盐酸麻黄碱皮下浸润联合晶体共负荷预防剖宫产腰麻后低血压的效果分析
张雪苗 岳圆圆 赵文琪 范修颖 张月顺

【摘要】 目的:觀察盐酸麻黄碱与1%利多卡因混合皮下逐层浸润联合晶体液共负荷预防剖宫产产妇腰麻后低血压的效果以及对新生儿的影响。方法:选取牡丹江市妇女儿童医院2019年10月-2020年1月收入院的60例择期在腰麻下行剖宫产产妇。根据电脑生成的随机数字,按随机数字表法将产妇随机分为C组和E组,每组30例。C组采用晶体共负荷,E组采用晶体共负荷联合盐酸麻黄碱皮下浸润。比较两组各时间点MAP、HR水平和并发症发生情况。比较两组静脉应用盐酸麻黄碱剂量,比较两组新生儿的酸中毒及Apgar评分情况。结果:T4~T8,E组的MAP均明显高于C组,差异均有统计学意义(P<0.05);T0~T3,两组的MAP、HR比较,差异均无统计学意义(P>0.05);T4~T8,两组的HR比较,差异均无统计学意义(P>0.05)。E组低血压发生率为33.3%,低于C组的63.3%,差异有统计学意义(P<0.05);E组恶心发生率为13.3%,低于C组的36.7%,差异有统计学意义(P<0.05);两组反应性高血压、呕吐发生率比较,差异均无统计学意义(P>0.05);C组静脉应用盐酸麻黄碱的总剂量明显高于E组,差异有统计学意义(P<0.05)。E组的pH明显高于C组,碱剩余、乳酸均明显优于C组,差异均有统计学意义(P<0.05);新生儿的1、5 min Apgar评分比较,差异均无统计学意义(P>0.05)。结论:盐酸麻黄碱皮下浸润联合晶体液共负荷用于预防腰麻后低血压,血流动力学稳定,无明显反应性高血压,对新生儿影响较小,可以作为一种安全、有效的预防手段。
【关键词】 低血压 蛛网膜下腔麻醉 剖宫产 盐酸麻黄碱 晶体共负荷
[Abstract] Objective: To observe the effect of Ephedrine Hydrochloride and 1% Lidocaine mixed subcutaneous layer by layer infiltration combined with crystal co-loading on the prevention of hypotension after lumbar anesthesia in cesarean section parturients and its effect on neonates. Method: A total of 60 parturients who received cesarean section under lumbar anesthesia were selected from Mudanjiang Women’s and Children’s Hospital from October 2019 to January 2020. According to the computer generated random numbers, the parturient women were randomly divided into group C and group E according to the random number table method, 30 cases in each group. Group C was treated with crystal co-loading, while group E was treated with crystal co-loading combined with Ephedrine Hydrochloride subcutaneous infiltration. MAP, HR level and complications were compared between the two groups at each time point. The dose of intravenous Ephedrine Hydrochloride was compared between the two groups, the acidosis and Apgar score of neonates in the two groups were compared. Result: T4 to T8, the MAP of group E were significantly higher than those of group C, the differences were statistically significant (P<0.05). T0 to T3, comparison of MAP and HR between the two groups, there were no statistical significance between the two groups (P>0.05). T4 to T8, comparison of HR between the two groups, there were no statistically significant differences (P>0.05). The incidence of hypotension in group E was 33.3%, which was lower than 63.3% in group C, the difference was statistically significant (P<0.05). The incidence of nausea in group E was 13.3%, compared with 36.7% in group C, the difference was statistically significant (P<0.05). The incidences of reactive hypertension and vomiting were compared between the two groups, the differences were not statistically significant (P>0.05). The total dose of intravenous Ephedrine Hydrochloride in group C was significantly higher than that in group E, the difference was statistically significant (P<0.05). The pH of group E was significantly higher than that of group C, base excess and lactic acid were significantly better than those of group C, the differences were statistically significant (P<0.05). Comparison of 1 and 5 min Apgar scores between the two groups, there were no statistically significant differences (P>0.05). Conclusion: Ephedrine Hydrochloride subcutaneous infiltration combined with crystal co-loading can be used to prevent hypotension after spinal anesthesia, with stable hemodynamics and no obvious reactive hypertension, it has little effect on newborns, and can be used as a safe and effective prevention method.
