The predictive value of preoperative albumin-to-globulin ratio in patients with hilar cholangiocarcinoma
Hong-Gen Liu,Liu Yong, and Ying-Jie Jia
Abstract—Background:Toinvestigate the associations between preoperative albumin-to-globulin ratio and clinicalpathological factors,and the impacts of albumin-to-globulin ratio on the longterm outcomes and postoperative complications in hilar cholangiocarcinoma. Methods: Ninety-seven hilar cholangiocarcinoma patients were enrolled in our study.The clinicalpathological and survival information were collected. Correlation analysis was using chi-square test and logistic regression. Univariate analysis was done by Log-rank test, multivariate analysis was performed using the Cox proportional hazard regression model. Results:The optimal cutoff value of the preoperative albumin-to-globulin ratio was set at 1.34, The albumin-to-globulin ratio level was elevated in 49 hilar cholangiocarcinoma patients, while other 48 hilar cholangiocarcinoma patients were with low level. Tumor stage (OR = 2,621; P = 0.003) and lymph node metastasis(OR = 3.704; P = 0.004) were identified as independently risks of albumin-to-globulin ratio level in hilar cholangiocarcinoma patients. Multivariate Cox proportional hazard regression model found differentiation (HR = 1.989; P =0.014), tumor stage (HR= 1.480; P =0.014) and albumin-to-globulin ratio level (HR =0.037; P = 0.017) were identified as the independent factors of the overall survival. Furthermore, we found the low albumin-toglobulin ratio level (OR = 0.037; P = 0.017) was an independent risk factor for the incidence of postoperative complications.Conclusions: Preoperative albumin-to-globulin ratio is a simple and useful marker not only to identify patients at increased risk for postoperative complications, but also to predict long-term survival.
Keywords—Hilar cholangiocarcinoma, Albumintoglobulin ratio,Prognosis,Postoperative complications
I. BACKGROUND
Hilar cholangiocarcinoma (HC) continues to be one of the most high frequency causes of cancer related mortality [1].Surgery is the only curative treatment. Due to the specific location, HC is often diagnosed with advanced stages and the majority of HC patients lost the chance of radical surgery [2].How to improve the survival and reduce the morbidity rate still remain urgent issues. Consequently, identifying novel biomarkers could help in designing treatment strategies and stratifying HC patients with poor prognosis.
It is well-know that malnutrition is closely associated with the incidence of postoperative complications, length of hospital stay,short overall survival,quality of life and increased mortality after surgery [3]. Cancer patients are often associated with increased malnutrition rates.Malnutrition is awellknown factor capable of impairing the immunological functions, contributing to an increased risk of postoperative infectious, anastomotic trouble, and metastasis [4]. Albuminto-globulin ratio (AGR) has been suggested as an effective factor related with nutrition status. The AGR are based on two simple laboratory parameters,abumins and globulin,which are measured routinely in clinical practice [5]. Albumins function as the regulators of colloid osmotic pressure of blood, while globulin is known as immunoglobulin or antibody and secreted by B cells of the adaptive immune system [6], they involve in various sorts of physiological activities of human bodies.In recent years, many studies has explored the relationships between the AGR and the prognosis in cancers[7].Yasunori et al.[8]demonstrated low AGR level can predict poorprognosis in cervical cancer patients treated with radiation based therapy;while other scholars found AGR was an independent predictor of early recurrence in gastric cancer patients [9]. All these studies together indicate that the AGR is a novel independent survival predictor for patients with cancers.
However,the role of AGR in HC remains largely unknown.To explore the usefulness of AGR in HC patients.In this study,we firstly detected the optimal cut-off value of AGR,additionally, we examined the relationships between AGR and clinicopathological factors and investigated the prognosis value of AGR in HC patients.Lastly, we explored the correlations between AGR level and the incidence of postoperative complications.
