Subepidermal Autoimmune Bullous Disease Associated With Monoclonal Gammopathy of Unknown Significance and Unexpected Positive Direct Nikolsky Phenomenon: A Case Report
Gamze Tas¸-Aygar1,∗, Müzeyyen Gönül1, Aysun Gökçe2, Münire Çagın2
1Dermatology Clinic, 2Pathology Clinic, University of Health Sciences, Dıs¸kapı Yıldırım Beyazıt Training and Research Hospital,Ankara 06110, Turkey.
Abstract
Introduction: Numerous dermatoses associated with monoclonal gammopathy have been reported in the literature. Subepidermal autoimmune bullous diseases (SABD) are one of them which were not common.Here we report a case of SABD associated with MGUS who had a severe mucosal involvement and unexpected positive direct Nikolsky phenomenon.
Case presentation: A 68-year-old male patient was admitted to our clinic with erosions on the oral mucosa,tense blisters, erosions, and ulcers on the trunk and extremities. Subepidermal vesicle formation was detected in the skin biopsy. Clinical examination revealed positivity for the Nikolsky phenomenon. The disease was unresponsive to conventional treatments and dysphagia and hoarseness occurred. The patient was screened for malignancy due to his unresponsiveness to the treatments and his severe oral mucosal involvement. Ig-G MGUS was detected in the patient.
Discussion: The Nikolsky sign is an indicator of acantholysis and is known as a specific finding for pemphigus.However, when we look at gammopathy-associated autoimmune bullous dermatoses, skin fragility has been reported in cases. However, the meaning of fragility is not explained. The diagnosis of all these patients was Ig-M MGUS. Our patient was presented because of non-IgM MGUS, direct Nikolsky positivity, and severe mucosal involvement.
Conclusion: Nikolsky positivity may be a clue for gammopathy-related subepidermal autoimmune bullous diseases.
Keywords: subepidermal autoimmun bullous diseases, gammopathy, MGUS, Nikolsky phenomenon, case report
Introduction
Monoclonal gammopathy of unknown significance (MGUS)is a plasma cell dyscrasia that often precedes multiple myeloma, which is common in people of advanced age The most common skin abnormalities associated withMGUSare scleromyxedema, scleredema, flat xanthomas, necrobiotic xanthomas, Schnitzler syndrome, erythema elevatum diutinum, and subcorneal pustular dermatosis. Association with subepidermal autoimmune bullous diseases (SABDs) such as bullous pemphigoid (BP) and epidermolysis bullosa acquisita has been reported in a few cases of MGUS.1We herein present a case of an SABD associated with MGUS characterized by severe mucosal involvement and an unexpected positive direct Nikolsky phenomenon.
Case report
A 68-year-old man presented with multiple areas of erosion and tense blisters on his body. His medical history included type 2 diabetes mellitus, loss of vision in one eye, hypertension, chronic renal disease, hypercholesterolemia, and hepatitis B carriage. Physical examination revealed 1.0- to 1.5-cm bullae and numerous areas of erosion with an erythematous base on the scalp, upper chest, back, and bilateral forearms and legs; two 1.0-cm erosions were also present on the cheek and lip mucosa.Positive indirect and direct Nikolsky signs were found in the skin with and without lesions (Fig. 1). Anti-desmoglein antibodies were negative. Histopathological examination revealed subepidermal vesicle formation with associated mixed lymphocytic and eosinophilic inflammation direct immunofluorescence showed deposition of immunoglobulin (Ig) G along the basement membrane (Fig. 2). Neither the salt-split technique nor immunoblotting tests could be performed because they were unavailable in our hospital.Anti-type VII collagen antibody levels and BP180 and BP230 antigen levels could not be evaluated because of the patient’s financial limitations.
