Prediabetes and cardiovascular complications study: Highlights on gestational diabetes, self-management and primary health care
Ezekiel Uba Nwose, Phillip Taderera Bwititi, Otovwe Agofure, Echinei Jacob Oshionwu, Ekenechukwu Esther Young, Eferhire Aganbi, Solomon Ekwuweokwuenu Egwenu, Helen Egoyibo Chime, Fortunatus Darius Gbeinbo, Alex Odufu, John Nwakaego Okuzor, Azuka Okuleye, Kennedy Aninze, Innocent Chuks Onyia, Euzebus Chinonye Ezugwu, Eunice Obiajuru Igumbor, Ifeoma Isabel Ulasi
Ezekiel Uba Nwose, Otovwe Agofure, Solomon Ekwuweokwuenu Egwenu, Helen Egoyibo Chime, Fortunatus Darius Gbeinbo, Eunice Obiajuru Igumbor, Department of Public and Community Health, Novena University, Kwale 322107, Nigeria
Ezekiel Uba Nwose, Phillip Taderera Bwititi, School of Dentistry and Medical Sciences, Charles Sturt University, Wagga campus, New South Wales 2650, Australia
Ezekiel Uba Nwose, Echinei Jacob Oshionwu, Alex Odufu, John Nwakaego Okuzor, Azuka Okuleye, Kennedy Aninze, Innocent Chuks Onyia, Global Medical Research and Development Organization (GMRDO) group, Abbi Delta State 322107, Nigeria
Echinei Jacob Oshionwu, California Department of State Hospital, Stockton, CA 95215, United States
Ekenechukwu Esther Young, Euzebus Chinonye Ezugwu, Ifeoma Isabel Ulasi, Department of Medicine, College of Medicine, University of Nigeria, Ituku-Ozalla campus, Enugu 402109, Nigeria
Eferhire Aganbi, Biochemistry Department, Delta State University, Abraka 330105, Nigeria
John Nwakaego Okuzor, Department of Clinical Laboratory Services, Texas Health (HMH HEB), Bedford, TX 76022, United States
Kennedy Aninze, Clinic Department, Donak Hospital, Kwale 2539083, Nigeria
Innocent Chuks Onyia, Clinic Department, U-Turn Hospital, U-Turn Abule Egba 100276, Nigeria
Abstract International collaboration on the prediabetes and cardiovascular complications study started in 2013.In 2017, a reflection was reported.Incompleteness of documentation and screening of antenatal cases for gestational diabetes mellitus (GDM) was concerning.Hence, further observations have been made that warrant an update.The objective of this review is to highlight gaps between clinical knowledge and practice in GDM, diabetes self-management and primary health care (PHC) for rural dwellers.We followed a descriptive field notes method.Antenatal records of patients screened for GDM with incomplete documentation were examined to determine incompleteness of data in those that also met the criteria for GDM risk assessment.Experiences on development of a diabetes register and education and notes on behavioural change wheel were also reviewed.Other data included cross-sectional evaluation of activities of daily living at two private hospitals.Up to 29% had high GDM risk factors, which fulfilled selection criteria for laboratory screening.Demographic data was complete in all women; however, incomplete documentation was observed with as much as 98% of basic data.High levels of physical activity were found in the population, and health lectures proved effective in food choices.The workforce need for diabetes care seems underestimated, but this may be better understood with reactivation of PHC services.The observations highlight behavioural change wheel issues on GDM and PHC services that need concerted focus.Two proposals are to advance the use of a ‘risk assessment and screening sheet’ for GDM screening and enlightenment of stakeholders on the central hub role of PHC in diabetes management.
Key Words: Behavioural change wheel; Community health; Diabetes education; Knowledge vs practice gap; Lifestyle; Patient follow-up; Screening services; Telehealth
INTRODUCTION
Diabetes mellitus is a global challenge and public health concern that has continued to attract multifaceted research[1-3].These interests include laboratory examinations for definitive diagnosis of gestational diabetes mellitus (GDM)[4-6], lifestyle treatment options[7-9] and use of technologies for patient follow-up and self-management[10-12].
In 2013, a proposal for an international collaboration on prediabetes and cardiovascular complications study was launched[13].In 2017, an update with future directions was reported[14].In the last 3 years, the program has been expounded, with niches developing from parts of the research.The Global Medical Research and Development Organization that oversees the activities at Catholic Hospital Abbi conceptualized the integration of a monthly diabetes clinic and GDM screening and registry for antenatal clinic patients[15-17].A user-friendly GDM risk assessment and screening form was proposed in January 2020 in collaboration with the University of Nigeria Teaching Hospital.
An opportunity arose after the acquisition of the BRIDGES2 grant [Eli Lily and International Diabetes Federation (IDF)] for a targeted diabetes self-management education trial.This created impetus to develop the lifestyle component of the research.In addition to reports[18-20], two field notes detailing dietary options and food choices as well as physical activities of daily living (ADL) were presented.
To further add to the diabetes registry and BRIDGES2 project, the Global Medical Research and Development Organization reviewed primary health care (PHC) services.This included a discussion about telehealth capacities to enhance diabetes services[21,22].Telehealth is becoming an invaluable resource.The lessons from the coronavirus disease 2019 pandemic have proven this.Hence, field note observations relevant to PHC and telehealth constitute part of this update, including lessons from the World Diabetes Day (WDD) 2020.
Objective and approach of review
The objective of this paper is to give a periodic review of trends[23-25].This review is based on our current prediabetes and cardiovascular complications study research with a focus on the gap between knowledge and practice in laboratory testing for GDM diagnosis, including the use of risk assessment factors for selective screening.Other focus areas are emerging treatments (specifically nutrition) and technologies (medical record documentation and telehealth).
DESCRIPTIVE FIELD NOTES REVIEW
This review was designed to follow a descriptive field notes study method.The notes were based on the international collaboration on a prediabetes and cardiovascular complications study program.The study was carried out in Delta State, Nigeria and at health care centres/hospitals.For this update, the ‘project evaluation’ looked at notes and data from the ongoing study, and the goals for each section are given as subheadings.
GDM screening
GDM constitutes a subsequent health risk to the mother and child.Several risk factors for GDM are known; hence, screening is encouraged.However, the adoption of robust screening protocols in various health care facilities is lacking, and reports have indicated a similar situation in our research performance sites[15,29].One notable observation was that selection criteria for lab tests in GDM screening were being followed[16] but arbitrarily and with rampant incompleteness of procedure.Therefore, while a screening flow sheet has been articulated[15], it was appropriate to develop another sheet with selective screening criteria (Table 1).This proposed GDM risk assessment and screening sheet was informed by two points: (1) Risk factors are generally non-invasive and can be obtained during antenatal registration and history taking[30-32]; and (2) Risk scoring systems exist.One includes gestational age[31], while the other is without gestational age[32].
