Mechanisms and Management of Postparalysis Facial Synkinesis
Xinying HUANG ,Wei WANG ,Wei DING,*
1 Department of Plastic and Reconstructive Surgery,Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai 200011,China
2 Shanghai Medical College,Fudan University,Shanghai 200032,China
KEY WORDS
INTRODUCTION
Facial synkinesis refers to synchronous and involuntary contractions of the muscles during volitional movements[1],and it is considered one of the most severe sequelae of facial nerve paralysis.It has various etiologies.Oral-ocular synkinesis is the most frequent pattern of facial synkinesis.It is characterized by involuntary eye closure (orbicularis oculi) during voluntary smiling (zygomaticus major or minor).Specific manifestations differ depending on the severity.
Severe synkinesis results in impaired social communication.Individuals with facial synkinesis may also experience reduced psychological status and quality of life[2-3].The pathogenesis of facial synkinesis remains unclear,and several mechanisms have been proposed.Different strategies for improvement have been applied clinically.
MECHANISMS BEHIND POSTPARALYSIS FACIAL SYNKINESIS
The mechanisms that have been discussed so far relate to the various anatomical levels of the facial nerve.
Aberrant Regeneration
The aberrant regeneration hypothesis has long been the most widely accepted explanation for synkinesis.It is believed that when axons and the endoneurium lose their continuity in nerve injuries,they cannot correctly guide regenerative nerve fibers.These fibers develop into neighboring endoneurial tubes and innervate the wrong muscles[4-5].Evidence supporting this theory includes the classic and representative Baker’s experiment[6]on cynomolgus monkeys that exhibited postparalysis ocular-oral synkinesis.With the aid of retrograde neuroanatomical tracers,they found that the perioral muscles of the monkeys were innervated by nerve fibers that originally dominated the muscles surrounding the eyes.There are more experiments on animals that validate incorrect innervation during the regeneration of facial nerves[7-10].
Ephaptic Transmission
The ephaptic transmission theory was developed from the hypothesis of abnormal nerve impulses that appear between adjacent axons with incomplete myelin sheath formation.Shunts between axons dominating different parts of the facial muscles allow nerve impulse conduction to another fiber when one fiber excites and finally induces synchronous movements of muscles[11].Research on hemifacial spasm (HFS) found that shunts are more likely to occur in the root entry zone (REZ) where facial nerves have no protection of the myelin sheath[12].However,it is unclear whether this phenomenon also occurs during the development of postparalysis facial synkinesis (PPFS).Takeda[13]revealed that ephaptic transmission occurs in synkinesis during HFS,and it has less to do with long-term synkinesis after facial paralysis.
These investigations on ephaptic transmission also indicate that there are two different pathological processes behind post-paralysis synkinesis and HFS.Clinicians should therefore distinguish between these two processes as they may have similar manifestations.
Overacting of the Facial Nucleus
Based simply on aberrant regeneration,the incidence of the different patterns of facial synkinesis after paralysis should be nearly equal because of the diffuse distribution of facial nerves.Moran’s experiment showed contradictory data that zygomaticus muscle involvement leading to oral-ocular synkinesis is much more common[14].This result suggests that the process behind facial nerve regeneration is not random,which draws researchers’ attention to the role of the facial nucleus in postparalysis facial synkinesis.Correlated research confirmed the increased excitability of the facial nucleus in patients with facial synkinesis[15].In recent research,Suming et al.[16]emphasized that two specific types of motor neurons in the facial nucleus are involved in this pathological process.
It is worth mentioning that overaction of the facial nucleus exists in both HFS and postparalysis synkinesis[17],which makes the role of this theory more definite than ephaptic transmission among various mechanisms.
Changes in the Cerebral Cortex
Along with the emerging examination technologies,such as functional magnetic resonance imaging (fMRI) of the nervous system,recent research on the mechanisms behind postparalysis synthesis has focused on the changes in the cerebral cortex.
A series of functional transformations occur in the cerebral cortex during the recovery process of facial nerve injuries[18].Distinguished changes appear in the early stage of facial paralysis,and even the severity can be quantified by examination[19].Several regions in the cerebral cortex,such as the areas of sensorimotor connection,processing,regulation,and movement execution,show varying degrees of functional changes in facial paralysis cases[20].Wang et al.performed smiling and blinking tasks in both healthy subjects and patients with postparalysis facial synkinesis and tested the activation of the cortex using fMRI.The results demonstrated that blinking and smiling in the contralateral primary sensorimotor cortex of the patient were almost overlapping,whereas representations in the healthy control seemed to be separated from each other (Fig.1)[22],and more intense activity in the supplementary motor area on the unaffected side than that on the affected side was shown in the patients (Fig. 2)[23].Wu et al.reported that several brain areas in patients with synkinesis differed from those in healthy people in increased amplitude of low-frequency fluctuation for the ipsilateral insula,which was demonstrated to contribute to hand and eye motor movement in motor control[23].This may be one of the potential mechanisms of postparalysis facial synkinesis at the cortical level.

