A nonagenarian patient with rhabdomyolysis and multiple organ dysfunction:a case report
Yan LIU, Xiao-Ming WANG, Ming-Tao XUE, Hong LI, Xin JIA, Xiao-Xuan NING
Department of Geriatrics, Xijing Hospital, Fourth Military Medical University, Shaanxi, China
Keywords: Continuous renal replacement therapy; Geriatrics; Hypoproteinemia; Infection; Rhabdomyolysis
Rhabdomyolysis (RM) refers to a pathological condition of skeletal muscle cell damage leading to the release of intracellular toxins into the blood circulation, resulting in potentially critical organ dysfunction and biochemical metabolic disorders.[1–3]The most common causes of RM are non-traumatic, such as drugs (i.e., statins), infections, breakthrough seizures, electrolyte disorders and metabolic diseases.[4–7]RM is rare in older adults and its etiology in this age-group can be multifactorial and complex.One study showed that falls (with or without immobilization) were the leading cause of RM in adults aged 65 years and older, accounting for 56.9% of all cases in this age-group.[8]RM due to hypokalemia, a common clinical electrolyte disorder affecting muscle cell membrane stability has also been reported in older adults.[9,10]
Multiple organ dysfunction can result from RM.Almost half of patients with RM develop acute renal failure and the mortality was reported to be 10.17% in the elderly.[8]Survival of RM patients depends on the underlying etiology,the extent of complications, and age of the patient.The shortterm mortality (death in 30 days) increases significantly with age and can be as high as 22.5%–60% in critically ill patients with acute renal failure.[10–13]When treated promptly and comprehensively with blood purification support, elderly patients with RM and acute kidney injury (AKI) may still recover completely.Continuous renal replacement therapy(CRRT) can be helpful for these patients as CRRT can efficiently remove myoglobulin and pro-inflammatory cytokines while maintaining stable hemodynamics and internal environmental homeostasis.[14,15]We hereby report a case of a nonagenarian patient with serious RM and multiple organ dysfunction who was successfully treated with measures including infection management, electrolyte supplement, fluid replacement, nutritional support and CRRT.
A 92-year-old male with pitting edema in both lower limbs, fatigue and anorexia was admitted to the Department of Geriatrics, Xijing Hospital, Fourth Military Medical University.The patient had developed bilateral lower limb pitting edema two months before, without fatigue, chest discomfort or shortness of breath.After treatment with cardiac diuretics, his symptoms subsided until two weeks before admission, when the lower-limb edema recurred.He also complained of severe fatigue and anorexia.The patient had a history of coronary heart disease and type 2 diabetes mellitus.His blood pressure had been normal with regular hydrochlorothiazide.No history of trauma, diarrhea, intoxication or alcohol intake was reported by the patient.
The patient was conscious with depressed mood at admission, and vital signs were normal (temperature: 36.4 °C;pulse: 76 beats/min; respiratory rate: 18 breaths/min; blood pressure: 134/64 mmHg).There was mild pitting edema in both lower extremities.Laboratory tests revealed moderate hypokalemia, mild anemia, hypoproteinemia and abnormal renal function, but not suggestive of infection (Table 1).The patient was admitted with a provisional diagnosis of coronary heart disease, diabetes mellitus, hypoproteinemia, hypokalemia and treated with diuretic, increasing myocardial blood supply, supplement of albumin, medicine of reducing blood-glucose,et al.Two days later, he developed cough,shortness of breath, hypoxemia and fever up to 38 °C.Chest X-ray found extensive opacification in lower lobe of the right lung consistent with infection.The status of the patient deteriorated as his daily urine volume decreased, and he developed lip cyanosis, muscle pain, orthopnoea, and soon after became unconsciousness.Laboratory findings suggested infection, AKI and progressive cardiopulmonary failure.Laboratory indices were as follows: white blood cell count (WBC): 10.87 × 109/L (normal: 3.5–9.5 × 109/L);creatinine: 170 μmol/L (normal: 53–115 μmol/L); cystatin C: 2.60 mg/L (normal: 0.51–1.09 mg/L); creatinine kinase(CK): 2,794 IU/L (normal: 26–174 IU/L); creatinine kinasemuscle/brain (CK-MB): 41 IU/L (normal: 0–25 IU/L); lactase dehydrogenase (LDH): 413 IU/L (normal: 114–240 IU/L);myoglobin: 774.2 ng/mL (normal: 0–70 ng/mL); N-terminal pro b-type natriuretic peptide (NT-ProBNP): 230,000 pg/mL;pH: 7.43 (normal: 7.35–7.45); oxygen partial pressure (PaO2):56 mmHg (normal: 80–100 mmHg); potassium: 2.7 mmol/L(normal: 3.5–5.5 mmol/L).