Standard selection for screening:A user-friendly algorithm or chart is yet to be developed.Pending the adoption of the risk scoring chart, this evaluation would assess antenatal patients with three risk factors for laboratory investigation of GDM.Two retrospective cohort reviews have tabulated the GDM risk assessment and screening sheet (Table 1).Furthermore, the mother’s blood type is a potential genetic factor for the likelihood of GDM developing overt diabetes mellitus (DM) postpartum[33].Blood type assessments are determined for antenatal patients but may not be included in GDM screening sheets.Nevertheless, it is important to identify this as part of GDM management.
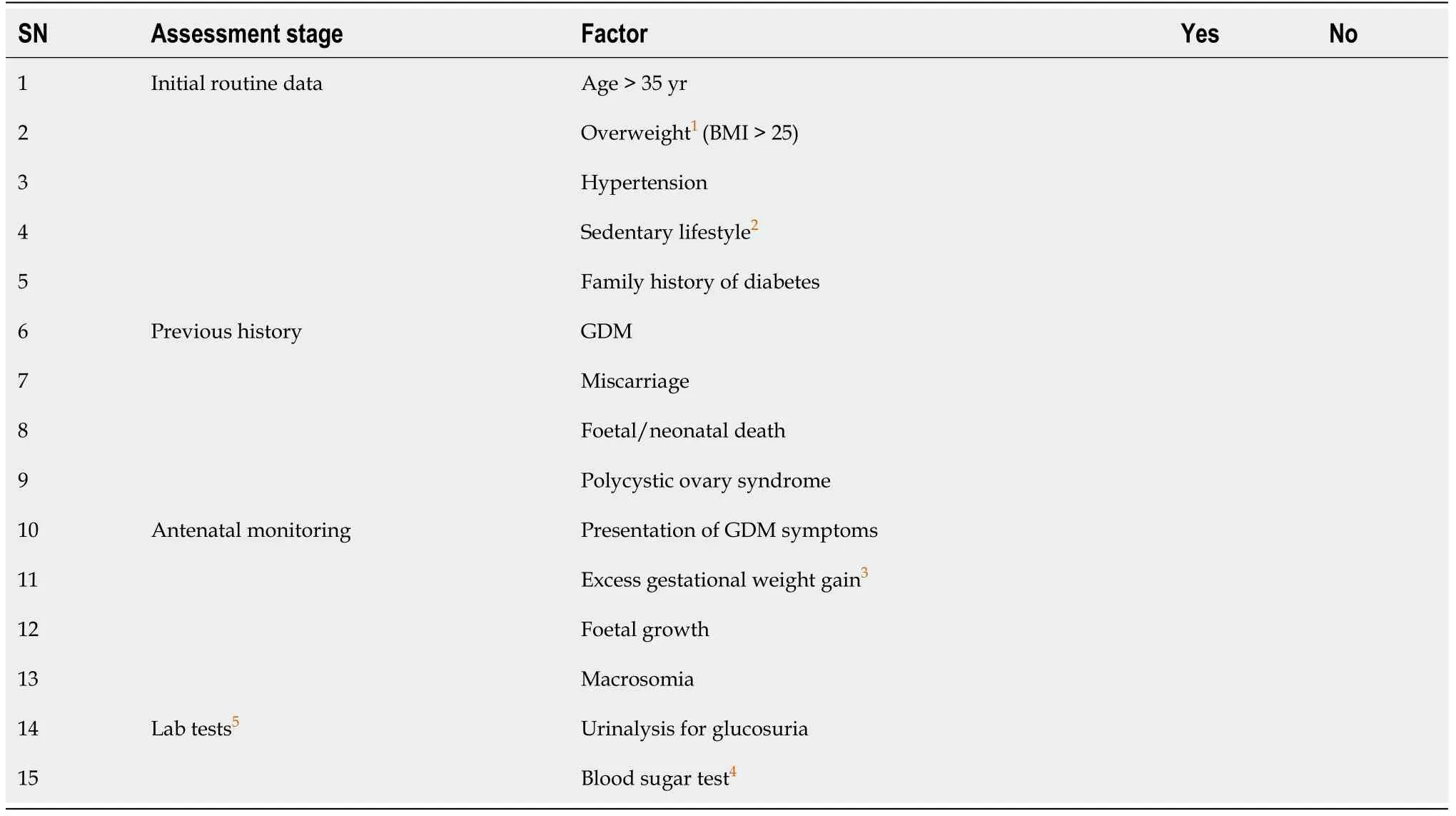
Table 1 Proposed gestational diabetes risk assessment and screening sheet
GDM screening register:In another field note, evaluation was specifically aimed to (1) Progress the development of screening registers, (2) Determine the level of attention given to or the potential of monitoring the rate of increase in body mass index (BMI) among the patients; and (3) Update the prevalence of GDM among pregnant women.
Diabetes self-management
Four items are imperative components of behavioural change included in diabetes education programs[34].They are dietary options, physical ADL, adherence to medical check-ups and adherence to prescription medicine.For this update, two field notes on dietary options and physical ADL are presented.
Physical ADL:Physical inactivity predisposes a person to DM.Thus, engaging in physical activities is preventive and therapeutic.The study evaluated ADL of local residents with diabetes who attended two non-government health facilities in rural communities of Delta State, Nigeria.This study was an addendum to a previous report[20].A cross-sectional descriptive design was used and comprised 48 participants from Catholic Hospital Abbi and Novena Health Centre Amai.A semi-structured questionnaire with integrated anthropometric and blood pressure measurements (weight, height, blood pressure, and BMI) was used.ADL of participants was delineated into bluevswhite collar jobs, depicting physically-active and -inactive occupations respectively.The data were analysed using the Microsoft Excel Analysis ToolPak.A demographic description of the respondents is presented in Table 2.Among the women, 11/21 (52.4%) were widows, and the average age of all respondents was 57 years.