Fig.1 Activation maps in left blinking (red color) and smiling (yellow color) facial tasks of a patient with left facial synkinesis (A) and a healthy control (B)
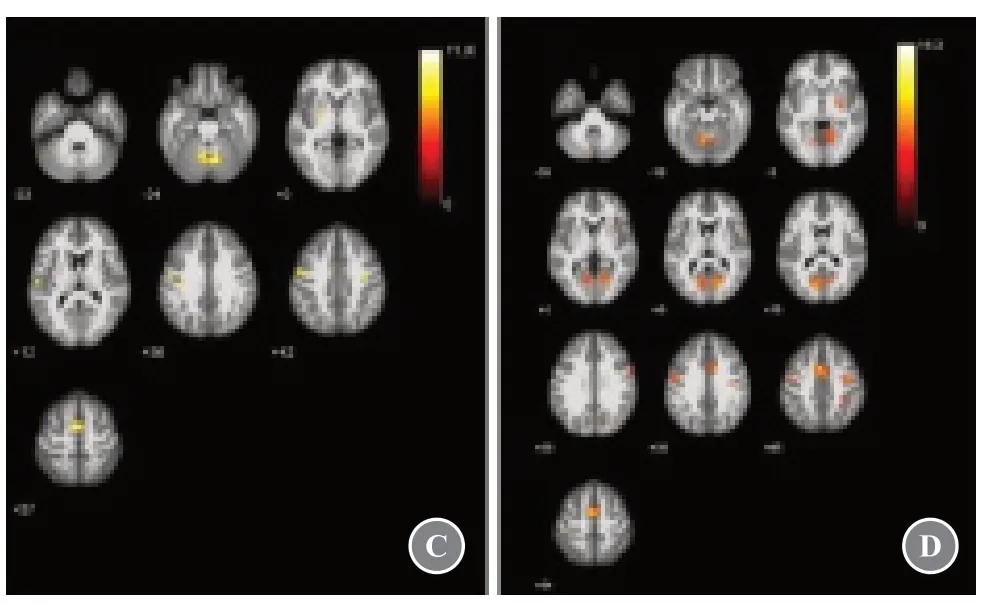
Fig.2 Activated brain regions in the patient group on the affected side (C) and the unaffected side (D) during blinking
To date,there is no clear explanation for why synkinesis occurs after facial paralysis.Disorders in every link of the entire facial nerve system participate in the complex pathophysiology of facial synkinesis.The importance of the different mechanisms in the various severities,stages,or patterns of facial synkinesis is also diverse.The challenges for clinicians when making individual and optimal treatment programs arise from this complexity.
CLINICAL MANAGEMENT
Facial synkinesis has long been a difficult issue in the treatment of facial paralysis.Long-lasting and more effi-cient therapies are still under investigation.It is a pity that patients with synkinesis cannot recover completely.The goals of the present therapies emphasize controlling of the occurrence of synkinesis,improving facial expression,and enhancing the quality of life.
Botulinum Toxin Type A Injection
Botulinum toxin type A (BTX-A) injection is a classic method for the treatment of postparalysis facial synkinesis.Several clinical trials have proven that BTX-A injection contributes to reduced involuntary facial movement,improved symmetry of facial expression[24],and enhanced quality of life[25].There are still more details of BTX-A injection therapy,such as differences between injection regimens and diverse reactions towards treatment of individuals with different patterns of synkinesis and with different backgrounds.These details have been explored recently.
Shinn et al.[26]reported 99 cases of post-paralysis facial synkinesis following BTX-A injection.On comparison,younger and female patients had better therapeutic effects.Additionally,the larger the dose administered,the greater the response was.Alipour’s retrospective data analysis of long-term therapy with BTX-A in 73 patients showed that there was a significant increase in dosage during repeated treatment,whereas the dose per muscle and time intervals remained stable[27].
Unfortunately,cases of botulinum resistance have been reported in clinical studies.BTX-A injection does not appear to work as well in patients with botulinum resistance,probably because of the existing neutralizing antibodies or other reasons[28-29].Overall,long-term therapy and complex injection plans are crucial issues to be addressed in BTX-A injection treatment.The optimal injection plan relies on repeated adjustments according to individual health conditions and reactions to treatment.
Surgical Strategies
Surgical strategies for postparalysis facial synkinesis are mainly directed to the facial nerves and muscle modification.With the changing concept of surgical management and further research,more limited and selective strategies for facial movement disorders are being pursued by clinicians[30].
Coleman[31]performed total neurectomy in patients with HFS for the first time,and the symptoms of these patients were significantly relieved.In comparison to HFS,myectomy is performed more frequently than neurectomy because of its better efficacy in cases of postparalysis facial synkinesis.Julia et al.[32]reported highly selective facial neurectomy and nerve grafting accompanied by BTX-A injection and neuromuscular reeducation training,which resulted in improved facial expressions.Azizzadeh et al.[33]proposed modified selective neurectomy and emphasized its effect on smile ability enhancement.In terms of facial muscles,the key point in surgical strategies is the removal of specific parts of the muscles involved in involuntary movements depending on the pattern of synkinesis,for example,perioral muscle excision for patients with ocular-oral synkinesis.Different types of surgical approaches can be used.Chuang et al.[34]discussed the choice of different surgical strategies for patients with various patterns of synkinesis,including combined myectomy,neurectomy,and cross-facial nerve grafting.Krag et al.[35]reported a strategy for depressor anguli oris muscle myectomy based on their discovery that the antagonistic action of a hypertonic depressor anguli oris muscle and concomitantly weak depressor labii inferioris muscle could be a direct cause of ocular-oral synkinesis,and the depressor anguli oris muscle receives innervation from both the lower buccal and marginal mandibular facial nerve branches.