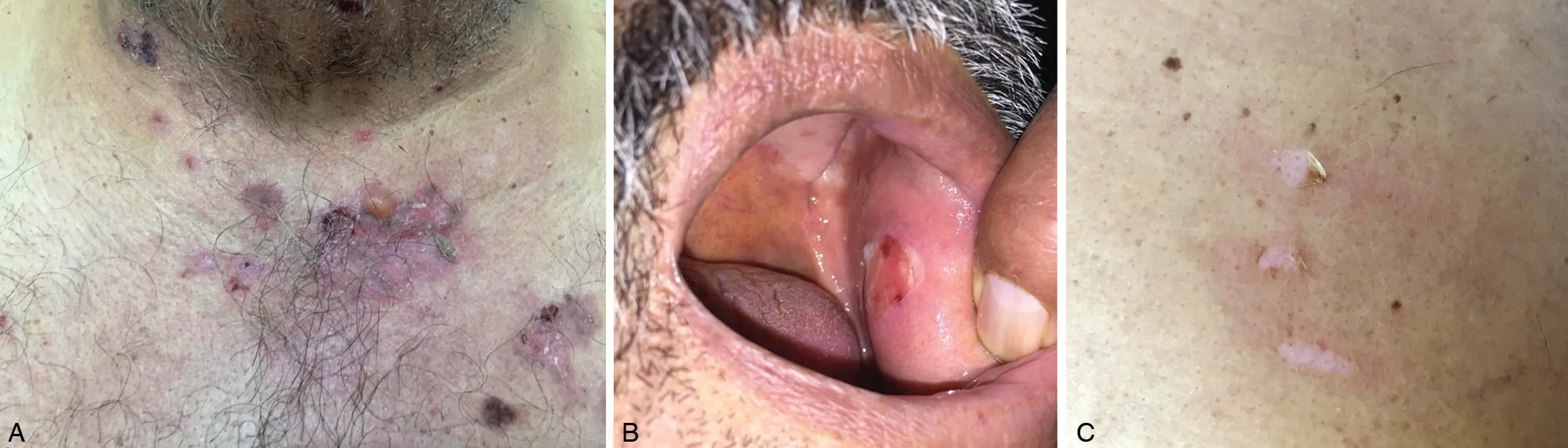
Figure 1. Clinical presentation of the subepidermal autoimmune bullous disease patient with monoclonal gammopathy ofunknown significance and unexpected positivedirect nikolsky phenomenon.(A) Tense bullae and areas of erosion with an erythematous base.(B) A 1-cmeroded plaque around the cheekmucosa with bulla residue.(C) Three areas of direct Nikolsky positivity in the lesion-free area of the back(erythema due to friction).
The patient was determined to have an SABD, and entecavir treatment was started with methylprednisolone at 96mg/day and mycophenolate sodium (MNa) at 1,440mg/day. Despite this treatment, the mucosal lesions continued to increase, and dysphagia and hoarseness newly developed.The dose ofmethylprednisolonewas reduced to 80mg and that of MNa was reduced to 1,080mg because of the development of mood changes, depressive symptoms,increased creatinine, leukopenia (3,100/dL), and thrombocytopenia (37,000/dL). Intravenous Ig treatment was started because the drug doses could not be further increased and mucosal involvement was severe. The patient was screened formalignancy because of severe and prolonged diarrhea and an unexpected clinical course. No malignancy was detected on either thoracoabdominal tomography or colonoscopy.Because the thrombocytopenia did not improve despiteMNa discontinuation, protein electrophoresis was performed and IgGmonoclonal gammopathywas detected. A bone marrow biopsy showed that the plasma cell concentration was<10%; therefore, the patient was diagnosed with non-IgM MGUSand followedup in the hematology department till the writing and the patient gave his agreement for the case publication.
Steroid and intravenous Ig treatments were combined with topical clobetasol propionate under occlusion and intralesional steroid injections for resistant lesions; the lesions then started to regress.
