Progress in Implant-Based Breast Reconstruction:What Do We Know?
Xueqing HU ,Cheng HUANG
KEY WORDS Breast reconstruction;Implant;Acellular dermal matrix;Expander
Breast cancer is the most common malignancy and the most frequently diagnosed cancer in women worldwide[1].In China,the incidence rate of breast cancer among women has been showing an upward trend and is higher in urban areas[2].Breast reconstruction after mastectomy for breast cancer is crucial for physical and psychosocial QoL[3-6].Plastic surgeons offer effective restoration of breast symmetry,size,volume,contour,and position,giving patients the freedom to dress up even after mastectomy.In China,it has been found that women who decide to undergo breast reconstruction generally have poor knowledge of breast reconstruction as well as pre-and post-surgery preparation.In addition,there is a dearth of knowledge on the basic principles of plastic surgery among many general surgeons in China who intend to work in breast reconstruction,probably due to a lack of theoretical knowledge on plastic surgery and rigorous technical training.Therefore,stepwise learning of plastic surgery methods may be an effective way to train young plastic surgeons.
Generally,several breast reconstruction methods can be considered,including prostheses,autografts,and combined autograft-prosthetic reconstruction.To achieve this,plastic surgeons must undergo extensive plastic surgery training.
AUTOLOGOUS VERSUS PROSTHETIC BREAST RECONSTRUCTION:WHERE DO WE STAND?
There are two different types of breast reconstruction procedures:autologous tissue-based and prosthetic expander/implant-based reconstruction[7].Because mastectomy is the first-stage surgery for breast cancer treatment,postmastectomy breast reconstruction has several important implications.The primary outcome is the initial surgical treatment of breast cancer and receipt of breast reconstruction at any time after mastectomy.Expander/implantbased reconstruction has rapidly increased in recent years and is associated with complications such as contralateral augmentation[8].Several vital prospective cohort studies have been conducted by the Multicenter Reconstruction Outcomes Consortium to examine breast reconstruction outcomes across 11 centers[9-11].Among patients recruited from North America,those who underwent autologous reconstruction expressed greater satisfaction with their breasts[9].In China,patients who underwent autologous reconstruction have been found to be more prone to intraoperative,postoperative,and re-operative complications than those who underwent prosthetic reconstruction.Patients who underwent prosthetic reconstruction had a lower chance of opportunistic infections and clinical failure[10].However,previous domestic studies comparing autologous tissue-based breast reconstruction techniques and prosthetic implant-based reconstruction have been limited due to a lack of high-quality patient-reported outcome (PRO) data.While autologous tissue-based breast reconstruction“does all the work upfront”,prostheticbased techniques are frequently employed to save operating room hours.In the current healthcare environment,a cost-effective outcome using PRO data may guide surgical decisions.Long-term studies[12-13]can help overcome these limitations.
PROSTHETIC IMPLANT-BASED RECONSTRUCTION IS NOT EQUAL TO PROSTHETIC AUGMENTATION MAMMOPLASTY
Breast reconstruction using flaps,such as latissimus dorsi muscle flaps,free/pedicle transverse rectus abdominis musculocutaneous flaps,and deep inferior epigastric artery perforator flaps,allows model selection for women undergoing autologous reconstruction when soft tissue transfer is needed.However,prosthetic reconstruction has been widely used.Most breast cancer mastectomy patients are required to determine whether prosthetic reconstruction can be considered for each subject[14].Indeed,there is a difference between prosthetic implant-based reconstruction and prosthetic augmentation mammoplasty.The confusion between these two techniques may be avoided by addressing misconceptions during educational sessions.Autologous tissue differs in various ways,including vascular supply,thickness,and texture,especially for breast reconstruction after radiotherapy (whole breast irradiation plus a boost)[15].In many situations,for a given augmented volume of the reconstructed breast in patients who underwent mastectomy via tissue expander/implantbased reconstruction,patients have been shown to have increased satisfaction with long-term outcomes.Nonetheless,an autologous flap is more practical for irradiated damaged breast reconstruction areas to provide sufficient volume.It is often argued that advanced tissue expanderassisted reconstruction is needed.Pectoralis major muscle rupture during subcutaneous tissue separation impedes continuity.Second-stage breast reconstruction requires a scrupulous surgical technique because the breast has to be removed through a tiny incision via mastectomy.Moreover,neoadjuvant chemotherapy often increases the implant-based surgical risk and postoperative complications[16].Therefore,the optimal regimen remains to be determined.
