Erosive Pustular Dermatosis of the Scalp After Excision and Skin Grafting of Scalp Squamous Cell Carcinoma
Xun He∗, Chao-Qun Wang, Wei Lu, Yu-Gang Gong, Xiao-Wei Sha, Zhu Shen
Department of Dermatology, Sichuan Provincial People’s Hospital, Chengdu, Sichuan 610071, China.
Abstract
Introduction: Erosive pustular dermatosis of the scalp (EPDS) is an uncommon condition with unknown etiology.The clinical exclusive diagnosis needs to be differentiated from similar diseases.
Here, we present a case of EPDS after surgical treatment of scalp squamous cell carcinoma.
Case presentation: A 68-year-old woman presented with an eight-month history of a chronic scalp eruption.She had been diagnosed as squamous cell carcinoma by biopsy nine months ago, and had been treated by surgical excision and skin grafting. One month later, she was referred for evaluation of the newly enlarged lesion which was observed at the skin grafting site. She was diagnosed of EPDS based on characteristics of lesions, clinicopathological findings and laboratory data. The condition had clinically improved with systemic steroid therapy and topical tacrolimus for two weeks. Relapses occurred after complete withdrawal of both treatments. After repeating the above therapy and applying topical tacrolimus as maintenance therapy, the condition was well controlled at the one-year follow-up.
Discussion: EPDS is an uncommon inflammatory dermatosis with main incidence rate of elderly patients and female predominance. The diagnosis of EPDS cant be made only by histopathological examination, which is helpful for differential diagnosis. Microbiological investigations commonly remain negative. For the high risk of relapse, it is important for clinicians to be aware of maintenance treatment and a long-term management.
Conclusion: It should be recognized by clinicians that EPDS is an uncommon and relapse disease, leading to serious cosmetic problems. The treatment lacks evidence-based medicine data, clinician should choose the appropriate therapy according to the condition of patients.
Keywords: case report, erosive pustular dermatosis, squamous cell carcinoma, surgical excision, skin graft
Introduction
Erosive pustular dermatosis of the scalp (EPDS) is an uncommon condition that tends to occur mainly in patients of advanced age and shows a significant female predominance. Clinically, EPDS is characterized by the presence of pustules, chronic crusted erosions with progressive scarring alopecia, and skin atrophy with an unknown origin. It may be triggered by local trauma, skin grafting, ultraviolet light exposure, cryotherapy, radiotherapy, drugs, autoimmune disease, or genodermatosis. We herein present a case of EPDS after surgical excision and skin grafting for treatment of scalp squamous cell carcinoma.
Case report
A 68-year-old woman presented with an eight-month history of a chronic scalp eruption characterized by erythema, pustules with erosion, crusting, and hair loss.She reported a chronic ulcer present on the vertex of her scalp for more than two years, and had been diagnosed as squamous cell carcinoma by biopsy nine months before presentation to our hospital. The squamous cell carcinoma was treated by surgical excision and skin grafting. One month after treatment, multiple erythematous, pustular,exudative, and erosive lesions were observed at the skin grafting site. She felt mild itching without pain or burning.Despite treatment with topical antibiotics, the lesions gradually enlarged. She was referred to us for evaluation of the eruption.
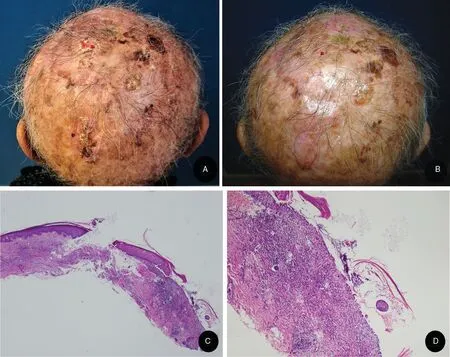
Figure 1. Clinical appearance and histopathological results of the lesions on the scalp from the patient with erosive pustular dermatosis of the scalp. (A) Diffuse crusts, erythema, pustules, erosions, and scarring alopecia. (B) After two weeks of treatment with oral steroid and topical tacrolimus. (C) Slight epidermal hyperplasia, focal erosions, a mixed inflammatory infiltrate, absent hair follicles, and prominent dermal fibrosis(hematoxylin–eosin stain ×40). (D) Intradermal mixed inflammatory cells, including large numbers of lymphocytes and neutrophils and minimal numbers of plasma cells (hematoxylin–eosin stain ×100).
Physical examination revealed no evidence of lymphadenopathy in the head and neck. Large numbers of superficial moist erosions and erythema covered with yellow-brown keratotic crusts were seen on the scalp. A few pustules were distributed on the erythematous skin and surrounded the erosions. Atrophy of the affected skin with scarring alopecia was seen on the scalp (Fig. 1A).Laboratory examinations revealed no significant abnormalities in blood and urine tests, liver and kidney function,and blood glucose level. Bacterial smear cytology, fungal microscopy, and bacterial and fungal culture evaluations were all negative. Histopathological examination of a specimen showed thinning of the epidermis with partial erosion, necrosis, and localized focal heterotypic hyperplasia. The intradermal elastic fibers were degenerated.Large numbers of lymphocytes and neutrophils and minimal numbers of plasma cells were infiltrated within the dermis. Ruptured hair follicles were also present with perifollicular infiltration of lymphocytes and histiocytes.The hair follicles appeared to be absent (Fig. 1C and 1D).Direct immunofluorescence was negative.