Discussion
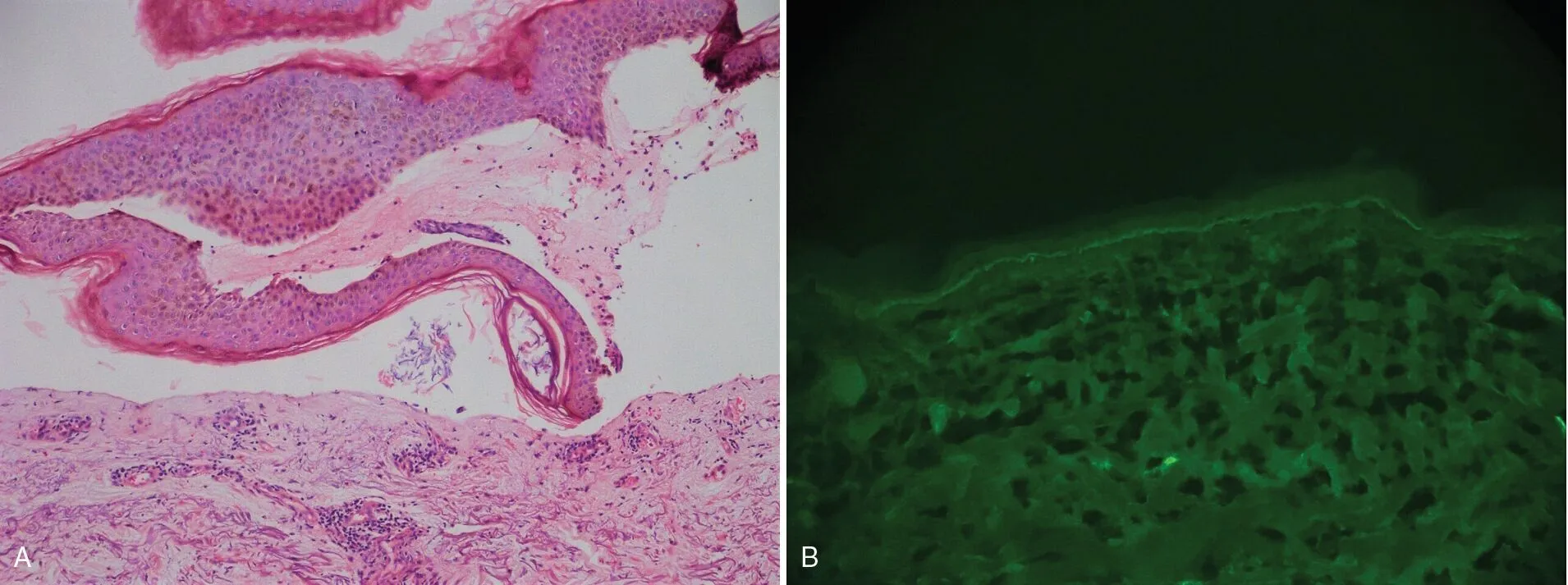
Figure 2. Pathological characteristics of the subepidermal autoimmunebullous disease patientwithmonoclonalgammopathyofunknownsignificance and unexpected positivedirect nikolsky phenomenon. (A) Subepidermal dissociation and perivascular mild inflammation of the dermis with fibrin and a small accumulation of nuclear debris (×10, hematoxylin and eosin). (B) Linear immunoglobulin G deposition along the basal membrane.
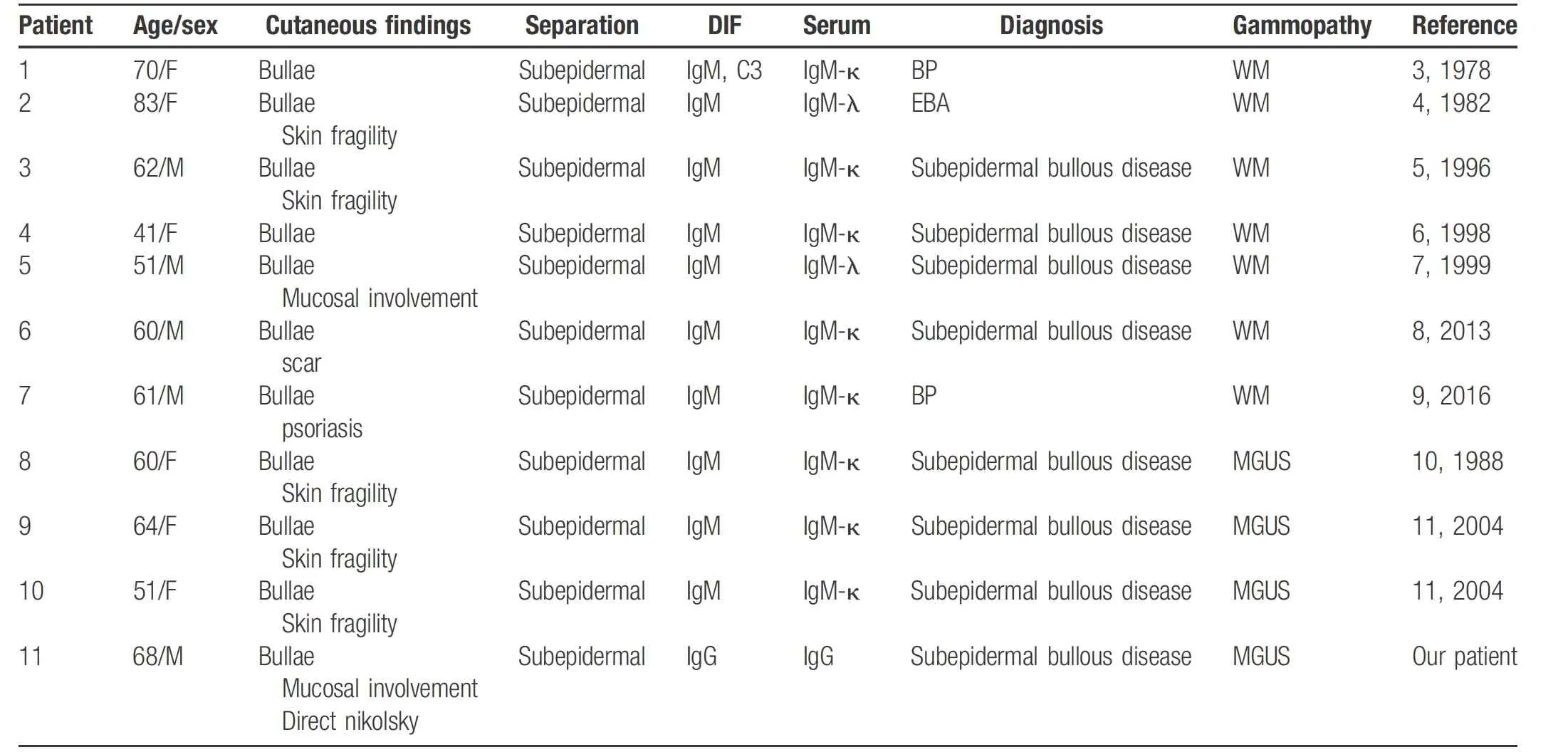
Table 1 Subepidermal autoimmune bullous diseases seen in patients with monoclonal gammapathy
Associations between SABD and gammopathy are very rare, and whether a real relationship exists between the two diseases is controversial. To our knowledge, 10 cases of SABDwith monoclonalgammopathy have been reported to date (Table 1). A definitive diagnosis of Waldenström macroglobulinemia was identified in three patients(two had BP and one had epidermolysis bullosa acquisita); however,the other seven cases could not be diagnosed accurately.Only three of the 10 cases were accompanied byIgMMGUS and defined as SABD. None of the patients withMGUS had mucosal lesions;2–8in contrast, our patient had severe mucosal lesions. This difference in mucosal involvement compared with cases described in the literature may be explained by the presence of non-IgMMGUS in our patient.An association between SABD and non-IgMMGUS has not been previously reported. The present case suggests that MGUS-associated SABDs have common features such as an unusual course and inability to distinguish the underlying SABD, suggesting that the association is not incidental.