Despite the technical advances and progress in surgical operations,it has been widely accepted that surgical management has defined roles in treating facial synkinesis.However,the risks of surgery,such as injuries to uninvolved facial parts,flaccid paralysis,and other problems,cannot be ignored.In contrast,overly conservative operations pose a risk of a probable second operation or supplemental BTX-A injection[36].Due to the sophistication of the anatomy and the diversity of the patterns of facial synkinesis,personalized analysis of the patient’s condition and comprehensive preoperative examination with the help of electromyography (EMG) or other implements are required during surgical protocols.Accuracy of the target,control of surgery-related injury,and maintenance of efficacy are the surgeons’ goals.
Neuromuscular Reeducation
Neuromuscular reeducation,an essential option for the treatment of facial paralysis,refers to selective muscle control training to improve muscle movement.The process of reeducation intrinsically restores the motor control pathway from the peripheral to the central nervous system by using physical therapy or exercise,with the aim of biofeedback,electromuscular feedback,or other techniques.It is worth mentioning that this type of treatment is better for recovery from complete nerve injuries (Sunderland Ⅲ)[37].
Previous studies have confirmed the positive role of neuromuscular reeducation in treating post-paralysis facial synkinesis[38-40].During therapy,patients gradually learn to control the occurrence of the involuntary movements with the help of a mirror,EMG,or other tools as a kind of visual or electrical feedback to the cerebral cortex.
Among the various training approaches in neuromuscular reeducation,mirror therapy has recently been a hot research topic as it is a non-invasive technique.Its therapeutic value has already been approved for phantom limb pain,stroke rehabilitation,etc.[41-42].The mechanisms behind mirror therapy involve complicated theories,including mirror neurons in the cerebral cortex,connection between visual afferent signals and motor efferent commands,enabling of the ipsilateral motor pathway,and so on[43].
Paolucci et al.[44]used a type of software that makes a duplicate of a patient’s non-paretic face on a computer screen to show a representation of his complete prelesional face.Compared to traditional rehabilitation training,patients receive better facial function improvement,and their quality of life is significantly enhanced.In addition,this kind of treatment encourages patients by showing them their healthy faces,which helps them persist in the long term.This can be a remarkable advantage of this therapy,as it conquers the difficulty of maintaining regular and continuous training.
The efficacy of neuromuscular reeducation,in turn,suggests that the cerebral cortex is associated with the development of postparalysis facial synkinesis,and its plasticity may be the key factor that influences the efficacy of neuromuscular reeducation.Based on this hypothesis,if specific functional areas in the cerebral cortex that contribute to facial synkinesis can be targeted,more direct stimulation,such as repeated transcranial magnetic stimulation[45],can bring more immediate and direct therapeutic benefits.
In summary,different methods play different roles in the management of postparalysis facial synkinesis.Several factors,including severity and duration of symptoms,sex,age,etc.[46],affect the development of a specific treatment method.The combination of several therapies results in a better prognosis.For example,combination of mirror therapy,BTX-A injection,surgery followed by BTX-A injection supplement,or other treatment modalities[47-48],has been shown to be superior to monotherapy.
CONCLUSION
As facial synkinesis is one of the most severe sequelae of facial nerve paralysis and significantly impacts patients’ quality of life,it should be handled seriously.Existing hypotheses for its mechanisms have discussed every link of the facial movement procedures from the peripheral to the central level,and its current management includes BTX-A injection,surgical strategies,and neuromuscular reeducation.To seek more efficient and noninvasive treatments,further research on its pathophysiology is urgently needed.Clinicians should consider the individual differences during the designing of treatment plans.Sufficient assessment and communication with patients are always required.
ETHICS DECLARATIONS
Ethics Approval and Consent to Participate
N/A
Consent for Publication
All the authors have consented to the publication of this article.
Competing Interests
The authors declare no conflicts of interest.The authors state that the views expressed in the article are their own and not the official position of the institution or funder.
 Chinese Journal of Plastic and Reconstructive Surgery2021年2期
Chinese Journal of Plastic and Reconstructive Surgery2021年2期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- The Practice of China’s Cosmetic Medicine Dated Back to 3 800-4 800 Years Ago
- Progress in Implant-Based Breast Reconstruction:What Do We Know?
- Electric Field:A Key Signal in Wound Healing
- Looped,Broad,and Deep Buried Suturing Technique for Wound Closure
- A Novel Composite Skin Graft Technique with Fat Derivatives
- A Case of Congenital Syringocystadenoma Papilliferum