[Key words] Hypotension Spinal anesthesia Cesarean delivery Ephedrine Hydrochloride Crystal co-loading
First-author’s address: Mudanjiang Medical University, Mudanjiang 157000, China
doi:10.3969/j.issn.1674-4985.2021.22.005
蛛网膜下腔麻醉又称腰麻,是产科麻醉的首选麻醉方式,而腰麻后低血压(spinal anaesthesia-induced hypotension, SAIH)是其最常见的不良并发症。SAIH可导致产妇术中出现恶心、呕吐等,严重的低血压还会导致产妇循环功能障碍、胎儿缺血、缺氧、酸中毒,甚至危及产妇及胎儿生命[1-2]。SAIH的定义和监测手段尚存在争议,SAIH的发生率达30%~100%[3-5]。目前,体位干预、晶体液或胶体液共负荷/预负荷、应用血管活性药物等方法在治疗和预防SAIH方面都展现出不同效果。但是,液体预扩容或者体位干预预防SAIH,临床效果欠佳,通常需要使用补救性血管活性药物[6-7]。麻黄碱是产科麻醉中常用的血管收缩药物之一,其升压效果具有一定剂量依赖性,低剂量升压效果不足,较高剂量常常又会引起产妇高血压且易导致心动过速[8]。研究表明腰麻前10 min肌肉注射0.5 mg/kg麻黄碱预防SAIH,术中产妇血压波动范围较小[9],表明合适剂量的麻黄碱肌肉注射或者皮下局部浸润可使产妇术中血流動力学稳定。盐酸麻黄碱皮下局部浸润联合晶体共负荷预防SAIH的研究鲜见报道,故本研究旨在探讨这种方案在剖宫产术中预防SAIH是否为一种安全、有效的临床方案,现报道如下。
1 资料与方法
1.1 一般资料 选取牡丹江市妇女儿童医院2019年
10月-2020年1月收入院的60例择期在腰麻下行剖宫产产妇。纳入标准:(1)足月择期剖宫产;(2)胎儿发育正常,无畸形;(3)胎膜早破无严重感染;(4)产妇年龄22~35周岁;(5)ASA分级Ⅰ级或Ⅱ级;(6)单胎。排除标准:(1)妊娠合并高血压、糖尿病、心脏病;(2)患有HELLP综合征;(3)蛛网膜下腔麻醉失败;(4)椎管内麻醉穿刺禁忌证。根据电脑生成的随机数字,按随机数字表法将产妇分为C组和E组,每组30例。患者或家属同意并签署知情同意书,研究经该院伦理委员会同意批准。
1.2 方法 所有产妇无术前用药,常规禁水4 h、禁食6 h,入手术室后,平卧位,右侧髋部侧垫高15°,常规监测心电图(ECG)、血压(BP)、心率(HR)、血氧饱和度(SpO2)。18G留置针左前臂建立静脉通道,面罩吸氧4 mL/min。嘱患者平静休息5 min后,每间隔2 min连续3次测量,每次测量的MAP波动范围<10%,三次测量的MAP均值记为产妇基础MAP,三次测量对应的平均HR,记为产妇基础HR,此时间点记为T0。产妇取左侧膝胸位,L3~4行蛛网膜下腔麻醉。L3~4椎间隙逐层浸润麻醉,C组局麻药配制:1%盐酸利多卡因注射液(生产厂家:山东华鲁制药有限公司,批准文号:国药准字H37022839,规格:10 mL︰0.2 g)