EXPANDERS ARE NOT FOR DILATION
To efficiently obtain“extra”skin tissue using“expansionin-situ”,one or more expanders are implanted beneath the skin.The expander replaces the prosthesis to occupy the tissue space after mastectomy,maintaining the area of the skin and soft tissue and preserving the optimal tissue conditions for subsequent reconstruction.
Techniques for expanding skin and soft tissues are widely used to repair defective areas because they offer a similar texture and skin color to the damaged region.However,these benefits come at a cost,such as loss of reconstruction effectiveness and increased risk of complications.There is currently limited,very low-quality evidence to support the use of expanders for dilation in the absence of hard tissue support.The expander forms extra skin tissue through a directional trend that depends on the properties of the hard supporting layer.We must recognize that an expander is not for dilation but for occupying space.
Post-mastectomy radiation therapy poses a challenge for plastic surgeons.Partial expander deflation exacerbates the adverse effects of radiotherapy in two-stage breast reconstruction[17].Whether the expander should be placed,and if placed,whether it should be inflated or deflated during radiotherapy is debated[18].Clinically,since the introduction of the concept of delayed immediate breast reconstruction,complete deflation before radiotherapy has been recommended as more conducive to addressing the internal mammary nodes to avoid adverse effects such as fat necrosis,flap volume loss,and contraction[19-21].Is there a better time to irradiate when performing immediate implant-based breast reconstruction? This certainly merits further exploration.Keeping the expanders fully inflated may avoid these adverse effects.The expander forms extra skin tissue through a directional trend that depends on the properties of the hard supporting layer.
Unlike conventional tissue expansion,dynamic expansion should be considered in breast reconstruction because nipple malposition may occur after nipple-sparing mastectomy and expander-implant reconstruction.The breast prostheses or tissue expanders in the empty hemithorax are far from sufficient.Plump and elastic breasts are functionally and esthetically necessary.However,there are some limitations to this study.Although small and nonptotic breasts after expansion have a relatively pleasing symmetry,large and ptotic breasts exhibit upward deviation from the nipple (Fig.1).
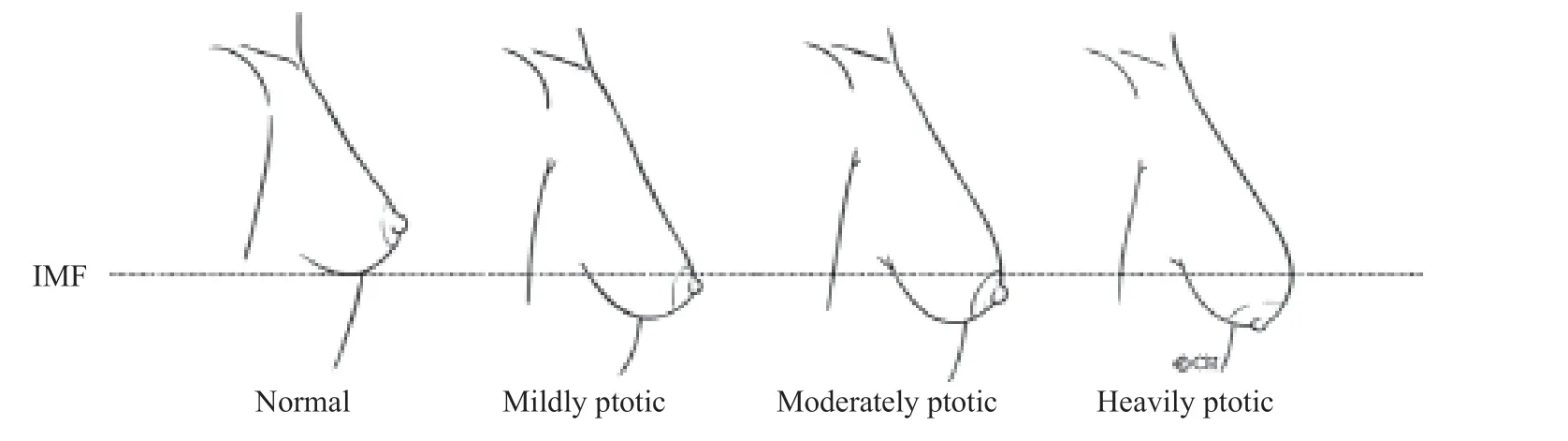
Fig.1 Breast ptosis. Small and non-ptotic breasts after expansion showed relatively pleasing symmetry,while large and ptotic breasts showed upward deviation from the nipple.