Patients and methods Patients and information collection
Patients with HC and who underwent radical surgery atFirst Teaching Hospital of Tianjin University of TraditionalChinese Medicine and Tianjin Medical University Cancer Hospital between April 2010 and December 2016 were collected. After surgery, patients were followed every 3–6 months for 2 year,then every year or until death. The follow-up of all patients in this study was completed in September 2019.
Eligibility criteria for this study included the following:(1) histologically proven HC; (2) patients with detailed clinicopathological data, preoperative serum laboratory data and availability of complete follow-up data; (3) the patients were not subjected to radiation, chemical or biological treatment before potentially curative surgery was performed. Excluded criteria included the following: (1) patients with metabolic syndrome, diabetes, heart disease, hypertension, autoimmune disease, and infection within 3 months; (2) patients who died within 90 days of surgery and died from other diseases; (3)patients who underwent palliative surgery.
Evaluated variables
We collected data on gender, age, size of tumor, Bismuth-Corlette classification, differentiation, tumor stage, lymph node metastasis. Data for preoperative hematological variables were obtained for all enrolled patients within 3 days before surgery.The preoperative AGR=albumin/(total serum proteinalbumin). Postoperative complications were defined as any deviation from the normal postoperative course. Postoperative complications in our study was short term postoperative complications, those include bleeding, infection, bile leakage, intestinal leakage, postoperative intestinal adhesion, obstruction,et al.
Statistical analysis
With the log-rank analysis, we calculated the best cutoff values for AGR. Qualitative correlation analysis was performed by Chi-square test. Multivariate correlation analysis was conducted by logistic regression.
Univariate survival analysis was performed by using the Kaplan-Meier method. Cox regression analysis was used to estimate the independent risk factor of overall survival.P<0.05 was considered statistically significant. All statistical analyses were carried out using SPSS software 21.0.
II. RESULT
Patient characteristics
Based on inclusion and excluded criteria, 97 HC patients were eligible for this study. The 3-year survival rate of all enrolled patients was 38.1%. There were 72 males and 25 females, and median age of the patients was 59.2 years old(range 39–76); the median maximum tumor diameter was 3.9 cm. Regarding the Bismuth-Corlette classification, 35,37 and 25 HC patients were type I-II, type III and type IV,respectively; there were 32 patients with well/moderate differentiation and 65 patients with poorly differentiation.Based on the TNM staging system,17,21 and 59 patients were classified as T1,T2 and T3 stage,respectively;and 54 patients with lymph node metastasis. After radical surgery,43 patients showed with different short term postoperative complications.While another 54 patients had no postoperative complications.
The optimal cut-off value
We attempted to determine the optimal cut-off value of AGR through the log-rank analysis [10], the corresponding optimal cut-off value was identified as 1.34 for AGR. Consequently,patients were divided into two groups for further analysis.There were 49 patients with high AGR level, while other 48 patients with low AGR level.
Associations between AGR level and clinicalpathological factors
The AGR level in different gender, age, size of tumor,differentiation,Bismuth-Corlette classification,tumor stage and lymph node metastasis were analyzed. Chi-square test showed tumor stage(P=0.004)and lymph node metastasis(P=0.003)were related with AGR level. Logistic regression found tumor stage(OR=2,621;P=0.003)and lymph node metastasis(OR= 3.704;P= 0.004) were identified as independently risks of AGR level.Patients with a low AGR level were more likely to have more advanced tumor stages and lymph node metastasis than those with a low AGR level(Table 1).
Survival analysis
Univariate survival analysis showed significant relationships between the overall survival and size of tumor,differentiation,Bismuth-Corlette classification, tumor stage and AGR level(P<0.05),but not with gender,age,lymph node metastasis and postoperativecomplications(P>0.05).Furthermore,differentiation (HR=1.989; (P=0.014), tumor stage (HR=1.480; (P=0.014) and AGR level (HR=0.037; (P=0.017)were identified as the independent factors of the overall survival,following the multivariate analysis(Table 2).Patients with low AGR level exhibited a significantly shorter prognosis compared to those with high AGR level(Figure 1).