4 mL;E组局麻药配制:1%利多卡因+15 mg盐酸麻黄碱注射液(生产厂家:东北制药集团沈阳第一制药有限公司,批准文号:国药准字H21022412,规格:1 mL︰30 mg)至4 mL,用18G硬膜外针(埃斯埃麻醉穿刺包,上海)硬膜外穿刺至硬膜外腔,成功后用腰麻针穿刺至蛛网膜下腔,见脑脊液外流后,缓慢注入重比重腰麻液[0.75%罗哌卡因(生产厂家:AstraZeneca AB,批准文号:注册证号H20140764,规格:10 mL︰75 mg)2 mL+50%葡萄糖(生产厂家:山东华鲁制药有限公司,批准文号:国药准字H20184027,规格:20 mL︰10 g)
0.2 mL+0.9%氯化钠注射液(生产厂家:辰欣药业股份有限公司,批准文号:国药准字H20013310,规格:100 mL︰0.9 g)0.8 mL,推注速度为0.1 mL/s,硬膜外腔置管备用,将麻醉平面调节控制在T6~8,右侧髋部垫高15°。C、E两组在腰麻液注入蛛网膜下腔即刻,15 mL/kg的乳酸钠林格注射液(生产厂家:山东威高药业股份有限公司,批准文号:国药准字H20044239,规格:500 mL)以最大速度静脉输注。腰麻液注入蛛网膜下腔后1、3、5、7、10、15、20、30 min的各个时间点分别记为T1、T2、T3、T4、T5、T6、T7、T8,测量记录腰麻液注入蛛网膜下腔后各时间点MAP、HR。胎儿娩出后未啼哭前夹闭脐带即刻采取脐带动脉血1 mL,立刻使用血气分析仪(RADIOMETER)进行血气分析。术中产妇若出现低血压(MAP<基础值20%)静脉应用盐酸麻黄碱5~10 mg,效果不明显可重复使用,直到血压恢复>基础血压80%;若出现心动过缓(HR<50次/min)静脉应用硫酸阿托品注射液(生产厂家:安徽长江药业有限公司,批准文号:国药准字H34021900,规格:1 mL︰0.5 mg)0.5 mg直到心率恢复>50次/min;若出现反应性高血压,MAP>基础值30%时,静脉应用乌拉地尔注射液(生产厂家:广州万正药业有限公司,批准文号:国药准字H20010806,规格:5 mL︰25 mg)5 mg,C、E两组晶体液速度降至40~60滴/min。
1.3 观察指标及判定标准 比较两组T1~T8各时间点MAP、HR水平。比较两组并发症发生情况,包括低血压、反应性高血压、恶心、呕吐。比较两组静脉应用盐酸麻黄碱剂量。比较两组新生儿的酸中毒及Apgar评分情况,包括新生儿脐动脉pH值、碱剩余、乳酸及新生儿1、5 min Apgar评分情况,Apgar评分满分10分,分数越高新生儿情况越好。
1.4 统计学处理 采用SPSS 22.0软件对所得数据进行统计分析,计量资料用(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 两组年龄、身高、体重、孕周、ASA分级比较,差异均无统计学意义(P>0.05),见表1。
2.2 两组各时间点MAP、HR水平比较 T4~T8,E组的MAP均明显高于C组,差异均有统计学意义(P<0.05);T0~T3,两组的MAP、HR比较,差异均无统计学意义(P>0.05);T4~T8,两组的HR比较,差异均无统计学意义(P>0.05)。见表2。