ACELLULAR DERMAL MATRICES ASSIST EXPANDER-IMPLANT BREAST RECONSTRUCTION
Acellular dermal matrices (ADMs) have demonstrated success in primary breast reconstruction using prosthetic devices (Fig.2).Submuscular and prepectoral breast reconstruction using ADMs do not differ significantly in complication rates[22-23].ADM use for implant-based breast reconstruction does not appear to increase or decrease the risk of complications[24]but contributes to increased postoperative satisfaction rates.During submuscular breast reconstruction,an ADM can be placed to obtain adequate coverage of the inferior pole of the implant.The breast has an ideal volume,and the surgeon needs to use an implant to augment the volume for reconstruction.However,the pectoralis major muscle cannot completely cover the inferior pole of the implant[23,25].Based on these findings,ADMs have become a cornerstone for implant-based breast reconstruction over the last two decades.While the dual-plane subpectoral approach can reduce the operation time and improve the expansion of the lower pole,it requires fixing to the inframammary fold (IMF) as the definition of the IMF location allows the formation of continuous stress between the pectoralis major muscle and IMF.The implant is inserted beneath the pectoralis ADM layer,and the ADM is sutured to the IMF to cover and secure the implant in a hand-in-glove fit.There is conflicting evidence on the use of ADM in expander/implant breast reconstruction.The plastic surgeon should evaluate the patient’s condition and decide whether to use it.
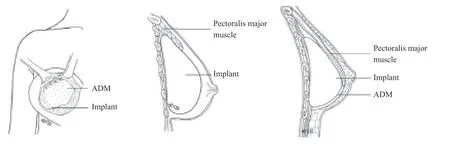
Fig.2 (A) An inferior gutter of ADM offers IMF support.(B) The pectoralis major muscle is often retracted under the clavicle and the reconstructed prosthesis is exposed directly under the skin.(C) After the ADM is used,the pectoralis major is restored to the dual-plane approach.
When and how do we use ADM?Ⅰ) Mildly or moderately ptotic breasts are appropriate,while it is less applicable to heavily ptotic breasts;Ⅱ) the IMF has not yet been destroyed;Ⅲ) the superior part of the pectoralis major muscle has not been widely separated;Ⅳ) the well-perfused flap blood supply (inferior and superior) should be the ultimate indicator and is directly correlated.If blood supply is inadequate,ADM should not be used.Moreover,ADM does not increase the thickness of the prosthesis and,therefore,does not affect its softness.
INFECTIOUS COMPLICATIONS LEAD TO EXPLANATION IN IMPLANT-BASED BREAST RECONSTRUCTION
As any foreign prosthetic material is inserted into the body,infection remains the most dreaded complication of implant-based breast reconstruction[8].Postoperative infection is defined as any of the following:Ⅰ) requirement for continuation or even escalation of antibiotics against clinical signs of infection or Ⅱ) confirmation of pathogenic bacteria cultured from the wound site.Surgical treatment requirement is defined as the need for an operative procedure to resolve complications with prompt antibiotic treatment that occurred at the operation site,with the complications directly related to nipple-sparing mastectomy and immediate breast reconstruction procedures.A poorly perfused skin flap is a major risk factor for infectious complications.
NIPPLES CANNOT BE IGNORED
Nipple-sparing mastectomy procedures have become standard at many medical centers and are preferred over skin-sparing or skin-reducing procedures[26-30](Fig. 3).One may speculate why surgeons undertake such a cumbersome,complex procedure if nipples can be reconstructed later.This may be attributed to the fact that patients are generally less satisfied with reconstructed nipples or nipple-like tattoos.