Table 2 Descriptive statistics of respondents
Dietary options and food choices:In another study niche, the consumption of indigenous carbohydrate foods was evaluated.This niche was originally studied to determine the agribusiness and health economics nexus[35], but the basis of this field note was the controversy around cassava[36,37] that was buoyed by indigenously sourced cassava meal (eba/garri) being omitted from a hospital-based menu[19].The study involved baseline and post-intervention surveys of community members including hospital visitors, and the intervention was public health lectures on medical nutrition therapy value of cassava.Information collected included consumption habits regarding farmed choices (cassava and yam) and an imported option (wheat).
Other evaluations
PHC needs - lessons from WDD 2020: With the invaluable support from the Public Health Department of Novena University, the WDD event was organized at 11 health facilities, including four research performance sites, a general hospital, two PHC centres in the Delta state, one centre in the southern Nigeria, and three centres in northern Nigeria.There were 23 volunteers comprised of academic staff and postgraduate students of the Public Health Department of the Novena University who facilitated the event.An additional 79 health care personnel were recruited who delivered public health lectures and diabetes screening.A total of 286 community members benefited from the event[38].Observations were made from this event.
Telehealth potential in rural communities of Nigeria:Development of diabetes registers was started at the research performance sites,i.e.health facilities.However, evaluation of the usefulness for patient recall and telehealth have yet to be reviewed.Hence, in the hospital cohort study of 123 cases, the evaluation approach for telehealth involved assessing previous antenatal patients by telephone.
PERSPECTIVES ON GDM, SELF-MANAGEMENT AND PHC IN PREDIABETES AND CARDIOVASCULAR COMPLICATIONS
GDM screening
In a hospital cohort involving 90 cases, there was no urinalysis on the antenatal patients despite various prevalent risk factors.A history of GDM was the least common risk factor, and age over 35 years was the most common risk factor (Figure 1).Considering the prevalence of risk factors at initial registration, the lack of urinalysis is inexplicable.In another hospital cohort of 123 cases, 29% of those assessed had three or more risk factors that warranted screening (unpublished data).These reports provide evidence that screening education should be provided to antenatal providers.