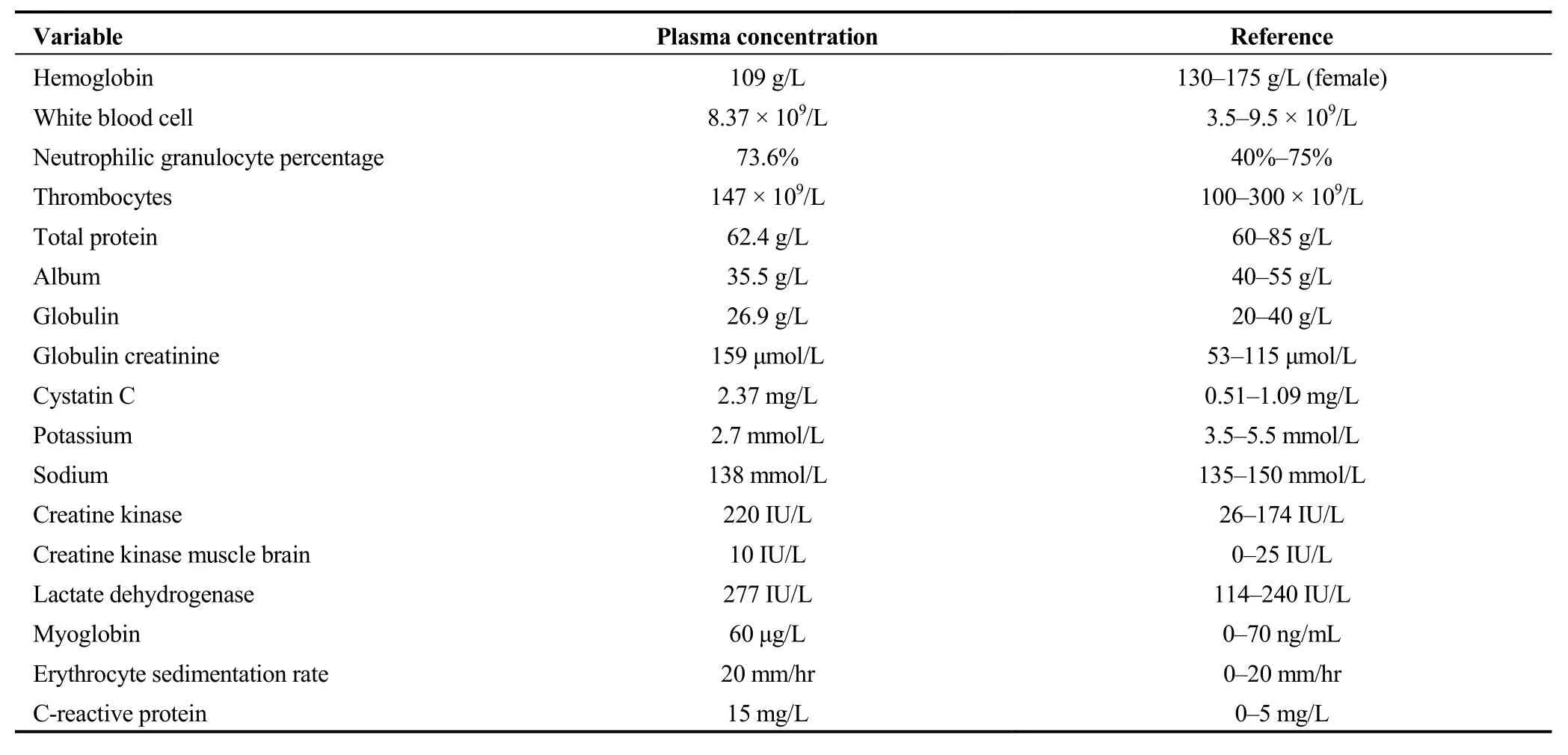
Table 1.Blood samples of the patient at the admission.
A diagnosis of RM was suggested and confirmed later based on the following laboratory tests.WBC elevated to 20.72 × 109/L, CK to 4,092 IU/L, CK-MB to 52 IU/L, LDH to 579 IU/L, myoglobulin to 4,024 μg/L, creatinine to 210 μmol/L, cystatin C to 2.94 mg/L, and NT-ProBNP to >35,000 pg/mL, PaO2dropped to 50 mmHg.The patient’s temperature increased to 39.5 °C and the lower limb edema worsened.Acute renal failure was identified when the patient’s daily urine volume dropped to less than 500 mL.A definite diagnosis of RM with multiple organ dysfunction was made.The patient had previously taken statins but had ceased more than two months prior to this episode.Hypokalemia was most likely caused by long-term thiazide diuretics.We hypothesize that this case of RM with multiple organ failure (heart, lung and kidney) was caused by hypokalemia and infection.