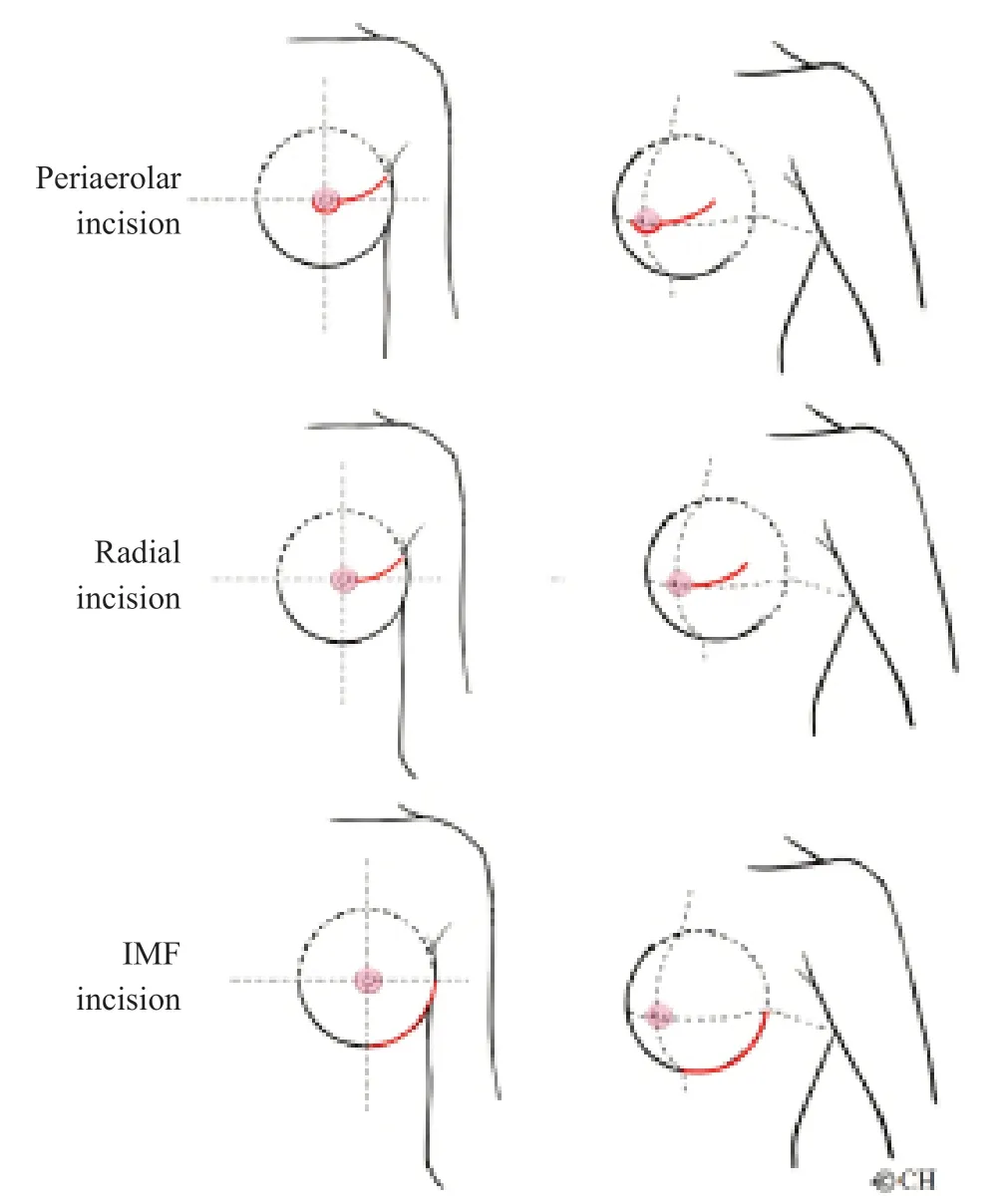
Fig.3 Nipple-sparing mastectomy incisions
Patients with gradeⅠorⅡbreast ptosis are suitable candidates for nipple preservation.For a grade Ⅲ ptosis patient who would like to retain the same size and volume of their breast,the skin envelope pocket may be filled or overfilled using an IMF incision.When nipple preservation is impossible,an areola-sparing procedure may be considered.Relative to skin-sparing procedures,this preserves more skin during mastectomy,which has advantages for direct-to-implant reconstruction and may obviate the desire for nipple reconstruction[23].Despite the nipple-areola complex-related oncologic risk,more recent reports[31]have demonstrated that nipple-sparing mastectomy may carry a tolerable risk in selected patients with a negative axillary node.