Level of completeness of data collected during GDM screening:We collected data from 391 antenatal cases that were seen from September 2018 to December 2018.The women’s ages ranged from 15 to 46 years, and average gestational age was 23 wk, with the earliest clinic visit occurring at the fourth week.Further, several of the women were in their first pregnancy, and cohort average was less than gravida 3 (Table 3).
Among the 391 cases, the names, ages, medical record numbers and dates of hospital visits were complete,i.e., 100% documentation.Information on the mother’s and/or family history of type 2 diabetes and GDM were not indicated,i.e., 0% documentation on hereditary risk factor.There were also no records of lipid profiles.Other relevant data that were collected are presented in Table 4.Blood sugar tests were undocumented for 98.7% of patients, and BMI was not reported for 76.7% of patients.Overall, our results show that the average level of completeness of data collection during GDM screening was 79% (Figure 2).The figure shows the percentages of completeness that were not captured in Table 4.
Level of attention given to BMI:The 301/391 cases lacking BMI measurement had missing data on height (Table 4), but only 14 Lacked weight measurements.A critical evaluation showed that 5% of the cases without BMI values were due to lack of height and weight measurements, and 95% were solely due to lack of height data (Figure 3).Further review of the potential monitoring rate of increase in BMI among the patients showed that 13% (12/90) were in the first trimester and 48% (43/90) in the second trimester.There was a noticeably higher level of BMI in the third trimester relative to the earlier trimesters, but the difference was not statistically significant.
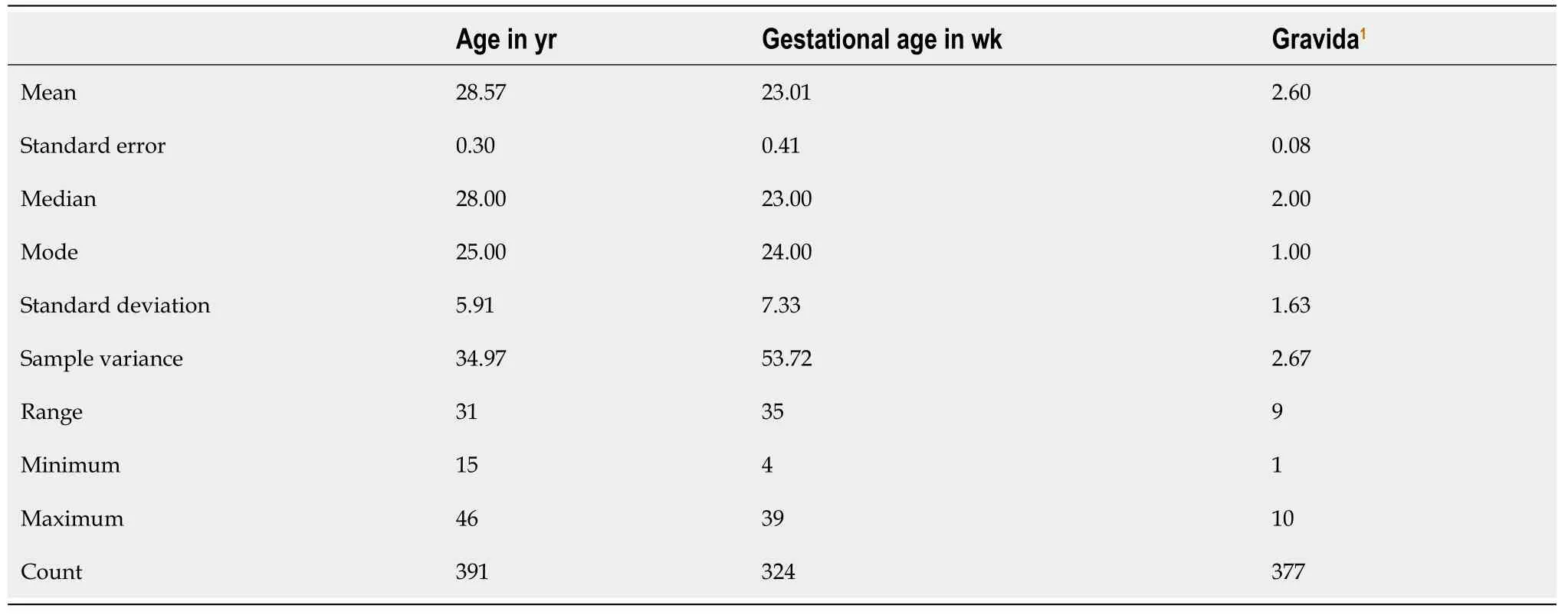
Table 3 Descriptive statistics of patients entered in a gestational diabetes screening register
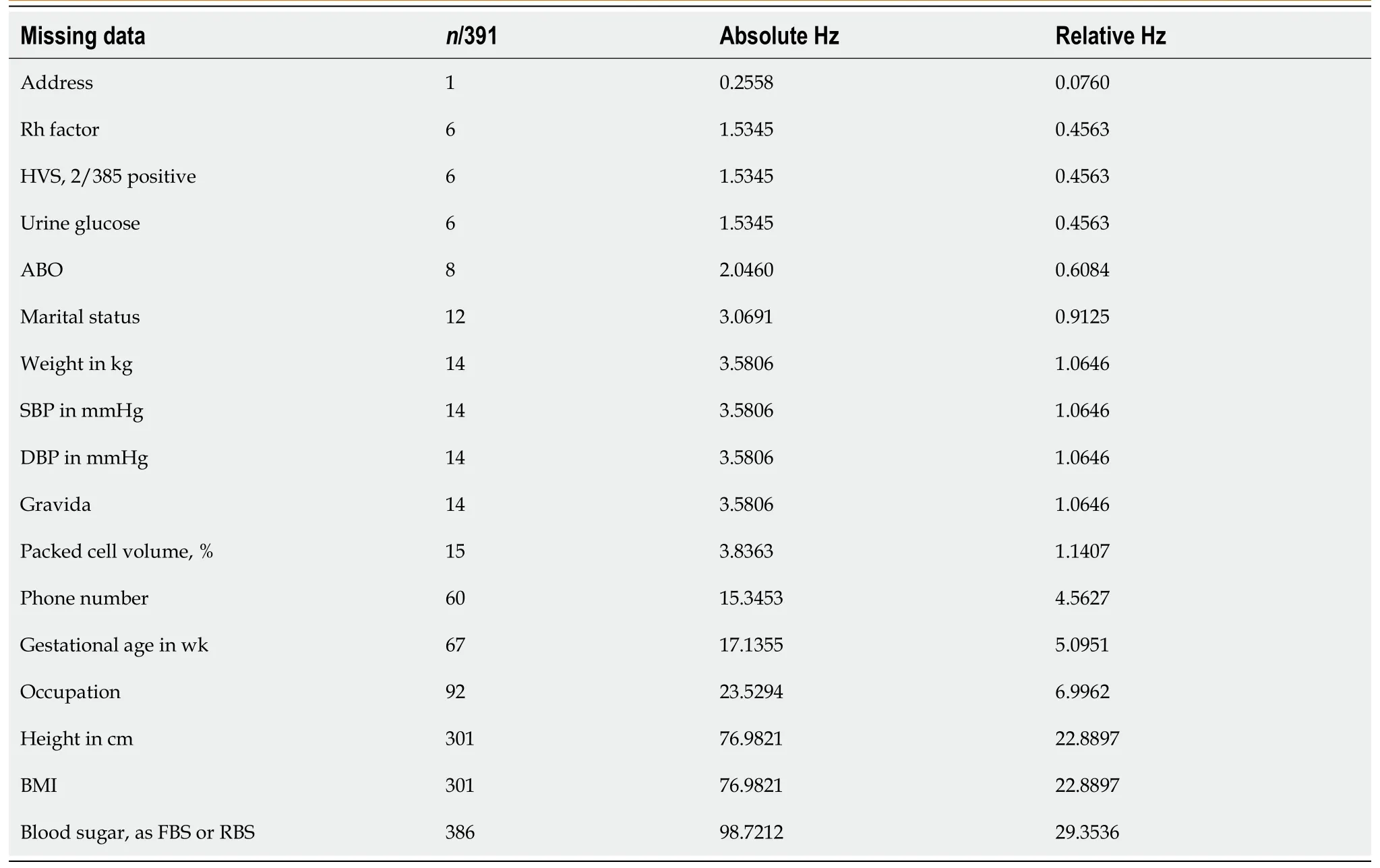
Table 4 Level of incompleteness of data
ADL in the community
This analysis was based on the occupation of the participants.The indicated occupations were categorized into blue collar (manual labour,e.g., agriculture, construction,etc.) and white collar (office or non-hard manual work professional) depending on assumptions of physical demands of the jobs.Forty-eight respondents were analysed, including four who did not indicate their occupations and were assumed to be blue collar.Evaluation showed that 73% were involved in physically demanding ADL (Figure 4).

Figure 1 Prevalence of gestational diabetes risk factors in a hospital cohort from Delta State, Nigeria.
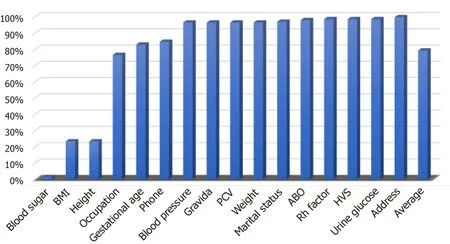
Figure 2 Translated percentage completeness of data collection.
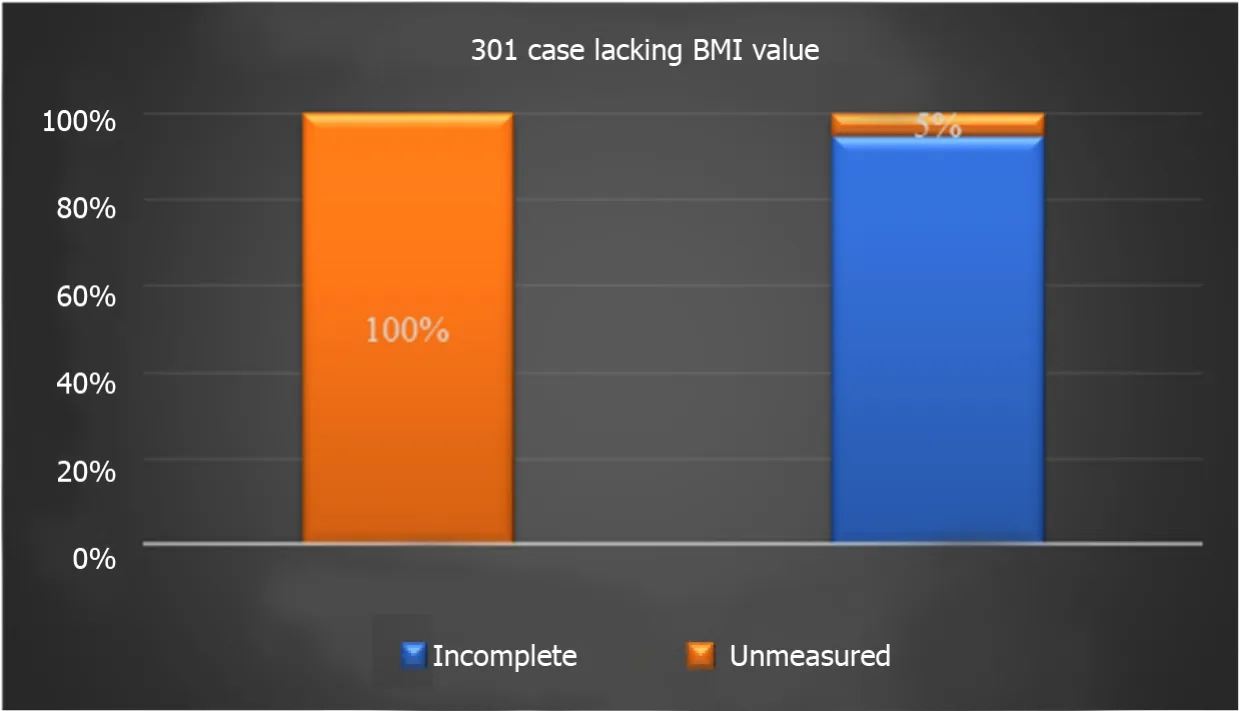
Figure 3 Proportions of missing body mass index values attributable to either missing height or weight.