The patients received immediate CRRT support with other measures including high-flow nasal cannula oxygenation, volume expansion with plasma and crystalloids, potassium supplement, antibiotics (piperacillin sodium and tazobactam sodium) and nutritional support.The patient’s fever subsided after nine days, hypokalemia was rectified once CRRT commenced; infection was controlled after 14 days.Serum levels of CK, myoglobulin, LDH, and creatinine returned to normal after 14 days (Figure 1).CRRT was discontinued once the above indicators returned to normal.The patient was discharged one month after hospitalization and has been observed regularly for the last four years.During this time, the patient’s renal function has been normal, with an estimated glomerular filtration rate between 35–45 mL/min.
The most frequent causes of RM in the elderly are falls,followed by seizures, immobilization, sepsis, trauma or surgery, drugs, diabetic ketoacidosis, alcohol intoxication,vigorous exercise, infection, and others.[8]The patient reported here had taken statins for one year, but not together with other psychotropic drugs or macrolide drugs.Given that the statins were discontinued two months before the onset of symptoms, it is unlikely that they were contributing factors.The patient had a history of long term oral diuretic intake and hypokalemia lasting up to two months.Prolonged hypokalemia could have led to transportation of intracellular potassium, causing changes in the cell membrane action potential threshold, and enhancing cell membrane permeability, all of which may have contributed to the development of RM.In addition, pulmonary infection and high fever can aggravate ischemia and hypoxia of muscle cells, resulting in the depletion of adenosine triphosphate,which affects the exchange by sodium-potassium ATPase and the calcium-sodium pump.This increases the instability of the cell membrane, leading to the dissolution of muscle cells.Therefore, we suggest that RM in this case was caused by hypokalemia and infection.
The typical clinical manifestations of RM are myalgia,fatigue, and dark urine.[1–3,8]The manifestations of RM may be less typical in the elderly patients and our patient hadmyalgia, but no dark urine.RM in the elderly can therefore remain undiagnosed or be easily misdiagnosed given its low prevalence and atypical clinical features.Clinicians should be aware of RM as a differential diagnosis in the geriatric population.
Multiple organ failure, such as AKI can cardiorespiratory failure observed in our patient, can complicate the management of RM and significantly increase the risk of death.[12]The severity and urgency of the patient with RM need to be promptly recognized and treatment with correction of hypovolemia, alkalization of urine, removal of myoglobin from the circulation and kidney is critical measures for the management of AKI.[2,14]
Treatment of the underlying etiology is also important in reducing mortality from in patients with non-traumatic RM.Whereas in younger patients, RM is generally caused by a single etiological factor; RM in the elderly can potentially be caused by numerous conditions such as refractory or long-term hyperkalemia, metabolic acidosis, oliguria, or volume overload.As in this case, infection and hypokalemia were believed to be the causes and were treated with antibiotics and potassium supplementation.
In summary, RM is a severe and potentially fatal disease with lower prevalence but higher fatality in the elderly patients.In this case, the patient is very old, and complicated with multiple organ failure, atypical symptoms, coexistence of multiple complex diseases, all of which increase the difficulty of diagnosis and treatment for RM.Nevertheless, even in very elderly patients, prompt diagnosis and aggressive treatment can significantly improve excellent clinical outcomes.
Acknowledgments
This study was supported by the Natural Science Foundation of China (No.81870470) and the Xijing Hospital Subject Promotion Plan (XJZT18MDT 11 & XJZT18MJ31).All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2020年12期
Journal of Geriatric Cardiology2020年12期
- Journal of Geriatric Cardiology的其它文章
- Wild type transthyretin amyloidosis, a reason not to be forgotten for heart failure of preserved ejection fraction in the elderly
- Guiding extension catheter facilitated percutaneous coronary intervention for a dextrocardia patient with acute left anterior descending artery occlusion: a case report
- Can sacubitril/valsartan become the promising drug to delay the progression of chronic kidney disease?
- Venous thromboembolism prophylaxis-prescribing patterns among elderly medical patients in a Saudi tertiary care center: success or failure?
- Validation of methods for effective orifice area measurement of prosthetic valves by two-dimensional and Doppler echocardiography following transcatheter self-expanding aortic valve implantation
- Parity and carotid atherosclerosis in elderly Chinese women