Associations between AGR level and postoperative complications
Postoperative complications occurred in 43 (44.3%) in all enrolled patients. Size of tumor(P=0.033),Bismuth-Corlette classification (P= 0.010) and AGR level (P= 0.006) were significantly associated with the incidence of postoperative complications by Chi-square test. Logistic regression showed Bismuth-Corlette classification (OR = 0.465,P= 0.011) and AGR level (OR = 0.037,P= 0.017) were independently associated with the incidence of postoperative complications(Table 3).
III. DISCUSSION
HC patients frequently show malnutrition, which can decrease capacity for treatment tolerance, increased mortality,and worse quality of life[11].Moreover,malnutrition has been found to be associated with an immuno-suppressed condition and led to inadequate antitumor immunity, which promote tumorigenesis by increasing tumor proliferation and metastasis,and exert immunosuppressive effects enables the escape of cancer cells from immunosurveillance [12]. Various markers,such as the neutrophil-lymphocyte ratio, platelet lymphocyte ratio, systemic immune-inflammation index, prognostic nutrition index, and prognostic index have been established the status of nutritional or inflammation.However,these indicators can not represent both nutritional and inflammation in clinical.Hence,AGR,a new biomarker can reflect nutritional status and inflammationhas, been been used recent years. Studies found AGR was conversely correlated to the tumor survival. The mechanisms maybe albumin was crucial for the drug delivery in chemotherapy, while globulins secreted by tumor-related cells were reported to promote tumor development, angiogenesis, immunosuppression, and metastasis [13].AGR was more significant and precise to demonstrate the prognostic effect than albumins and globulins in many malignant tumors [14].Zhang et al. [15] found AGR could be a useful and effective prognostic index for identifying the prognosis of hepatocellular carcinoma patients, and low AGR level was significantly associated with shorter overall survival in hepatocellular carcinoma patients. Similar results were reported for patients for colon cancer[16].Xu et al.