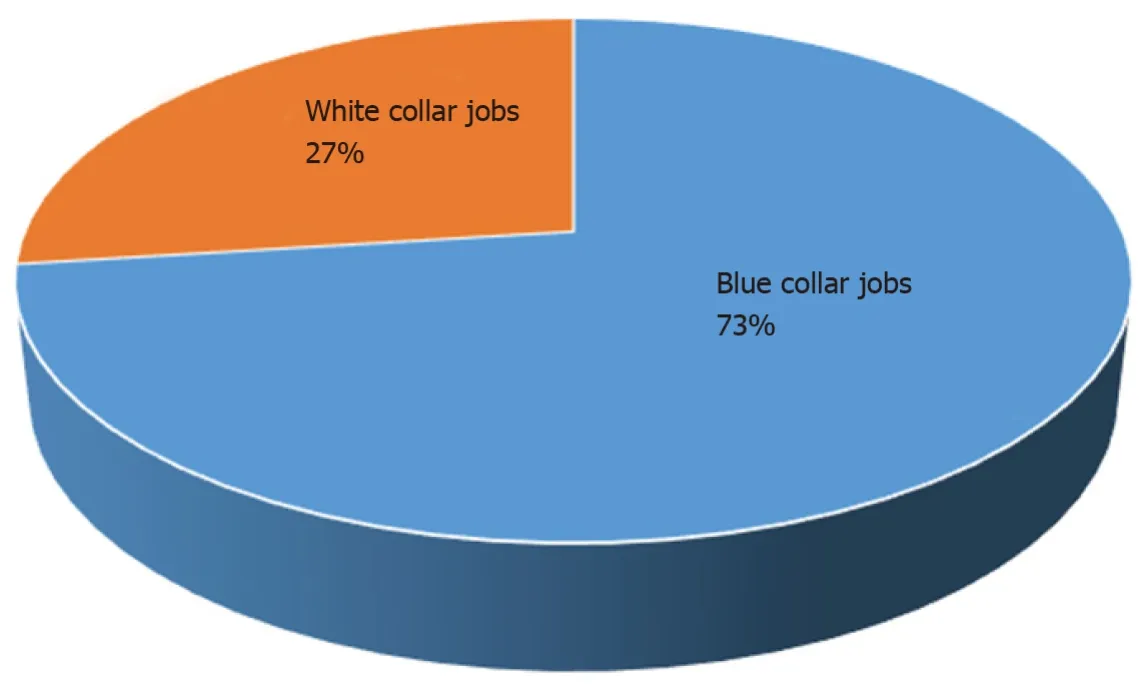
Figure 4 Distribution between manual and non-manual jobs.
Level of physical activities among participants
Evaluation of responses to exercise ADL indicated that over 50% of the respondents were not able to stretch or swim, while walking appeared to be the activity for most (Table 5).Evaluation of interference of basic ADL showed that ill health interfered mostly with respondents’ hobbies, but generally all people engaged in a variety of physical activities.
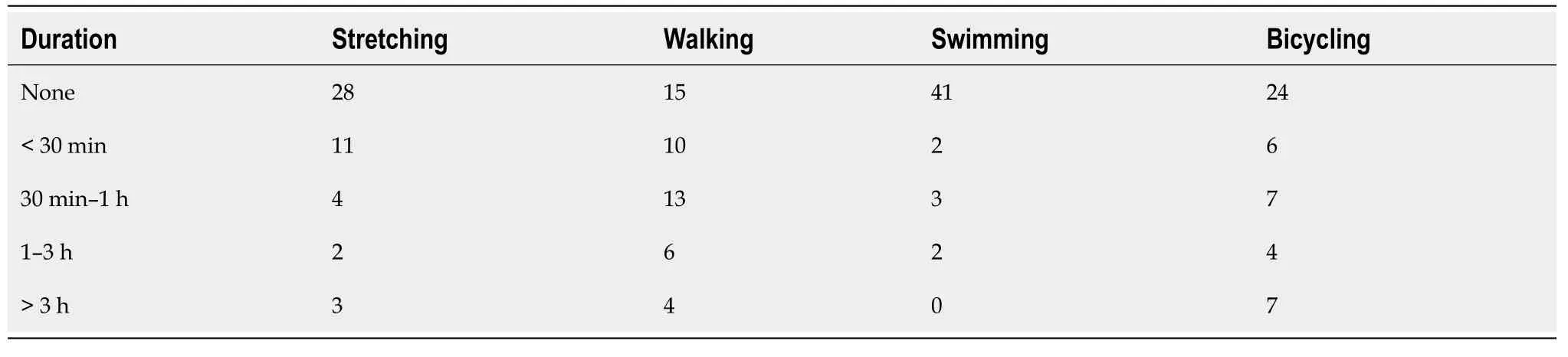
Table 5 Responses to exercise abilities, n = 48
Effect of diabetes on the ADL of participants in the community
When participants were categorized based on DM and hypertension + DM, the results showed that diabetes interfered with hobbies and work the most.However, the interference was minimal.The impact of hypertension + DM on all the surveyed ADL items was higher (moderate interference of hobbies and work) (Figure 5).
