Venous thromboembolism prophylaxis-prescribing patterns among elderly medical patients in a Saudi tertiary care center: success or failure?
Dalal A.Alabdulkarim, Omar A.Almohammed, Maha A.Al Ammari, Nada S.Almaklafi,Munirah A.Alkathiri, Manal A.Aljohani
1Pharmaceutical Care Service, Ministry of the National Guard-Health Affairs, Riyadh, Saudi Arabia
2King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
3Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Abstract Background Hospitalized elderly patients are at high risk of venous thromboembolism (VTE), and the appropriate use of thromboprophylaxis can significantly reduce the incidence of VTE in high-risk patients.We investigated the pattern of VTE prophylaxis administration among elderly medical patients and assessed its appropriateness based on the American College of Chest Physicians (ACCP) recommendations.Methods A cross-sectional single-center study was conducted between October 2019 and March 2020, including hospitalized(> 48 h), elderly (≥ 60 years), medical patients, and excluding patients receiving anticoagulant for other reason, having contraindication to thromboprophylaxis, or had VTE diagnosed within 48 h.The Padua prediction score was used to determine the patients’ risk for VTE, and thromboprophylaxis use was assessed against the ACCP recommendations.Results The study included 396 patients with an average age of 75.0 ± 9.01 years, and most patients (71.7%) were classified as high risk for VTE development (Padua score ≥ 4 points).Thromboprophylaxis use was inappropriate in 27.3% of patients, of whom 85.2% were ineligible but still received thromboprophylaxis.Patients who were classified as low risk of VTE were more likely to receive inappropriate thromboprophylaxis (AOR = 76.5, 95% CI: 16.1–363.2), whereas patients with acute infection or rheumatologic disorder were less likely to receive inappropriate thromboprophylaxis (AOR = 0.46, 95% CI:0.22–0.96).Conclusions Although the use of thromboprophylaxis among high-risk elderly patients was reasonably adequate, a large proportion of low-risk patients were exposed to unnecessary risk through inappropriate overutilization of thromboprophylaxis.Thus, healthcare providers should accurately assess patients’ risk before prescribing thromboprophylaxis to ensure patient safety.
Keywords: Hemorrhage; Hospitalization; Prophylaxis; The elderly; Venous thromboembolism
1 Introduction
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism, is a medical condition where a blood clot forms inappropriately in a vein,leading to severe morbidity and mortality.[1]VTE places a major disease and financial burden on the healthcare system.[2]Moreover, many developed countries consider VTE as one of the major causes of preventable hospital deaths.[3]In the USA, VTE affects > 900,000 patients and results in >100,000 deaths annually.[4]Although no accurate incidence rate for VTE in Saudi Arabia (SA) is available, assuming that it is similar to those in other parts of the world, approximately 25,000 Saudis are affected by VTE annually.[5]
The incidence rate of VTE increases exponentially with age.Thus, the elderly are at a much higher risk than the general population,[6]and the risk is even higher among hospitalized elderly patients.[7]The incidence increase from 1 per 10,000 in young adults to 1 per 100 in the elderly.[4]Data from two large cohort studies found that the estimated lifetime risk of VTE after the age of 45 years was around 8%.[8]Moreover, elderly patients with acute VTE have a substantial long-term risk of VTE recurrence,[9]and higher mortality and VTE-related morbidity compared to elderly patients that didn’t have VTE.[6]A study found that overall in-hospital mortality among elderly patients with VTE was twice that of younger patients (6.6%vs.3.2%).[10]This high incidence of VTE among the elderly patients can be explained by the presence of other comorbidities,[11]and the impact of aging on the prothrombotic state.[12]
Without appropriate thromboprophylaxis, 10%–40% of medical or general surgery patients are at risk of VTE during their hospitalization, and the risk is even higher(40%–60%) if the patient is hospitalized for orthopedic surgery.[13]The American College of Chest Physicians (ACCP)guidelines recommend different situation-based thromboprophylaxis strategies.The recommended thromboprophylaxis in medically ill patients includes low-dose unfractionated heparin (LDUH) or low-molecular-weight heparins.Mechanical methods of thromboprophylaxis, such as compression stockings, are urged for patients with contraindications to pharmacological thromboprophylaxis or those with a high risk of bleeding.[13]Although these guidelines are regularly updated and provide clear criteria for the use of VTE prophylaxis, their appropriate utilization remains a major concern.