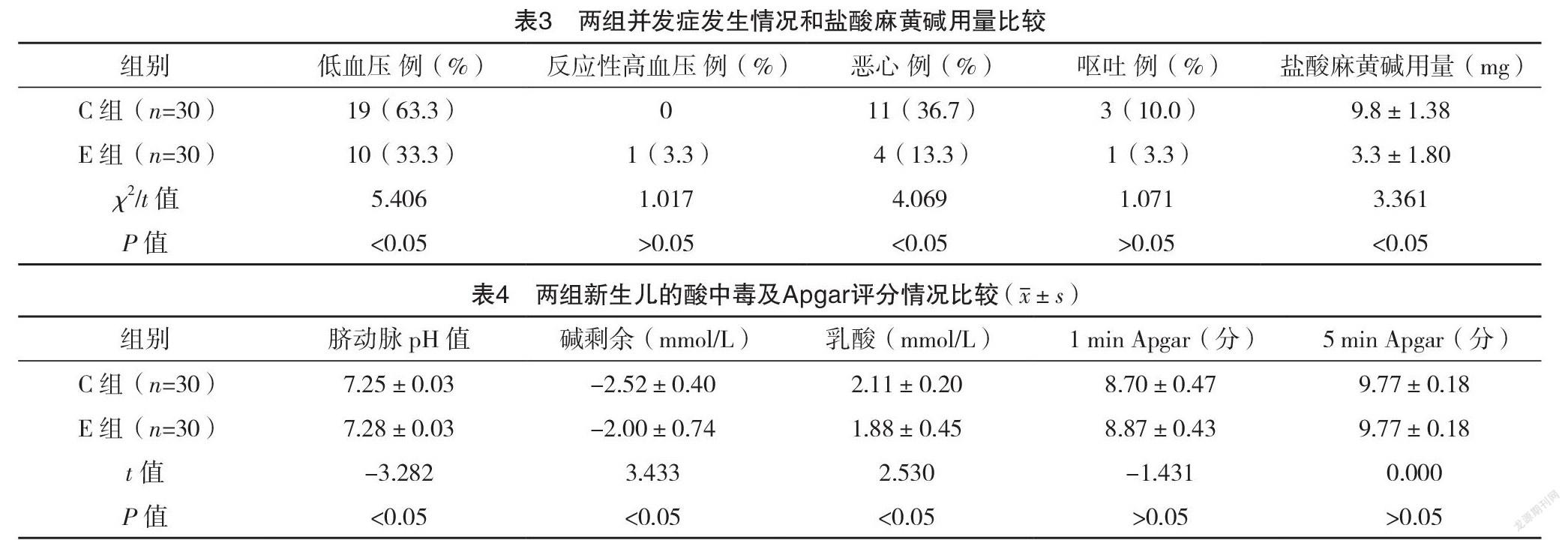
2.3 两组并发症发生情况和盐酸麻黄碱用量比
较 E组低血压发生率为33.3%,低于C组的63.3%,差异有统计学意义(P<0.05);E组恶心发生率为13.3%,低于C组的36.7%,差异有统计学意义(P<0.05);两组反应性高血压、呕吐发生率比较,差异均无统计学意义(P>0.05);C组静脉应用盐酸麻黄碱的总剂量明显高于E组,差异有统计学意义(P<0.05)。见表3。
2.4 两组新生儿的酸中毒及Apgar评分情况比较 E组的pH明显高于C组,碱剩余、乳酸均明显优于C组(P<0.05);新生儿的1、5 min Apgar评分比较,差异均无统计学意义(P>0.05)。见表4。
3 讨论
麻黄碱可以增加产妇心排血量(CO)和改善胎盘的血供[10]。臨床上常常在SAIH发生时静脉推注麻黄碱5~10 mg,较少预防性肌注或皮下应用麻黄碱。盐酸麻黄碱肌注/皮下单次剂量为15~30 mg,极量为60 mg,为预防反应性高血压的发生,本研究选择了肌注最小有效剂量15 mg。近年来,剖宫产术中防治SAIH发生的液体管理方案一直存在争议,主要表现在液体的选择、晶胶输注配比、液体的输注时机这三方面[6],目前最常用的液体管理方案为晶体预/共负荷、胶体预/共负荷。苏鸿莉等[11]的研究发现胶体液预负荷与晶体液共负荷预防剖宫产术中SAIH的效果无明显统计学差异,而胶体液易导致过敏反应、凝血功能障碍等不良并发症发生[12],因此临床上常选用晶体进行扩容。另外,Ni等[13]的研究发现晶体共负荷预防SAIH的效果优于晶体预负荷。因此本研究选择15 mL/kg乳酸林格共负荷预防产妇术中SAIH。
晶体共负荷可以减少SAIH的发生率,但单独晶体共负荷预防SAIH效果有限。Mercier[14]分析得出,在腰麻后最初的5~10 min输注足够的液体,并预防性应用血管收缩药物可以增加单独晶体共负荷预防SAIH的效果。与此结论一致,Buthelezi等[15]的研究中将苯肾上腺素500 μg加入1 000 mL乳酸林格液中共负荷输注,产妇SAIH的发生率降低了29%。与Mercier[14]的研究结果一致,本研究中,与单纯晶体共负荷输注相比,局麻时1%利多卡因与15 mg盐酸麻黄碱混合局部浸润,低血压的发生率降低了30%。其作用机制可能是盐酸麻黄碱在SAIH发生前逐渐发挥作用,从而减少了SAIH的发生。但33%的产妇出现SAIH,这不除外本试验中盐酸麻黄碱剂量较小的可能,提示对一般产妇来说可能存在更适合的剂量,需进一步探索。本研究中E组发生了1例反应性高血压,但是MAP升高的幅度<基础血压30%,且产妇无不适发生。