It was concluded that participants in manual jobs constituted about three-quarters of the diabetes patients.Nevertheless, the proportion of those in non-manual jobs with hypertension comorbidity was higher, which implies healthy occupational ADL as indicated by a preponderance of manual occupations in people with diabetes.The impact of ill health on leisure ADL was also indicated, especially that it was worse in those with hypertension comorbidity.This highlights that a pivotal focus on diabetes self-management regarding physical activities should include evaluation of the patient’s capacity to engage in ADL, especially as the impact of diabetes on ADL translates to a barrier of a therapeutic lifestyle regimen.Given that the interference of ADL by ill health was worse among those with hypertension and diabetes, both groups require different levels of care.
Effect of public education on food consumption
A baseline survey showed that 100% of rural farmers harvest cassava.The survey also showed that only 48% consumed cassava as one of their food choices, and 10% consumed wheat only and disregarded other options (Figure 6).This observation differed from other cohorts, such as urban dwellers who were wheat consumers and included a high proportion of educated people.After the public health lecture, the post-intervention survey showed a shift in consumption patterns, in favour of cassava products[39].
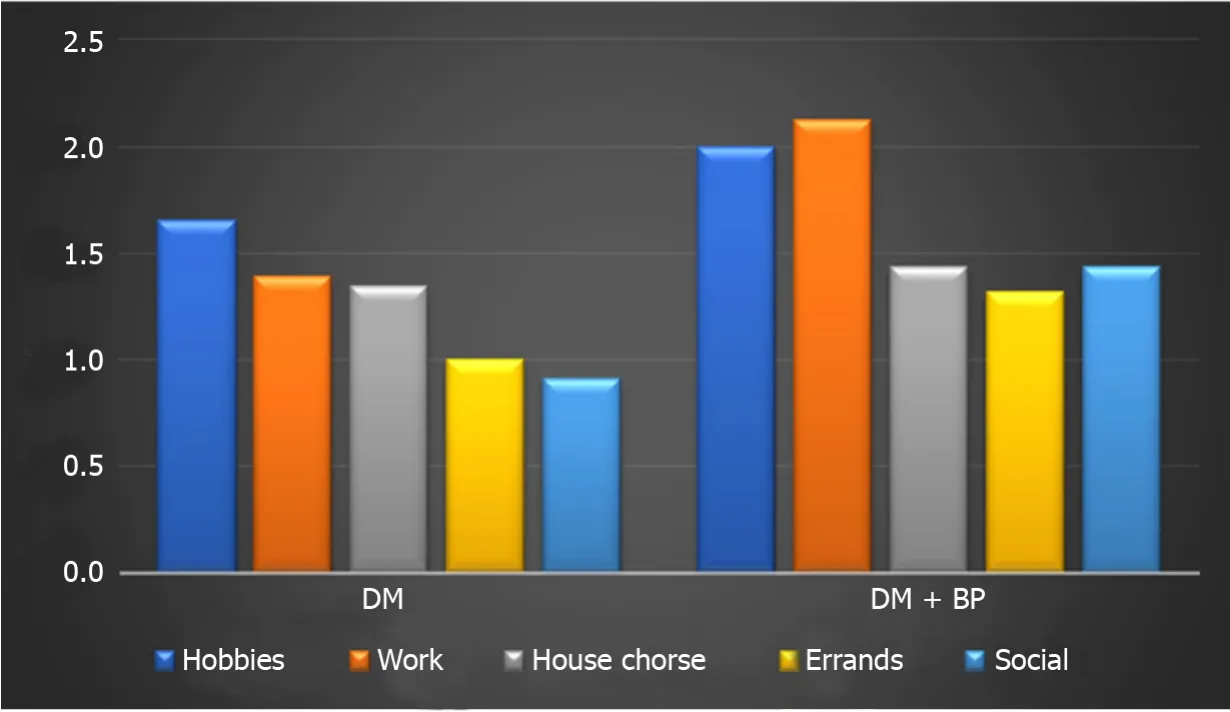
Figure 5 Average responses on interference of ill health on activities of daily living.
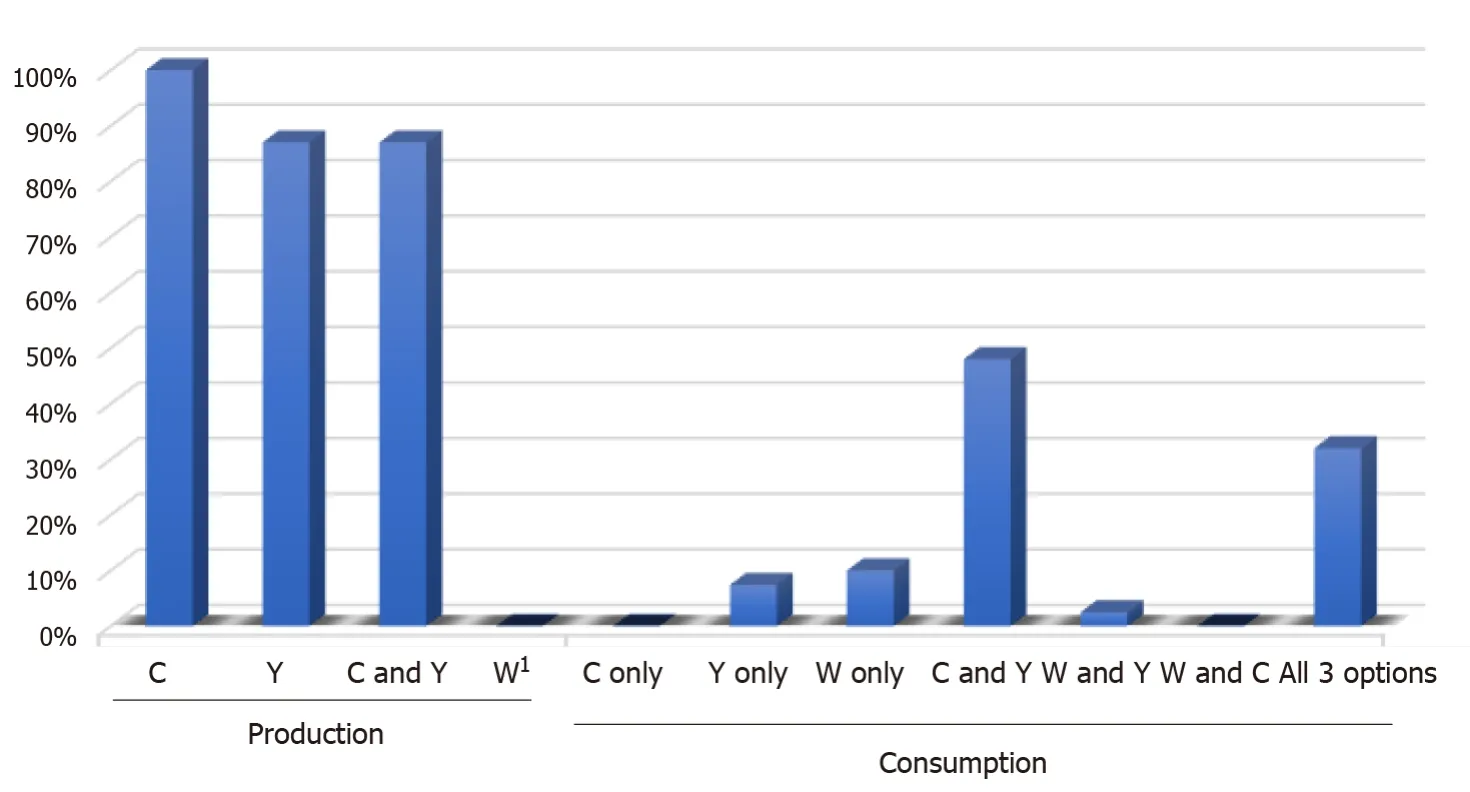
Figure 6 Consumption and production carbohydrate food choices.