[17]also reported AGR lev was an independent predictor of prognosis of glioblastoma,and AGR was an inexpensive and easy-to-perform indices for predicting overall survival with glioblastoma. A meta-analysis showed that higher AGR level was related to better overall survival and distant metastasis-free survival[18].AGR may be a promising indicator of prognosis for solid cancers.Low AGR was also reported to related with poor biological behaviors.Zhang et al. [19] also proved AGR level was significantly lower in patients with NSCLC with a larger tumor size,higher WBC and platelet counts, higher fibrinogen and D-dimer levels,which were related to tumor progression.Lin et al.[20]reported low AGR level was significantly associated with high alkaline phosphatase, gamma-glutamyl transpeptidase, total bilirubin levels and advanced TNM stages in patients with cholangiocarcinoma.However,the clinical significances of the AGR in HC have not been elucidated.
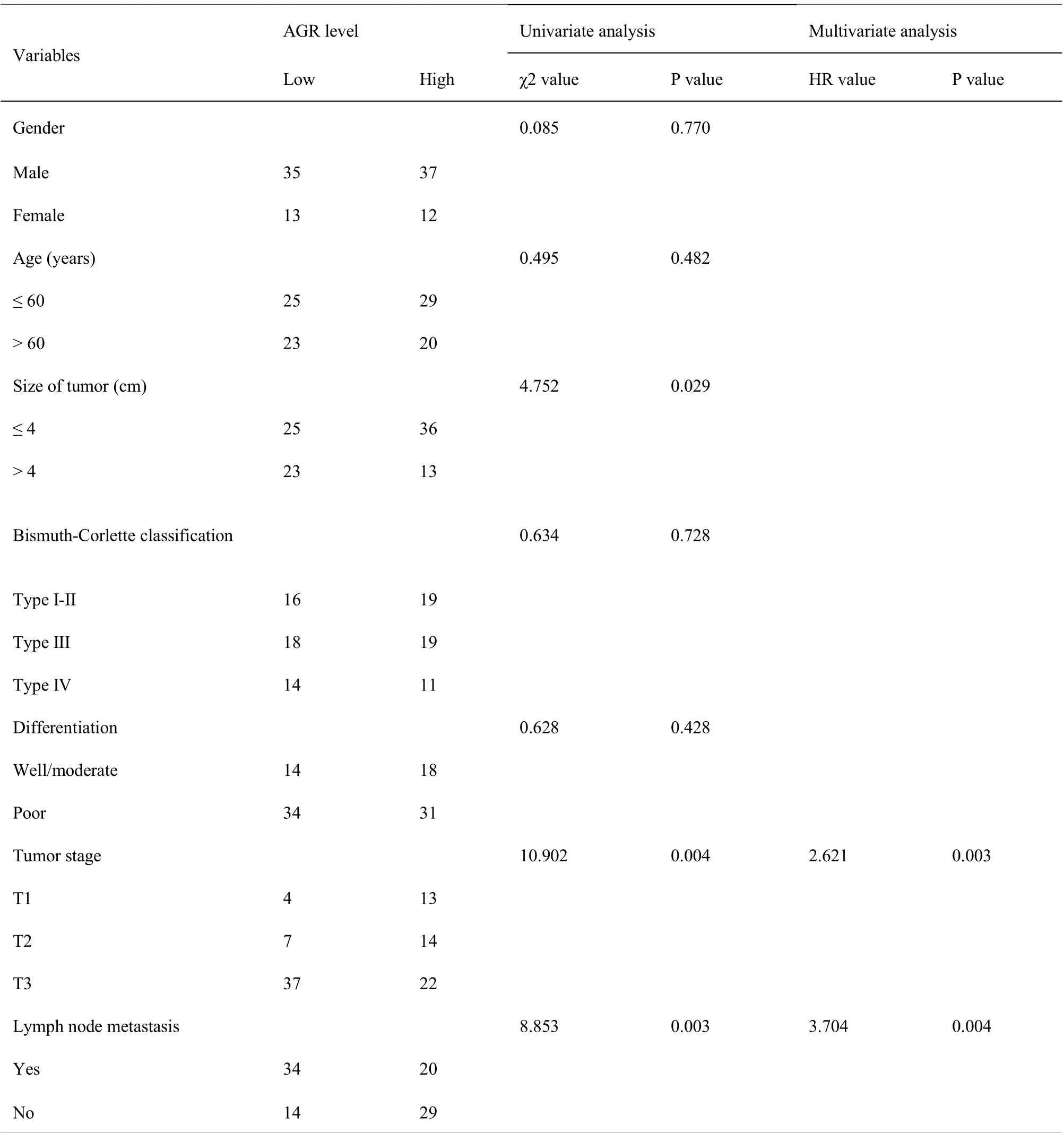
Table 1 Relationships between albumin-to-globulin ratio level and clinicopathological factors

Table 2 Univariate and multivariate analysis of overall survival in enrolled hilar cholangiocarcinoma patients
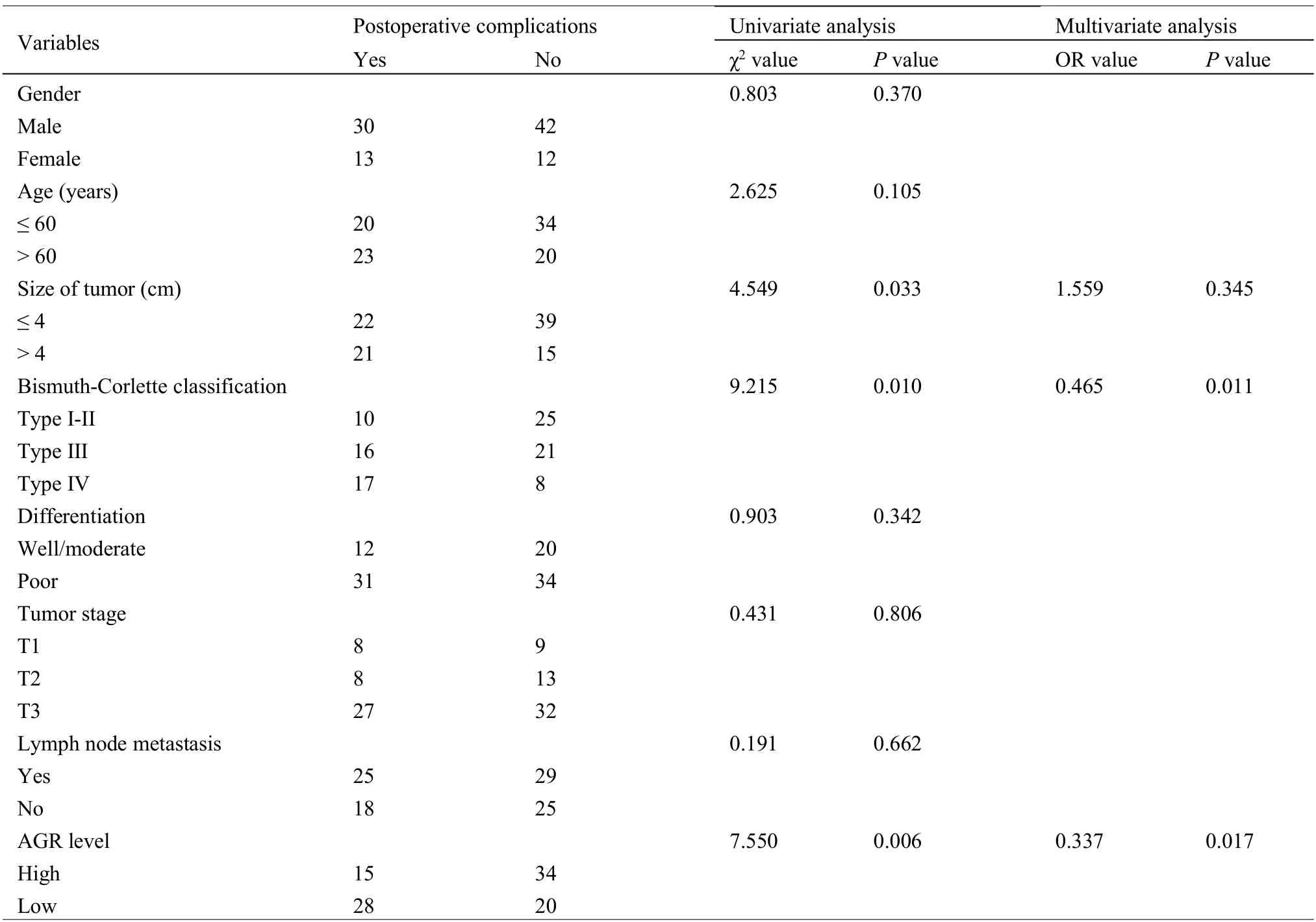
Table 3 Relationships between incidence of postoperative complications and clinicopathological factors in hilar cholangiocarcinoma patients
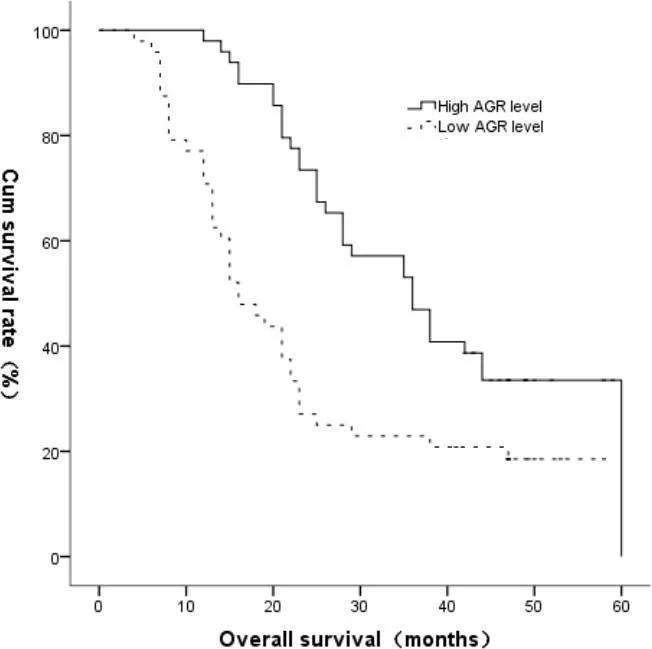
Fig.1.urvival curve of hilar cholangiocarcinoma patients according to albumin-to-globulin ratio level(low albumin-to-globulin ratio level or high albumin-to-globulin ratio level)