The direct Nikolsky sign is indicative of active acantholysis. Although the indirect Nikolsky sign may be positive in some patients, the direct Nikolsky sign is almost always negative in patients with SABDs. Uzun and Durdu9 examined 123 patients with bullous disease and concluded that the direct Nikolsky sign was specific to pemphigus.Although our patient hadSABD, he showed a positive direct Nikolsky sign.
Skin fragility has also reportedly been detected in some patients with gammopathy-associated SABD (all patients with MGUS); however, the definition of skin fragilitywas not provided.1,6–8Direct Nikolsky positivity in these patients might be an important finding to support the gammopathybullous disease relationship, or it may be an exceptional finding because of the non-IgM MGUS in our patient.
In conclusion, the similar aspects between our case and MGUS-related bullous diseases reported in the literature suggest that this relationship is not incidental. Unlike the cases reported to date, our patient’s condition was uniquely associated with non-IgM MGUS, direct Nikolsky positivity, and severe mucosal involvement.
- 国际皮肤性病学杂志的其它文章
- Understanding of Melanocyte Distribution in Skin
- Epidural Block Treatment on Postherpetic Neuralgia and Comorbid Spine Metastasis of Malignant Tumor: Two Cases of Report
- Role of Tight Junctions and Their Protein Expression in Atopic Dermatitis
- Consensus on the Diagnosis and Treatment of Vitiligo in China (2021 Revision)#
- Guidelines for Diagnosis and Treatment of Atopic Dermatitis in China (2020)#
- Calcified Epidermal Cyst on the Neck