Nicolau Syndrome Following Metamizole Injection: A Case Report
Dilek Mentes¸oglu1,∗, Hamidullah Khurami1, Ays¸en Karaduman1, Özay Gököz2
1Department of Dermatology and Venereology, School of Medicine, Hacettepe University, Ankara 06100, Turkey, 2Department of Medical Pathology, School of Medicine, Hacettepe University, Ankara 06100, Turkey.
Abstract
Introduction: Nicolau syndrome is a rare complication following intramuscular injections of various drugs. It is characterized by severe pain, skin and sometimes muscle necrosis after drug injection. However the pathogenesis of Nicolau syndrome remains unclear.
Here, we report a case of Nicolau syndrome following metamizole injection.
Case presentation: A 35-year-old female presented with an painful necrotic ulcer who developed Nicolau syndrome after an intramuscular injection of metamizole in her right thigh due to reccurent episodes of back pain. This reaction is typical for Nicolau syndrome.
Discussion: The most common finding of Nicolau syndrome in the early period was severe pain at the injection site.Other common findings were skin discoloration, tenderness, and swelling; indurated livedoid plaques; and erythematous, ecchymotic and purpuric patches. The histopathological results of the case with Nicolau syndrome showed formation of ulceration and fat necrosis.
Conclusion: Although Nicolau syndrome is an uncommon cutaneous adverse reaction, clinicians should be aware of this complication to prevent or minimize the severity of Nicolau syndrome.
Keywords: nicolau syndrome, embolia cutis medicamentosa, metimazole
Introduction
Nicolau syndrome (NS) is a rare form of iatrogenic cutaneous necrosis that occurs at the site of an injection.NS, also known as livedo-like dermatitis and embolia cutis medicamentosa, is characterized by acute, severely painful,and localized erythematous-ecchymotic reticular lesions following an injection.1Although conventionally associated with intramuscular injections, it can also occur following subcutaneous or parenteral drug injections.2NS often leads to necrotic ulcers and scarring in multiple tissue layers (cutaneous, subcutaneous, and muscular).1Herein we describe a 35-year-old female diagnosed as NS following intramuscular injection of metamizole.
Case report
A 35-year-old female presented with a painful necrotic ulcer on her right thigh. She reported that it had appeared 10 days after an intramuscular injection of metamizole in the laterofemoral region of her right thigh for treatment of recurrent episodes of back pain. Anamnesis showed that she had a lumbar hernia and frequently used a nonsteroidal anti-inflammatory drug (metamizole sodium). Although having received similar injections in the past, she reported that this was the first time she had developed such a reaction.
Dermatological examination showed an erythematous ulcerated plaque on the right thigh (Fig. 1A). Her complete blood count, erythrocyte sedimentation rate, C-reactive protein concentration, total creatine kinase concentration,and coagulation parameters were normal. The patient underwent wound debridement, and tissue samples were collected from the lesioned area for aerobic and fungal cultures. The cultures grew Pseudomonas stutzeri and Aeromonas hydrophila/caviae. NS was considered in light of the patient’s history and clinical presentation; however,a deep incisional biopsy was performed to exclude other causes of ulcers, especially pyoderma gangrenosum.Histopathological examination of the tissue specimen showed ulceration and fat necrosis (Fig. 1C).