In the present study,we firstly detected the cutoff value for AGR. The optimal cutoff value of the AGR remained unclear up to now,the range of ARG was from 1.15-1.75 in different cancers [18]. By using log-rank analysis analysis, we found the optimal cutoff value for the AGR for our enrolled HC patients was determined to be 1.34, then 1.34 was set as the border level to divide high and low AGR groups. Besides the results mentioned above, the AGR level was analyzed for the correlations with clinicopathological factors, and we found patients with a low AGR level were more likely to have more advanced tumor stages and lymph node metastasis.AGR can be used to indicate the aggressive behaviors in HC patients.To assess the prognostic value of AGR level in HC, we analyzed AGR level using overall survival and Cox regression analysis. Our results demonstrated AGR level was identified as an independent factors of the overall survival,patients with low AGR level exhibited a significantly shorter overall survival. These findings suggested that HC patients with low AGR level may be a high-risk group, physicians should pay attention to peri-operative care for patients with a low AGR level. We suggested that AGR should be included in the routine assessment of HC patients.
A novel finding of this study was that the AGR level was associated with a higher risk of the incidence of short term postoperative complications in HC.As we know,postoperative complications after surgery often resulted in a significantly increased morbidity and mortality; postoperative complications also had a negative impact on the prognosis of cancers [21].Some nutritional status indexes had been demonstrated to be associated with the incidence of postoperative complications in digestive tract cancers. Mohri et al. [22] demonstrated that prognostic nutritional index was a useful predictor of postoperative complications in patients with colorectal cancer. For the complexity of radical surgery,postoperative complications occured with a higher incidence in HC. However, there was no