本研究结果显示,T4~T8,E组的MAP均明显高于C组,差异均有统计学意义(P<0.05);T0~T3,两组的MAP、HR比较,差异均无统计学意义(P>0.05);T4~T8,两组的HR比较,差异均无统计学意义(P>0.05)。从T4~T8时间点,与T0时相比,E组MAP的下降程度明显小于C组,表明E组血压波动较小,血流动力学较C组稳定。这说明晶体共负荷联合应用麻黄碱可以从降低低血压的发生率及低血压的严重程度,从而维持产妇腰麻后血流动力学的稳定。然而,盐酸麻黄碱皮下局部浸润给药相对于静脉给药而言,吸收缓慢,达到有效血药浓度需要一定的时间,这在一定程度上削弱了其对SAIH的预防作用。但在本研究中盐酸麻黄碱达到有效血药浓度之前,静脉快速输注的晶体液可以抵消一部分因腰麻导致血管扩张造成的血容量相对不足;另外,局部麻醉药所具有的血管扩张作用加速了盐酸麻黄碱的吸收,从而维持血压平稳。
产妇血流动力学的稳定,良好的胎盘灌注对于胎儿酸碱状态的影响至关重要。麻黄碱可通过胎盘影响胎儿pH值。Kee等[16]的研究发现盐酸麻黄碱可通过胎盘激动胎儿的β受体增加其新陈代谢,使氧气相对不足,致脐动脉血pH降低。Rolbin等[17]进一步研究表明腰麻前预防性肌肉注射盐酸麻黄碱45 mg对胎儿的pH值和Apgar评分无显著影响,当盐酸麻黄碱肌肉注射增至50 mg时才出现胎儿酸中毒。可见盐酸麻黄碱对胎儿pH的影响可能存在剂量相关性。本研究结果显示,E组的pH明显高于C组,差异有统计学意义(P<0.05),没有出现1例严重酸中毒(pH<2.0),并且无一例pH<2.5。这可能是E组麻黄碱维持血流动力学稳定的结果,也不除外盐酸麻黄碱使用剂量较小。另外,E组的碱剩余、乳酸均明显低于C组,差异均有统计学意义(P<0.05);进一步表明E组维持血压较平稳,对新生儿的不良影响较小。蛛网膜下腔阻滞引起的低血压和仰卧位低血压综合征、饱胃、手术牵拉刺激等均可引起产妇恶心呕吐[18-19]。本研究结果显示,E组恶心发生率低于C组,差异有统计学意义(P<0.05)。C组静脉应用盐酸麻黄碱的总剂量明显高于E组,差异有统计学意义(P<0.05),也进一步表明E组的血压维持优于C组。本研究选取的研究对象为健康产妇,有研究表明先兆子痫产妇的SAIH的发生率和严重程度均低于健康女性[20],而该方案在循环功能障碍、妊娠期高血压产妇或者先兆子痫产妇中的应用安全性有待进一步研究。
综上所述,盐酸麻黄碱局部浸润联合晶体共负荷预防SAIH,低血压发生率明显降低,术中血压波动范围小,且无明显反应性高血压等不良反应,对胎儿的酸碱状态影响较小,可安全应用于健康产妇。
参考文献
[1] George R B,Mckeen D M,Dominguez J E,et al.A randomized trial of phenylephrine infusion versus bolus dosing for nausea and vomiting during Cesarean delivery in obese women[J].Can J Anaesth,2018,65(3):254-262.
[2] Lappen J R,Chien E K,Mercer B M.Contraction-Associated Maternal Heart Rate Decelerations: A Pragmatic Marker of Intrapartum Volume Status[J].Obstet Gynecol,2018,132(4):1011-1017.
