1例ANCN相关性血管炎合并肺炎患者诊断与治疗的药学实践
胡艳芬 余焕香 陈云武
[摘要] 抗中性粒细胞胞浆抗体(ANCA)相关性血管炎(AAV)是一种以小血管壁的炎症和纤维素样坏死为特征的血管炎。抗中性粒细胞胞浆抗体相关性血管炎常累及肺脏和肾脏,其中以肺部症状为主或首发的患者,常被误诊。临床药师通过参与1例抗中性粒细胞胞浆抗体相关性血管炎合并肺炎患者的诊断和治疗方案的调整,学习和探讨该类疾病及其并发症的诊断要点及治疗药物的选择,并复习治疗药物的监护重点。通过对治疗药物实施药学监护,可提高药物治疗的安全性和有效性。
[关键词] ANCA相关性血管炎;肺炎;诊断;治疗;药学监护
[中图分类号] R971 [文献标识码] C [文章编号] 1673-9701(2021)25-0147-05
Pharmaceutical practice of diagnosis and treatment of a patient with ANCA-related vasculitis complicated with pneumonia
HU Yanfen YU Huanxiang CHEN Yunwu
Department of Pharmacy, the First People′s Hospital of Zhaotong City in Yunnan Province, Zhaotong 657000,China
[Abstract] Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a type of vasculitis characterized by inflammation and fibrinoid necrosis of small blood vessel walls. Antineutrophil cytoplasmic antibody-related vasculitis often involves the lungs and kidneys, and patients with pulmonary symptoms as the main or first episode are often misdiagnosed. The clinical pharmacist participated in adjusting the diagnosis and treatment plan of a patient with anti-neutrophil cytoplasmic antibody-related vasculitis and pneumonia, learned and discussed the diagnosis points of this type of disease and its complications the choice of treatment drugs. And they reviewed the key points of monitoring of therapeutic drugs. The safety and effectiveness of drug treatment can be improved through the implementation of pharmaceutical monitoring of therapeutic drugs.
[Key words] ANCA-related vasculitis; Pneumonia; Diagnosis; Treatment; Pharmaceutical care
抗中性粒細胞胞浆抗体(Anti-neutrophil cytoplasmic antibodies,ANCA)相关性血管炎(Anti-neutrophil cytoplasmic antibody associated vasculitis,AAV)是一种以小血管壁的炎症和纤维素样坏死为特征的血管炎,其主要自身抗原靶标为髓过氧化物酶(Myeloperoxidase,MPO)和蛋白酶3(Protease3,PR3)[1]。AAV常累及多个脏器,其中肾脏和肺脏较易受累,目前对以肺部症状为主或首发的患者,常被误诊为肺部感染、间质性肺疾病、肺结核或肿瘤,进而延误治疗[2]。本案例临床药师通过参与临床会诊,对1例ANCA相关性血管炎合并肺炎患者的诊断和治疗提供相关建议,并实施药学监护,为临床合理制定该类疾病的用药提供参考,现报道如下。
1 资料与方法
1.1 临床资料
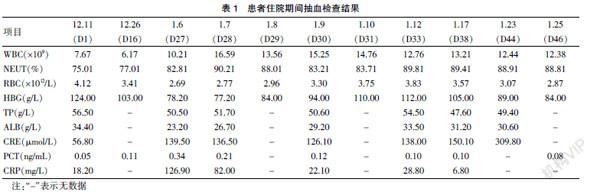
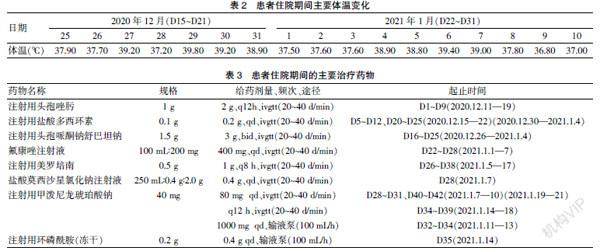
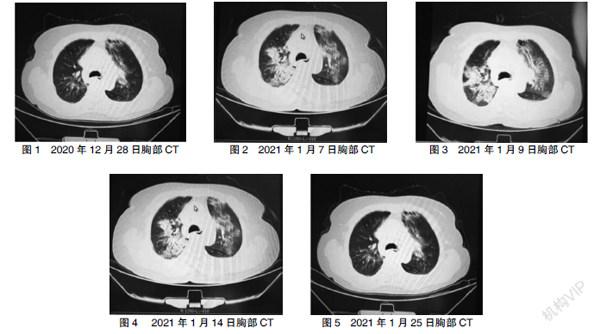
患者,女,63岁,身高168 cm,体重68 kg,因“反复咳嗽、咳痰7年余,再发加重伴喘息、咯血痰半月余”入院。入院查体:T:36.8 ℃、P:90次/min、R:22次/min、BP:128/70 mmHg、SPO2:89%;听诊:双肺呼吸音减弱,右下肺可闻及少许湿性啰音,HR:90 次/min,律齐,各瓣膜听诊区未闻及杂音;腹软、无压痛、肝脾、未触及、双下肢无水肿;2020年12月11日(D1)血常规示:WBC:7.67×109/L,NEUT(%):75.01、PCT:0.05 ng/mL、TP:56.50 g/L、ALB:34.40 g/L;门诊胸部CT提示:①一右肺尖及中叶钙化结节灶,考虑陈旧可能;②双肺磨玻璃病变,考虑出血可能;③局部支气管扩张征象:右上叶前段磨玻璃结节;④主动脉壁钙化;⑤右侧胸膜局部增厚。入院诊断:①肺炎、呼吸衰竭;②支气管扩张并咯血;③慢性支气管炎急性病加重期,肺气肿;④慢性胃炎。

