可能成为重要的替代方式。我国专家[3]认为单纯DCB治疗小血管病变可能是一种优选方案。但DCB相对于DES来说还不能有效解决血管弹性回缩问题,其应用条件还需根据临床实际情况和积累更多的临床证据。
综上所述,本研究对比了DCB和DES在治疗ISR和小血管病变的临床疗效并随访了部分患者的复查冠脉造影资料,结果表明DCB在治疗ISR和小血管病变的疗效不劣于DES,可作为临床冠脉血运重建的一种重要策略。但本研究也存在一定的不足之处,首先入组样本量较少,相关数据的比较不排除研究结果与事实存在一定程度偏倚的可能,本研究为单中心试验且仅用SeQuent Please DCB,尚需多中心的临床数据和不同品牌DCB治疗效果的对比;其次由于DCB扩张时间不同,药物的释放、溶解和血管组织的吸收均不尽相同,短期内临床疗效可能无法体现,本研究平均随访时间为(9.15±5.46)个月,有必要进行更长时间的随访。
[参考文献]
[1] Brott BC,Chatterjee A. Drug-eluting balloon therapy for in-stent restenosis of drug-eluting stents:Choose and prepare the appropriate lesion[J]. JACC Cardiovascular Interventions,2018,11(10):979-980.
[2] 谢江波,温燕华,衷涛,等. 药物涂层球囊在糖尿病患者冠状动脉小血管病变中的疗效分析[J].国际心血管病杂志,2019,46(5):297-300.
[3] 陈韵岱,王建安,刘斌,等. 药物涂层球囊临床应用中国专家共识[J]. 中国介入心脏病学杂志,2016,24(2):61-67.
[4] Neumann FJ,Sousa-Uva M,Ahlsson A,et al. 2018 ESC/EACTS guidelines on myocardial revascularization:The task force on myocardial revascularization of the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery(EACTS). Developed with the special contribution of the European Association for Percutaneous Cardiovascular Interventions(EAPCI)[J]. Eur Heart J,2019,40(2):87-165.
[5] Jeger RV,Eccleshall S,Wan Ahmad WA,et al. Drug-coated balloons for coronary artery disease:Third report of the International DCB Consensus Group[J]. JACC Cardiovasc Interv,2020,13(12):1391-1402.
[6] 葛均波,徐永健,王辰.內科学[M].9版.北京:人民卫生出版社,2018:218-244.
[7] Cai JZ,Zhu YX,Wang XY,et al. Comparison of new-generation drug-eluting stents versus drug-coated balloon for in-stent restenosis:A meta-analysis of randomized controlled trials[J]. BMJ Open,2018,8(2):e017 231.
[8] 赵韧,韩雅玲. “介入无置入”理念的兴起和前景[J].中国心血管病杂志,2019,24(6):493-495.
[9] Bukka,Rednam PJ.Drug-eluting balloon:Design,technology and clinical aspects[J]. Biomed Mater,2018,13(3): 032 001.
[10] Xu B,Gao R,Wang J,et al. A prospective,multicenter,randomized trial of paclitaxel-coated balloon versus paclitaxel-eluting stent for the treatment of drug-eluting stent in-stent restenosis:Results from the PEPCAD China ISR trial[J]. JACC Cardiovasc Interv,2014,7(2):204-211.
[11] Xu B,Qian J,Ge J,et al. Two-year results and subgroup analyses of the PEPCAD China in-stent restenosis trial:A prospective,multicenter,randomized trial for the treatment of drug-eluting stent in-stent restenosis[J]. Catheter Cardiovasc Interv,2016,87:624-629.
[12] 蔡金赞,陈凯伦,贾海波,等. 普通球囊、药物涂层球囊及药物洗脱支架治疗冠状动脉支架内再狭窄的长期疗效Meta分析[J].中国循环杂志,2018,33(9):873-878.
[13] 谢秀峰,张越,曲泽.药物洗脱球囊和药物洗脱支架对支架内再狭窄的疗效比较[J].中国组织工程研究,2020, 24(4):555-560.
[14] Unverdorben M,Kleber FX,Heuer H,et al. Treatment of small coronary arteties with a paclitaxel-coated balloon catheter[J]. Clin Res Cardiol,2010,99(3):165-174.
[15] Unverdorben M,Kleber FX,Heuer H,et al. Treatment of small coronary arteries with a paclitaxel-coated balloon catheter in the PEPCAD I study:Are lesions clinically stable from 12 to 36 months?[J]. Euro Intervention,2013, 9:620-628.
[16] Tang Y,Qiao S,Su X,et al. Drug-coated balloon versus drug-eluting stent for small-vessel disease:The restore SVD China randomized trial[J]. JACC Cardiovasc Interv,2018,11(23): 2381-2392.
(收稿日期:2021-02-19)