[3]杜唯佳,徐振東,刘志强.剖宫产腰麻后低血压预测方法的研究进展[J].临床麻醉学杂志,2019,35(2):192-194.
[4] Tan H S,Gan Y T,Tan E C,et al.Association of renin-angiotensin-aldosterone system genetic polymorphisms with maternal hypotension during spinal anaesthesia for caesarean delivery - a retrospective cohort study[J].International Journal of Obstetric Anesthesia,2020,44:3-12.
[5]王云秀,左小清.剖宫产椎管内麻醉产妇发生低血压的危险因素分析[J].临床医学研究与实践,2019,4(11):85-86,99.
[6]陈伟,陈永权.剖宫产腰麻后低血压防治措施的研究进展[J/OL].中华临床医师杂志(电子版),2019,13(4):312-315.
[7]丁振东,谭慧玲,郑洪,等.麻醉前预泵注间羟胺对剖宫产产妇腰麻后低血压的防治作用[J].临床麻醉学杂志,2020,36(6):599-601.
[8] Nag D S.Vasopressors in obstetric anesthesia: A current perspective[J].World Journal of Clinical Cases,2015,3(1):58-64.
[9] Bhar D,Bharati S,Halder P S,et al.Efficacy of prophylactic intramuscular ephedrine in prevention of hypotension during caesarean section under spinal anaesthesia: a comparative study[J].J Indian Med Assoc,2011,109(5):300-303,307.
[10] Guo R,Xue Q,Qian Y,et al.The Effects of Ephedrine and Phenylephrine on Placental Vascular Resistance During Cesarean Section Under Epidual Anesthesia[J].Cell Biochem Biophy,2015,73(3):687-693.
[11]苏鸿莉,晋雅凌.胶体液预负荷和晶体液共负荷在预防腰麻剖宫产术中低血压效应的临床疗效对比[J].安徽医药,2015,19(11):2210-2212.
[12] Heesen M,Stewart A,Fernando R.Vasopressors for the treatment of maternal hypotension following spinal anaesthesia for elective caesarean section: past, present and future[J].Anaesthesia,2015,70(3):252-257.
[13] Ni H F,Liu H Y,Zhang J,et al.Crystalloid Coload Reduced the Incidence of Hypotension in Spinal Anesthesia for Cesarean Delivery, When Compared to Crystalloid Preload: A Meta-Analysis[J].BioMed Research International,2017,2017:1-10.
[14] Mercier F J.Cesarean delivery fluid management[J].Curr Opin Anaesthesiol,2012,25(3):286-291.
[15] Buthelezi A S,Bishop D G,Rodseth R N,et al.Prophylactic phenylephrine and fluid co-administration to reduce spinal hypotension during elective caesarean section in a resource-limited setting: a prospective alternating intervention study[J].Anaesthesia,2019,75(4):487-492.
[16] Kee W N,Khaw K S,Tan P E,et al.Placental transfer and fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery[J].Anesthesiology,2009,111(3):506-512.
[17] Rolbin S H,Cole A,Hew E M,et al.Prophylactic intramuscular ephedrine before epidural anaesthesia for caesarean section: Efficacy and actions on the foetus and newborn[J].Can Anaesth Soc J,1982,29(2):148-153.
[18]趙军博,姜丽华,杨波.多拉司琼与托烷司琼用于预防子宫收缩剂引发的剖宫产产妇恶心呕吐的效果比较[J].数理医药学杂志,2020,33(7):1013-1015.
[19] Ashagrie H E,Chekol T D,Melese D Y,et al.The incidence and factors associated with intraoperative nausea and vomiting during cesarean section under spinal anesthesia, July 2019. An institution based cross sectional study[J].International Journal of Surgery Open,2020,26:49-54.
[20] Sivevski A,Ivanov E,Karadjova D,et al.Spinal-Induced Hypotension in Preeclamptic and Healthy Parturients Undergoing Cesarean Section[J].Open Access Maced J Med Sci,2019,7(6):996-1000.
(收稿日期:2020-11-11) (本文编辑:姬思雨)