WDD 2020 highlights
At WDD 2020, the IDF highlighted the following three urgent facts about Nigeria and diabetes: (1) Six million nurses are needed; (2) About 50% of adults living with diabetes are undiagnosed; and (3) Over 75% of people living with diabetes live in urban areas and are of working age.
Lessons from the event can be summarized in two themes.First, there is an underestimated burden of diabetes in terms of the nursing workforce requirement in PHC.During preparation for the event, it was determined that the 6 million projection is an underestimation.This determination was based on: (1)Australia being speculated to require about 120000 nurses in the next 10 years, which is 2% of the projected 6 million need[40]; and (2) More than 75% of people in African countries being undiagnosed for diabetes[41], making the actual burden yet to be estimated.This implies that Nigeria, with a population of over 200 million, needs to train and recruit many health care workers in diabetes care.Considering the current nursing workforce in the country, Nigeria will need more than the estimated 6 million.
Non-governmental organizations run diabetes screening services at community and PHC centres, but resident staff of the health care centres do not.Therefore, the knowledge is present but is not practiced, hence the apparent gap in knowledgevspractice.Importantly, most of the health care workers in the rural community-based PHC facilities are unaware of the WDD diabetes educator courses.However, these courses are well-received because the general hospitals requested a reschedule of the WDD from a Saturday to a weekday, in order for the staff to benefit.In addition, at three of the hospitals, the event was carried out twice, once for the general public and again for the hospital staff.
Telehealth
Our data indicates that 20% of the cases on medical records did not have phone numbers on record.However, 80% of the patients were able to receive servicesviatelehealth.A pertinent observation is that some of the phone numbers were actually owned by the patient’s child who was not living with the patient.Although many of the calls were unsuccessful, 34% of the cohort received telehealth services, and 29% of the sub-cohort received health advice (Figure 7).In light of the coronavirus disease 2019 pandemic and its effects on routine health care provision, this is an area that can be further utilised and expanded.
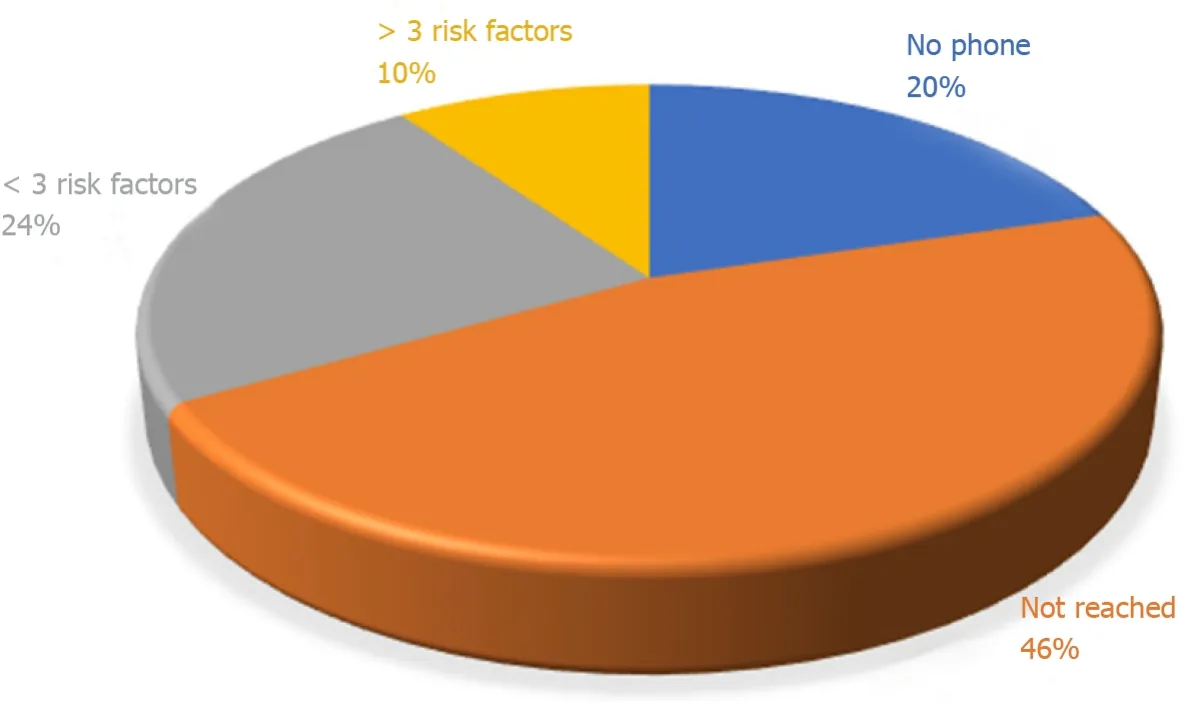
Figure 7 Distribution of cohort of cases assessed by telehealth.