reports on the relationship between the status of nutritional or inflammation and postoperative complications in HC. Our results suggested that postoperative complications occurred more frequently in the low AGR level group and the logistic regression demonstrated that AGR level was an independently factor associated with the incidence of postoperative complications. Hence, AGR may be used clinically to identify patients at increased risk for postoperative complications.
In conclusion, our results suggested that preoperative AGR may be used clinically not only to identify patients at increased risk for postoperative complications, but also to predict longterm survival as a simple and useful biomarker.
Acknowledgments:
This work was supported by Scientific Research Project of Tianjin Municipal Education Commission(No.2018KJ015).
Competing interests:
The authors declare no conflicts of interest.
Abbreviations:
HC,hilar cholangiocarcinoma;AGR,albumin-to-globulin ratio
Citation:
Liu HG, Yong L, Jia YJ. The predictive value of preoperative albumin-to-globulin ratio in patients with hilar cholangiocarcinoma. Prec Med Res. 2021;3(2):6. doi:10.12032/PMR2021060801.
Executive editor:Na Liu.
Submitted:17 March 2021,Accepted:19 April 2021,Online:10 May 2021.
© 2021 By Authors. Published by TMR Publishing Group Limited. This is an open access article under the CC-BY license(http://creativecommons.org/licenses/BY/4.0/).
 Precision Medicine Research2021年2期
Precision Medicine Research2021年2期
- Precision Medicine Research的其它文章
- Myeloid-derived suppressor cells as a therapeutic target in lung cancer
- Targeting mitochondrial protein transport system:a promising treatment strategy for heart failure?
- Expression and molecular mechanism of PCNA,Caspase-3,IL-6 and Survivin proteins in chorionic villi and decidual tissue of early embryo damage
- Expression and clinicopathologic significance of RASSF1A and WT1 in recurrent epithelial ovarian cancer