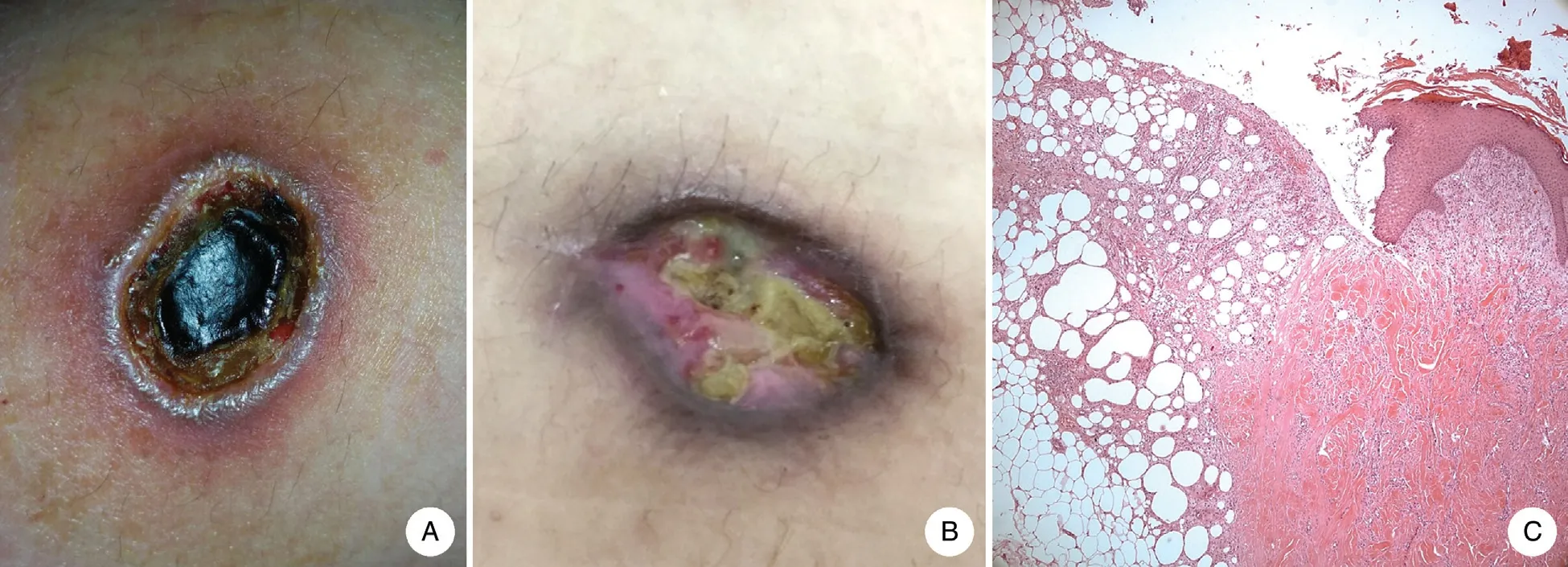
Figure 1. Clinical presentation of the lesion from the patient with Nicolau syndrome. (A) Ulcerated plaque with a dry erythematous midcircumference on the front of the patient’s right thigh. (B) The lesion 21 days after debridement. (C) Histological features of the lesion from the patient with Nicolau syndrome. The ulcer depth reached the subcutaneous tissue (hematoxylin and eosin,×10).
The patient’s clinical and histopathological findings were consistent with NS. She was prescribed oral amoxicillin and clavulanic acid, ciprofloxacin, and topical fusidic acid for 10 days. This treatment resulted in a significant reduction in both pain and lesion size at the 21-day follow-up (Fig. 1B). The patient provided written informed consent to have these data published.
Discussion
NS was first described in 1925 as occurring after intramuscular injections of bismuth salts for syphilis.3To date, numerous drugs have been reported to be associated with NS. Additionally, NS has been associated with intramuscular, subcutaneous, intravenous, and intraarticular injections of drugs such as cyanocobalamin(vitamin B12), lidocaine, vitamin K, etanercept, interferon β, meperidine, salicylate bismuth, glatiramer acetate,thiocolchicoside, nonsteroidal anti-inflammatory drugs(naltrexone, ketorolac, ketoprofen, ibuprofen, diclofenac sodium, piroxicam, phenylbutazone, and salicylamide),antibiotics (gentamycin, benzathine penicillin, tetracycline, streptomycin, penicillin G, and sulfapyridine),antihistamines (chlorpheniramine maleate, diphenhydramine, and hydroxyzine), antipsychotics (phenobarbital and chlorpromazine), corticosteroids (cortivazol, hydrocortisone, paramethasone, dexamethasone, and triamcinolone), vaccines (polio-Hib and diphtheria-pertussistetanus), calcium hydroxide, and mesotherapy injections.4
In previously reported cases, the most common finding in the early period was severe pain at the injection site.Other common findings were skin discoloration, tenderness, and swelling; indurated livedoid plaques; and erythematous, ecchymotic and purpuric patches.2It is important for clinicians to be aware of the early signs of NS to prevent or minimize tissue necrosis.
If skin findings are not recognized early and proper treatment is not initiated in a timely manner, complex operations may be required for treatment of extensive tissue necrosis, which can lead to permanent injury and organ loss. In the present case, timely wound debridement and appropriate systemic antibiotic treatment were administered.
In conclusion, although NS is an uncommon cutaneous adverse reaction, clinicians should be aware of this complication and its role as a potential adverse effect of commonly prescribed agents. This case report highlights the importance of early recognition of the cutaneous signs of NS because timely management can prevent morbidity.
- 国际皮肤性病学杂志的其它文章
- Circulating MicroRNAs as Potential Biomarkers in the Diagnosis of Neurosyphilis: A Case Control Study
- NCSTN Gene Silencing Inhibits the Retinoic Acid Signaling Pathway in Human Immortalized Keratinocytes
- A Clinical Retrospective Analysis of 340 Inpatients With Malignant Skin Tumors in Western Inner Mongolia
- Subepidermal Autoimmune Bullous Disease Associated With Monoclonal Gammopathy of Unknown Significance and Unexpected Positive Direct Nikolsky Phenomenon: A Case Report
- A Study of Normal Epidermal Melanocyte Distribution
- Erosive Pustular Dermatosis of the Scalp After Excision and Skin Grafting of Scalp Squamous Cell Carcinoma