DISCUSSION
This review highlighted some of the problems in diabetes research and practice.Specifically, the issues of GDM, nutrition in terms of carbohydrate food choices, PHC, and telehealth.Links have been made to the concept of behavioural change wheel (BCW_ regarding the gap between knowledgevspractice.BCW is important in managing chronic conditions.It is a guide for designing intervention programs, and it is predicated on capacity, motivation, and opportunity[26].It is a comprehensive framework for designing interventions by explicitly integrating behaviour theory to understand and target mechanisms of action within the intervention[27], and it is mindful that individual and collective behaviour change is key to implementing new practices and to improving health outcomes.It also incorporates context, which is key to effective design and implementation of interventions[28].
There has been a lack of clarity on the universal screening of pregnant women for GDM[42-44], and the result is that this service remains under-utilised[45].This low level of GDM screening service appears to represent a gap between knowledge and practice among the clinicians.The positive note is that GDM risk assessment for selective screening of pregnant women now exists[30-32].The user-friendly risk assessment sheet needs to be validated for local clinical use and integrated into GDM screening services.Two notable pieces of clinical knowledge include (1) BMI may be more reliable as a risk factor when measured in the first trimester, and (2) More weight measurements should be done because gestational weight gain is imperative in monitoring well-being of the baby and mother.Therefore, most antenatal clinics assess these at every visit, but height is documented at registration.This review highlighted the proportions of cases missing different necessary measurements and/or documentation.
Our cohort of 391 antenatal patients in the register were reviewed to determine the number of conclusive GDM diagnoses.This review was an addendum to a previous observation[15], and it was observed that 385 patients had a urine glucose test, out of which 16 (4%) were positive for glucosuria.Glucosuria may be found in about 50% at some point because of the associated changes in glomerular filtration rate.However, a follow-up blood sugar test for at-risk women is still essential[46].None of the 16 cases were followed-up with a blood sugar test.Instead, 5 other patients had blood glucose test results without urinalysis.Therefore, we do not know the incidence rate of GDM at our hospital.This highlights a knowledge and practice gap in antenatal patient laboratory test requisition and follow-up.
The four components of necessary diabetes education are: Adherence to medication, nutritional lifestyle, physical ADL, and up-to-date medical check-ups including laboratory tests[2,47,48].This review reported on carbohydrate nutrition and highlighted that people are still unaware of the values of their indigenous foods.This lack of knowledge was identified long ago[49], hence this report suggests that the problem is yet to be resolved.Therefore, more concerted efforts are needed to advance the knowledge of the glycaemic index of Nigerian carbohydrate foods.This report also highlighted physical ADL affordances and their effectiveness in the rural community.
PHC care is a function of the state, regarding the government’s policy and practice on health services.One of the issues, at least in developing communities such as Africa, is limited resources[50].However, studies on knowledge, attitude and practice have indicated that there are patient factors to consider[51].The Alma Ata declaration identified the necessity and potential of PHC to play a central hub role, and diabetes care services are encompassed[52].This report highlights a known problem that is still unresolved.
Therefore, it is recommended for the World Health Organization and other stakeholders (community, community leadership, policy makers and health care provision staff) to focus on PHC for diabetes care.For instance, looking at the Nigerian health care system, there are PHC centres scattered and operated by local governments, but the community dwellers rarely patronize the centres.By implication, the feedback to the government is hampered, and the impression is that “the government is not doing enough.” However, it is not entirely the fault of the governmentper se[18].This requires behavioural change of the community, inclusive of the ministry of health[53].It was reported from a BCW survey that about 40% of stakeholders agreed on the ability of PHC to offer diabetes services, whereas over 70% believed the motivation was poor[18].Therefore, this update highlights one area of need of BCW for IDF and the World Health Organization.
Over the past 3 years, translational research efforts have included development of a Diabetes Registry in the health facilities[17,54,55].It has been reported that a major factor to consider is concerted integration of telephone numbers of patients in medical files[54].For this obvious reason, the Global Medical Research and Development Organization is developing telehealth services for the area, of which telephone numbers are indispensable.
There is ongoing interest to utilise accessible and affordable telecommunication tools including telephones in community health service delivery[56-58].This review reported the potential to use the telephone for follow-up in rural communities.It also highlighted two limitations, which are non-documentation of the patient’s phone number or the patient providing another person’s telephone.This observation calls for awareness for health care providers to document phone numbers in patients’ records as well as alert patients on the importance of providing their own numbers.
CONCLUSION
These updated field note observations from ongoing research and topical research areas include prediabetes, diabetes registry, GDM screening concerns, PHC and telehealth potential for rural dwellers.From experience on the development of a diabetes register and intensive diabetes education, notes on BCW were reviewed and this is a work in progress, especially due to the negative impact of the coronavirus disease 2019 pandemic.Other field data included a cross-sectional study of ADL at two private hospitals.One of the important topics in diabetes care is that of PHC.There is a knowledge and practice gap for the important role that PHC must play in diabetes care, and this constitutes another point on BCW.This problem is likely confounded by the IDF and World Health Organization underestimating the nursing workforce.It is possible that a proactive PHC system equipped with various registries, such as a diabetes registry, could minimize the documentation issues as well as improving screening procedures.Mobile phones and internet services are becoming affordable and accessible, and research needs to focus on their utilisation.Future research should also advance BCW of all stakeholders (community, community leadership, policy makers and health care provision staff) to maximize the impact of diabetes research.
ACKNOWLEDGEMENTS
Some postgraduate and undergraduate students of the Public Health Department of Novena University supported the data collection during their research training, which have been duly published.This group includes Annette Orove, Edmond Anowa, Emmanuel Agege, Garba Ahmed, and Joseph Odoko.The staff and managements of Catholic Hospital Abbi, Donak Hospital Kwale, Eku Baptist Government Hospital, Friends Medical Laboratory Service and Novena University Health Centre are hereby appreciated.
 World Journal of Meta-Analysis2021年6期
World Journal of Meta-Analysis2021年6期
- World Journal of Meta-Analysis的其它文章
- Efficacy and safety of fingolimod in stroke: A systemic review and meta-analysis
- MicroRNAs as prognostic biomarkers for survival outcome in osteosarcoma: A meta-analysis
- Hydroxychloroquine alone or in combination with azithromycin and corrected QT prolongation in COVID-19 patients: A systematic review
- Newer developments in viral hepatitis: Looking beyond hepatotropic viruses
- Gastrointestinal tumors and infectious agents: A wide field to explore
- Preclinical safety, effectiveness evaluation, and screening of functional bacteria for fecal microbiota transplantation based on germ-free animals
