Implantation of an S-ICD in a Patient with a DDD Pacemaker and Congenitally Corrected Transposition of the Great Arteries
Yu Zhang ,Wen-Long Dai ,Can-Can Lin ,Qiao-Yuan Li and Cheng-Jun Guo
1 Department of Cardiology,Beijing Anzhen Hospital,Capital Medical University,Beijing,China
Abstract Subcutaneous implanTablecardioverter-def ibrillator (S-ICD) therapy has become a viablealternative to conventional transvenous ICD implantation.Patients with congenitally corrected transposition of the great arteries (ccTGA) have a high risk of sudden cardiac death due to malignant arrhythmia.The interaction between the S-ICD system and the transvenous pacemaker system is not fully understood.We report a case of S-ICD implantation in a patient with ccTGA and a DDD pacemaker.The patient was a 30-year-old man with a previously placed pacemaker with diagnoses of congenital heart disease,ccTGA (SLL),left atrioventricular valve insuff iciency,and third-degree atrioventricular block.He presented with an out-of-hospital cardiac arrest,and an S-ICD was implanted to prevent sudden cardiac death.Def ibrillation checks were performed successfully.We tested the compatibility of the DDD pacemaker with the S-ICD and found that there was no interference between them.In conclusion,an S-ICD system is a reasonableand safe option in patients with ccTGA.
Keywords:Subcutaneous implanTablecardioverter-def ibrillator; congenitally corrected transposition of the great arteries; pacemaker
Using currently availablesubcutaneous implanTablecardioverter def ibrillators (S-ICD) in patients with cardiac malposition remains diff icult.The feasibility and eff icacy remain unknown.We report a case of S-ICD implantation in a patient with congenitally corrected transposition of the great arteries (ccTGA) and a DDD pacemaker.ccTGA is an uncommon cardiac defect,accounting for less than 0.5% of congenital heart disease (CHD) [1,2].Most patients may also have one or more anomalies,such as ventricular septal defect,pulmonary stenosis,and abnormalities of the systemic atrioventricular(tricuspid) valve [3].
The patient was a 30-year-old man with diagnoses of CHD,ccTGA (SLL),left atrioventricular valve insuff iciency,and third-degree atrioventricular block.He had left atrioventricular valve replacement and left clavicular fracture f ixation at 16 years of age with warfarin as medication.Because of third-degree atrioventricular block,he underwent placement of a transvenous dual-chamber pacemaker (Biotronik Effecta D) in January 2018.He presented with an out-of-hospital cardiac arrest,and ventricular f ibrillation was later documented in October 2018.After external electric def ibrillation and cardiac compression by the emergency medical team,he was successfully resuscitated.At a local hospital,24-hour dynamic electrocardiogram(ECG) demonstrated ventricular tachycardia,frequent premature ventricular contractions,and loss of atrial capture.Pacemaker interrogation verif ied atrial electrode dislocation,and then the pacemaker was set to VVI mode.
On the basis of the patient’ s history,an ICD system was judged to be appropriate for secondary prevention of sudden cardiac arrest.There were detailed discussions between the family and the care team regarding options for ICD placement,and f nially a decision was made to implant an S-ICD.Detailed screening for the S-ICD was performed before device placement.Baseline 12-lead ECG demonstrated paced rhythm (VVI,basic rate 70 bpm) and QRS duration of 236 ms.Initial ECG vector screening revealed that the patient would be an optimal candidate on the basis of the screening result with the generator in the left axilla and the electrode placed on the right of the sternum.He also passed screening at higher heart rates,which was paced at 110 bpm.
An Emblem S-ICD (Boston Scientif ic,Marlborough,MA,USA) was placed with the generator in the left axilla,the inferior portion of the electrode to the right of the xyphoid,and the tip of the electrode to the immediate right of the sternum.Sensing through the device was noted to be best in the primary vector.The S-ICD was implanted by a three-incision technique with the patient under general anesthesia.Def ibrillation testing was performed at the time of implantation.Ventricular f ibrillation was induced by a 50-Hz current and was adequately sensed,but was not terminated by the f irst 65-J shock.Sixteen seconds later,the device successfully converted the arrhythmia back to paced rhythm with an 80-J shock; the charge time was less than 10 s and the shock impedance was 70 Ω ( Figure1).A postoperative chest X-ray showed proper position of the lead and S-ICD ( Figure2).After successful implantation,the interaction between the S-ICD and the pacemaker was investigated.When the ventricular lead was programmed to bipolar 3.0 V,unipolar 3.0 V,unipolar 7.5 V,and bipolar 7.5 V,at 0.4 ms,the morphology of the QRS complex recorded by the S-ICD remained quite sTable( Figure3).There was a slight change of the morphology of the QRS complex in the secondary vector,and the S-ICD sensed the QRS complex as noise in the primary vector when paced at unipolar 7.5 V.Neither bipolar nor unipolar pacing led to oversensing in any of the vectors in the supine and standing positions.Otherwise,the pacemaker functioned normally after two high-output shocks from the S-ICD.In the postoperative interrogation,the ventricular electrode of the pacemaker was programmed to bipolar pacing.The S-ICD was programmed with a shock zone of 200 bpm and a conditional shock zone of 170 bpm with postshock pacing off.At the 3-month followup visit in April 2019,the patient did not report syncope or other discomfort,and had not received any S-ICD shocks.