Based on these clinicopathological findings and laboratory data, a diagnosis of EPDS was made. According to the timing of the clinicalmanifestation and anamnestic data, we inferred that the disease was associated with the history of surgical excision and skin grafting for treatment of the squamous cell carcinoma. Treatment included systemic steroid therapy with prednisone at 0.75mg/kg and topical tacrolimus twice a day. After two weeks, the condition had clinically improved. No new lesions had developed on the scalp. The crusting, erosive lesions were significantly reduced and the pustules were almost cleared (Fig. 1B).The prednisone was then gradually tapered by 5mg per week until withdrawal, but the topical tacrolimus was continued. After three months of treatment, the condition was practically cured with scarring and cicatricial alopecia.Relapses occurred after complete withdrawal of both treatments. After repeating the above therapy and applying topical tacrolimus twice daily as maintenance therapy, the condition was well controlled at the one-year follow-up.
Discussion
EPDS is an uncommon inflammatory dermatosis of unknown etiology. This condition was first described in 1977 by Burton and in 1979 by Pye et al.1It tends to occur most commonly in the elderly. A type of infantile EPDS that occurred in association with Klippel–Feil syndrome was observed in a six-month-old girl. Another nine-yearold child developed EPDS after aplasia cutis congenita.EPDS exhibits female predominance with a female:male ratio of approximately 2:1. Evidence shows that in postmenopausal women, estrogen loss is accompanied by many skin changes, including atrophy and delayed wound healing.
The clinical manifestations of EPDS are diffuse erythema with coverage of the moist eroded surface by crusting and superficial pustules, which can cause scarring alopecia and skin atrophy. Histopathological examination shows subcorneal pustules, epidermal hypertrophy, or atrophy and erosions. Intradermal mixed inflammatory cells include infiltration of a variety of cells, such as neutrophils,lymphocytes, and plasma cells. Hair follicles are reduced or absent. Minimal leukocytoclastic vasculitis might be present near the erosions and ulcerations. Notably, a recent study showed that a neutrophilic spongiotic infundibular pustule was observed in 8 of 30 cases.2Microbial and mycological investigations remained negative. EPDS presents no pathognomonic laboratory or histopathological findings; it is a clinical diagnosis of exclusion. The main differential diagnoses include severe bacterial or fungal infections, pustular psoriasis, subcorneal pustular dermatosis, immunoglobulin A pemphigus, cicatricial pemphigoid, dissecting cellulitis of the scalp, folliculitis decalvans, field cancerization of squamous cell carcinoma, basal cell carcinoma, and hypertrophic actinic keratosis.
The etiology and exact pathogenesis of EPDS are still unclear.Some authors believe that EPDS is an inflammatory skin disease,while others consider that immune dysfunction is the main mechanism. Various predisposing factors, such as trauma, skin grafting, or skin damage, may be triggered by the production of inflammatory cytokines by keratinocytes or in a manner that mimics the Koebner phenomenon.3Other potential factors include radiation therapy,cryotherapy, sun exposure, or drugs (e.g., imiquimod,ingenol mebutate, epidermal growth factor receptor inhibitors, latanoprost, or 5% minoxidil solution). EPDS may be associated with autoimmune disorders such as rheumatoid arthritis and myasthenia gravis, and genetic skin conditions and syndromes, such as aplasia cutis congenita, Kindler syndrome, and myelodysplastic syndrome. Frequent comorbidities of EPDS reportedly include coronary artery disease, cerebrovascular insult, arterial hypertension, diabetes mellitus, and severe cases of cancer.The rarity of EPDS and the scarce literature data impede the establishment of a treatment algorithm for the disease.Semkova et al.4divided the treatment of EPDS into three lines of therapy. The first line was a high-potency topical corticosteroid or calcineurin inhibitor, the second line was an oral corticosteroid and topical calcipotriol, and the third line was oral acitretin. High-potency topical corticosteroids have been used in most reported cases with considerable efficacy. However, considering their adverse effects, they tend to be discontinued, and treatment is initiated with topical tacrolimus after improvement. Topical tacrolimus can be used either as monotherapy, in combination with topical steroids, or as a maintaining treatment after an initial course of topical steroids. The advantage of tacrolimus over topical corticosteroids is that it does not cause skin atrophy.EPDS that had undergone failed treatment with oral,intralesional, or topical steroids, tacrolimus, and antibiotics.
The role of photodynamic therapy in EPDS is still controversial. Guarneri and Vaccaro5 applied methyl aminolevulinic acid cream with 630-nm photodynamic therapy in two separate treatments at a one-week interval,and very good results were achieved by week 12. Yang et al.6performed gentle curettage followed with photodynamic therapy in eight patients with EPDS. Two of the patients developed residual lesions, and one patient relapsed. Retreatment with a second cycle of the above procedure was successful. López et al.7described an 81-year-old woman who presented with EPDS after photodynamic therapy for actinic keratosis. Photodynamic therapy should be used with caution in light of conflicting reports.
In general, EPDS is a chronic disease that requires longterm management, especially with topical drugs, and it has a high risk of relapse. Therefore, maintenance treatment with a topical calcineurin inhibitor has been recommended, and more experience is needed to establish effective treatment.
- 国际皮肤性病学杂志的其它文章
- Circulating MicroRNAs as Potential Biomarkers in the Diagnosis of Neurosyphilis: A Case Control Study
- NCSTN Gene Silencing Inhibits the Retinoic Acid Signaling Pathway in Human Immortalized Keratinocytes
- A Clinical Retrospective Analysis of 340 Inpatients With Malignant Skin Tumors in Western Inner Mongolia
- Subepidermal Autoimmune Bullous Disease Associated With Monoclonal Gammopathy of Unknown Significance and Unexpected Positive Direct Nikolsky Phenomenon: A Case Report
- Nicolau Syndrome Following Metamizole Injection: A Case Report
- A Study of Normal Epidermal Melanocyte Distribution