REFLECTIONS,PERSPECTIVES,AND VISIONS
In the transformation of the surgical process from delayed to immediate breast reconstruction,implant placement was a significant factor in evolution from a fully submuscular approach to partial muscular coverage of the implant,also known as the dual-plane subpectoral approach,and finally to no muscle coverage (prepectoral reconstruction).Prepectoral implant-based reconstruction offers a safe reconstructive approach to all oncologic principles.Limitations of the current study in China include the small sample size and short-term follow-up.A study with a larger sample size and long-term follow-up is needed.
A direct result of the advances in oncoplastic surgery is the combination of tumor resection,skin flap preparation (by a breast surgeon),and breast reconstruction (by a plastic surgeon) for satisfactory esthetic outcomes.
A flowchart of our implant-based breast reconstruction design is shown in Fig.4.
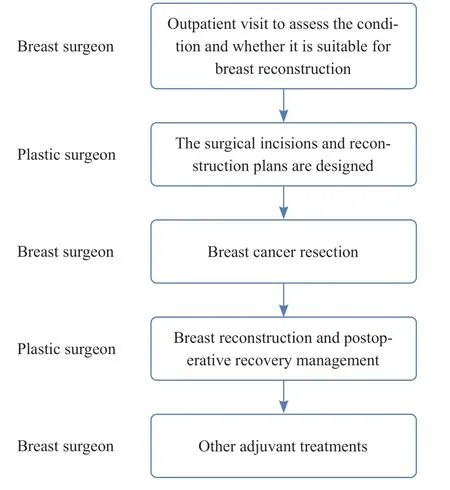
Fig.4 Breast reconstruction flowchart
Although the literature does not support advanced disease as a contraindication to breast reconstruction,women and their physicians may not perceive the procedure as a high priority.Given all that has been mentioned so far,we hold the view that Ⅰ) tissue blood supply is the first requirement for successful plastic surgery,and prosthesis exposure and infection are often related to blood supply;Ⅱ) differences between general tissue expansion and breast reconstruction should be understood;Ⅲ) indications for prosthesis breast reconstruction should be understood.It should be known that breasts cannot be made entirely via reconstruction with an implant only (possibly expansion first);Ⅳ) the influence of the change in the relative position of the tissue level on breast shape reconstruction should be understood;Ⅴ) the techniques of expander/implant-based treatment,cavity adjustment,and tissue transplantation should be mastered to improve the effect of prosthesis reconstruction;Ⅵ) breast reconstruction with a small volume and gradual replacement of the breast prosthesis with autologous fat should be known;Ⅶ) decisions should be made by a multidisciplinary team.
More than ever,we are well-placed to reconstruct breasts that perform equally,or,in some cases,better than the original breast using implant-based reconstruction.
ETHICS DECLARATIONS
Ethics Approval and Consent to Participate
N/A
Consent for Publication
All the authors have consented to the publication of this article.
Competing Interests
The authors declare that they have no competing interests.The authors state that the views expressed in the article are their own and not the official position of the institution or funder.
 Chinese Journal of Plastic and Reconstructive Surgery2021年2期
Chinese Journal of Plastic and Reconstructive Surgery2021年2期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- The Practice of China’s Cosmetic Medicine Dated Back to 3 800-4 800 Years Ago
- Electric Field:A Key Signal in Wound Healing
- Mechanisms and Management of Postparalysis Facial Synkinesis
- Looped,Broad,and Deep Buried Suturing Technique for Wound Closure
- A Novel Composite Skin Graft Technique with Fat Derivatives
- A Case of Congenital Syringocystadenoma Papilliferum