Discussion
Because of a history of recurrent ventricular arrhythmias,the patient met the criteria for ICD implantation.However,there might have been technical diff iculties and a high risk of postoperative complications for a traditional transvenous dual-chamber ICD with his complicated status and anatomical challenges.Besides,atrial electrode dislocation was another tricky problem.One solution could be transvenous lead extraction and implantation of a new transvenous ICD,which may cause major damage to the heart.Implantation of a new ICD without lead extraction could be another solution,thus leaving four leads in the vein,which could potentially cause venous occlusion and make it diff icult to replace or upgrade the device in the future.Since an S-ICD avoids the need for transvenous leads,use of this technique may provide an excellent alternative to epicardial or transvenous systems in young patients who require ICD placement.
The S-ICD is compatible with a pacemaker(Boston Scientif ic,Shanghai,China,pacemakers),which will avoid unipolar pacing in safe mode according to the technical manual for the S-ICD.Moreover,patients requiring permanent pacing and those with a previously implanted functional unipolar pacing system were excluded from S-ICDrelated clinical studies [4,5].However,several case reports examining the interaction of pacemaker and S-ICD systems have been published.Steinberg et al.[6] demonstrated the feasibility and safety of the addition of an S-ICD to a bipolar epicardial pacemaker system.A case report by Kossidas et al.[7]found that a unipolar epicardial pacing system can be used in combination with an S-ICD,with certain assessment and programming steps.In our case,we found the S-ICD sensed the QRS complex as noise in the primary vector when paced at unipolar 7.5 V at 0.4 ms.One way to overcome this situation is to avoid unipolar pacing at high amplitude.In our postoperative interrogation,the pacemaker was programmed to bipolar pacing.Also,it is recommended to program the pacemaker to bipolar pacing to prevent oversensing.
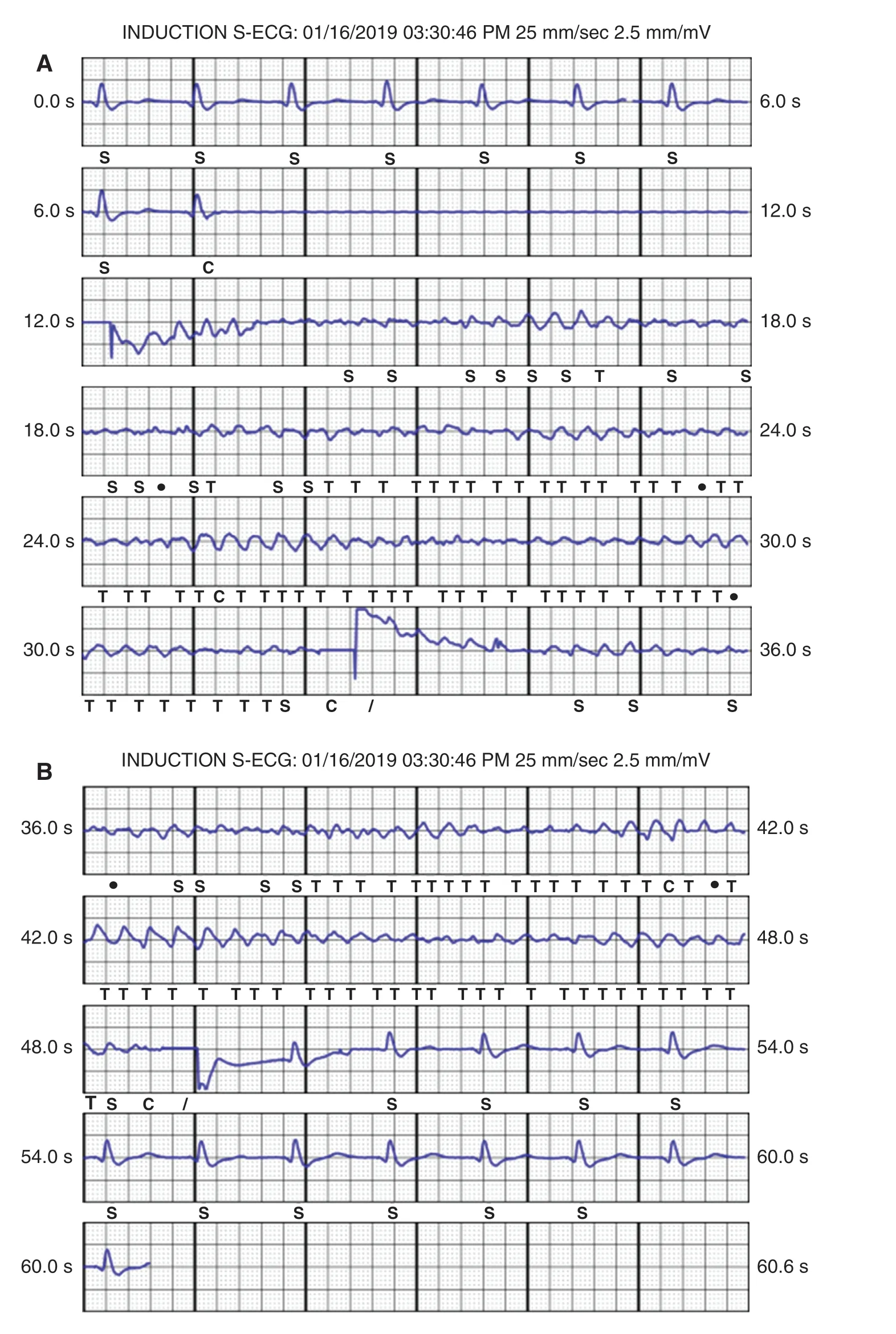
Figure1:Induction of Ventricular Fibrillation by a 50-Hz Current and Successful Def ibrillation after an 80-J Shock with an Impedance of 70 Ω.
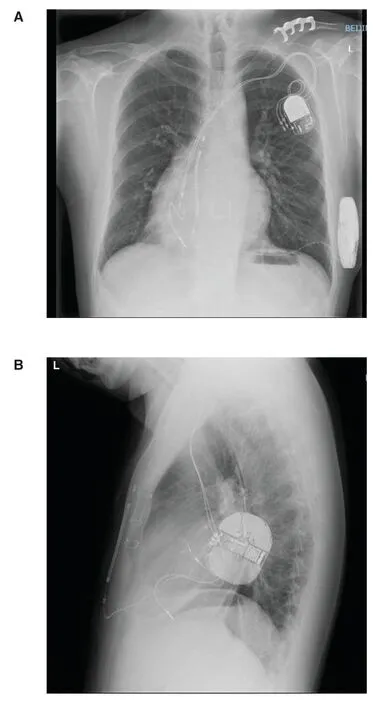
Figure2:Chest Radiographs of the Posteroanterior
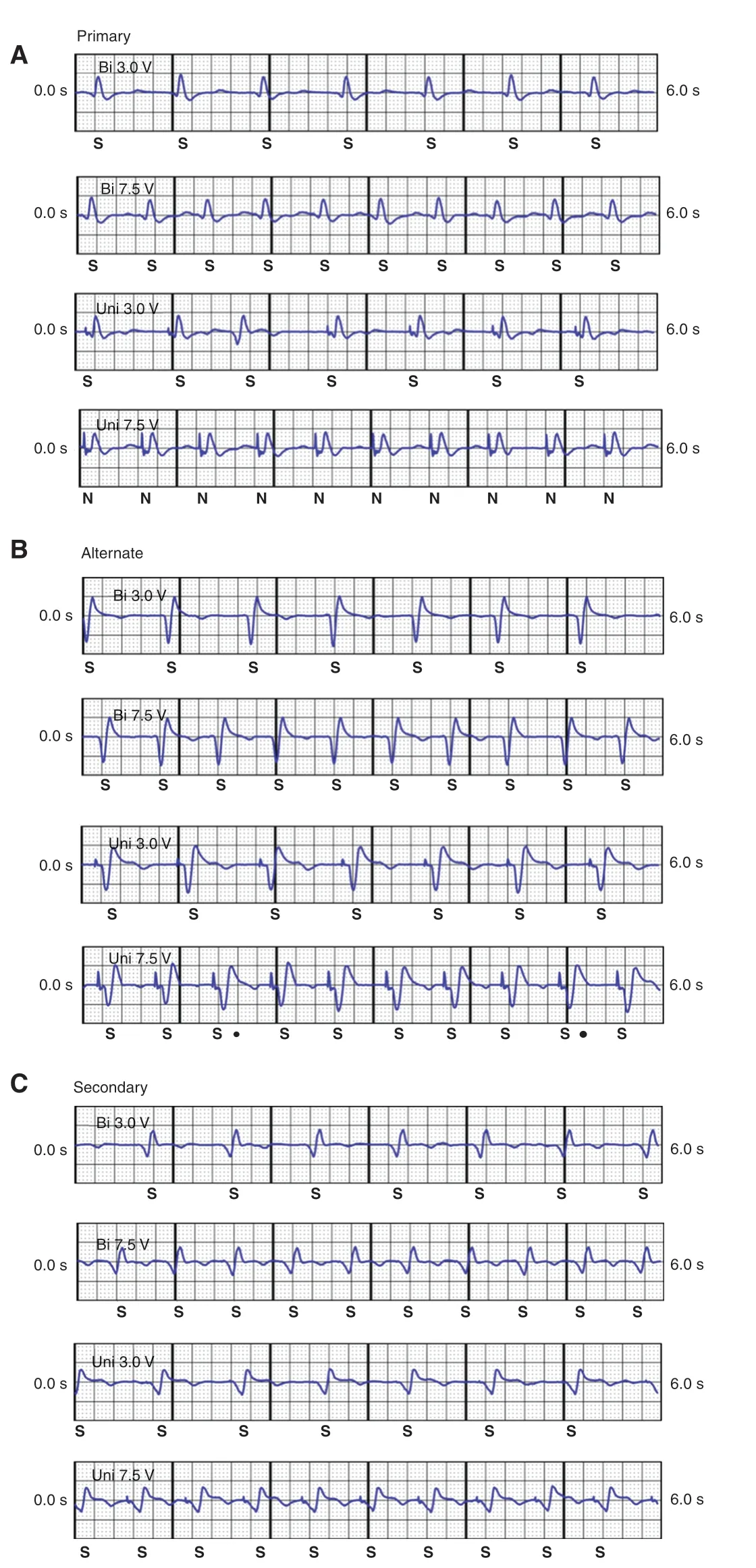
Figure3:Real-Time Electrogram Recordings from the Subcutaneous ImplanTableCardioverter-Def ibrillator System During Different Pacing Conf igurations at all Three Vectors.
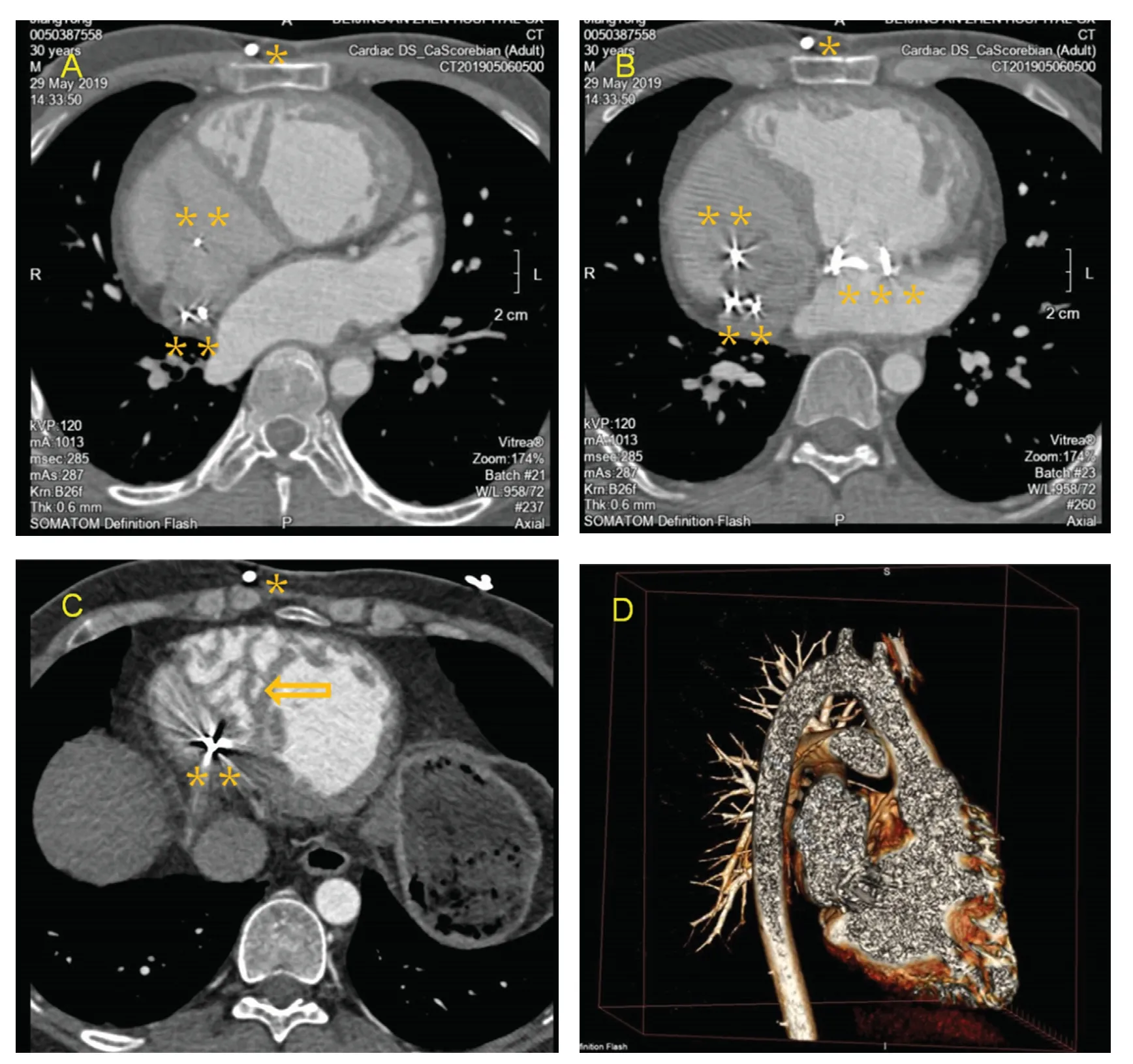
Figure4:Postoperative Computed Tomography Scans (A- C) and Reconstruction (D) Showing the Pacemaker Leads,the Subcutaneous ImplanTableCardioverter-Def ibrillator (S-ICD) Lead,and the Structure of the Heart.
In our patient,def ibrillation testing revealed excellent sensing during ventricular f ibrillation,while ventricular f ibrillation was not terminated by the f irst 65-J shock,although the second def ibrillation with an 80-J shock succeeded.In a meta-analysis of the cohort of CHD patients in the IDE study and the EFFORTLESS registry,both patients who failed def ibrillation testing at 65 J had d-transposition of the great arteries (d-TGA).The total number of patients with d-TGA was six.However,the sample size of the congenital cohort was small,which complicates any assessment of the eff icacy of the S-ICD specif ically in d-TGA [8].After atrial switch surgery,the anatomical right ventricle becomes the systemic ventricle,which is similar to the case for our patient.A right parasternal electrode position may not suff iciently include the dilated and shifting to right systemic (right) ventricle in the shock path ( Figure4 ),which might explain the unsuccessful shock at 65 J.Besides,noncompaction of right ventricular myocardium could also be part of the reason ( Figure4C).Further study of def ibrillation testing in CHD patients,especially those with ccTGA or d-TGA,will be necessary in the future.
In this case we reported that an S-ICD system was used in conjunction with a previously placed transvenous DDD pacemaker that provides chronic pacing.Because the S-ICD system avoids the need for transvenous leads,use of this system in young patients with ccTGA and other CHD who require ICD implantation is quite appealing.
Conf lict of Interest
The authors conf irm that there is no conf lict of interest.
 Cardiovascular Innovations and Applications2021年1期
Cardiovascular Innovations and Applications2021年1期
- Cardiovascular Innovations and Applications的其它文章
- A Meta-analysis of Major Complications between Traditional Pacemakers and Leadless Pacemakers
- Risk of Target Organ Damage in Patients with Masked Hypertension versus Sustained Hypertension:A Meta-analysis
- ECMO/CRRT Combined Support in the Treatment of Critically Ill SARS-CoV-2 Pneumonia Patients
- Predictive Value of Blood Pressure,Heart Rate,and Blood Pressure/Heart Rate Ratio in a Chinese Subpopulation with Vasovagal Syncope
- The Challenges of Treating Acute Myocardial Infarction due to Variant Angina:Lesson from an Interesting Case
- Relation between Cardiac Injury and Elevated Levels of Inf lammatory Biomarkers in Patients with Severe COVID-19