The Padua prediction score model was introduced to predict the risk of VTE development among hospitalized medical patients and to identify those who could benefit from thromboprophylaxis.[14]The risk value assigned to each patient characteristic ranges from 1–3 points, based on its contribution to the overall risk of VTE, and the patient score is calculated as the sum of these points.A total score ≥ 4 indicates a high risk of VTE, identifying the patient as a candidate for thromboprophylaxis.Among patients with a Padua score of ≥ 4, the prediction model found a significant difference in the VTE risk between patients who received thromboprophylaxis versus those who did not [2.2%vs.11.0%,hazard ratio = 0.13, 95% confidence interval (CI): 0.04–0.40].[14]
Before the Padua prediction score model was introduced,multiple international and national studies revealed a gap between guidelines’ recommendations and real-world practice.In 2004, a study assessing the use of thromboprophylaxis in real-world practice using an international registry found that only 29% of patients with confirmed DVT had received thromboprophylaxis before DVT development.[15]Later, the ENDORSE study reported that although > 50% of hospitalized patients were eligible to receive thromboprophylaxis, only half of them did.[16]Moreover, a multinational study of 2,266 patients (including 200 from hospitals in SA) found low compliance to VTE prophylaxis guidelines, as only 40% and 36% of medical and surgical patients,respectively, received appropriate thromboprophylaxis.[17]Furthermore, another study conducted in seven major hospitals in SA found that only 41% of VTE patients had received appropriate VTE prophylaxis before the event (63%and 35% of surgical and medical patients, respectively).[18]Thus, a high proportion of hospitalized patients were not receiving appropriate VTE prophylaxis, even if they were eligible.
Poor adherence to VTE prophylaxis guidelines for hospitalized medical patients exposes them to serious risk with preventable consequences that impact patients’ and healthcare systems’ outcomes.This risk is even higher among the elderly, where the inappropriate use of thromboprophylaxis would worsen their outcomes.Thus, we conducted this study to determine the pattern of VTE prophylaxis use among elderly medical patients and assess the appropriateness of its use based on the ACCP recommendations.
2 Methods
2.1 Study design
We conducted a six-month cross-sectional study (between October 2019 and March 2020) to determine the pattern of VTE prophylaxis use and its appropriateness based on the ACCP recommendations.The study was conducted at King Abdulaziz Medical City (Riyadh, SA), a tertiary care, academic medical center with approximately 1,500 beds.The study protocol was reviewed and approved by the Institutional Review Board at King Abdullah International Medical Research Center.
2.2 Study population
All medical patients who were admitted to the Medical City from October 2019 through March 2020 were retrospectively evaluated for eligibility.Patients were included if they were ≥ 60 years old and admitted for an acute medical illness that required hospitalization in a medical ward for >48 h.Patients were excluded if they were receiving anticoagulant treatment at a therapeutic dosage for another reason,had a known contraindication to pharmacological VTE prophylaxis (e.g., allergy, platelet count < 50 × 109/L, or active bleeding upon admission), or had VTE that was diagnosed within 48 h of admission.
2.3 Data collection
Data were collected from hospitalized patients’ electronic medical records and included demographic information, the reason for admission, preexisting comorbidities, risk factors for VTE based on the Padua prediction score, and the use of VTE prophylaxis.
2.4 Appropriateness of prescribing VTE prophylaxis
The appropriateness of prescribing VTE prophylaxis was evaluated based on the risk level according to the Padua prediction score (patients with ≥ 4 points were considered high risk and expected to receive thromboprophylaxis),[14]and against the recommendations of the 9thedition of the ACCP guidelines.[19]The prescribed thromboprophylaxis was considered appropriate if the patient was eligible and received proper VTE prophylaxis (type and dosage) or was ineligible and did not receive it.Prescribing was considered inappropriate if the patient was eligible and did not receive proper VTE prophylaxis (type and dosage) or if the patient was ineligible but received thromboprophylaxis.
2.5 Statistical analysis
Descriptive statistics, including mean ± SD as well as frequencies and percentages, were used to describe patients’characteristics.Univariate and multivariate logistic regression were performed to assess patients’ characteristics and risk factors that were associated with inappropriate thromboprophylaxis use.The literature reported that approximately 40% of all patients were expected to have a high risk of VTE, based on the Padua prediction score.[14]Assuming that we would have the same proportion of patients with high risk among our study population and using an α-value of 0.05 and 80% power, data for at least 369 patients were estimated as required to determine any difference in the appropriateness of prescribing of VTE prophylaxis.An α-value < 0.05 was considered statistically significant.The data were coded, checked for accuracy, and analyzed using SPSS Statistics version 25.0 software for Windows (SPSS,IBM Corp., Armonk, NY, USA).
3 Results
Of the 698 adult patients admitted to the Medical City between October 2019 and March 2020 who were initially screened for eligibility, 396 elderly and medically ill patients were included in the study, and 302 patients were excluded for meeting one or more of the exclusion criteria.
3.1 Patients’ characteristics
The mean age of our study cohort was 75.0 ± 9.1 years,and 43.2% of them were female.Hypertension, diabetes mellitus, and chronic kidney disease were present in 79.3%,75.8%, and 35.4% of the patients, respectively.Most patients received thromboprophylaxis (94%), and LDUH was the most commonly used (79.0%).The patients’ characteristics are summarized in Table 1.
3.2 Risk factors for VTE among patients
Most patients (71.7%) were classified as high risk for VTE development (Padua score of ≥ 4).The most common risk factor for VTE was patients aged ≥ 70 years old (67.7%),followed by reduced mobility for ≥ 3 days (63.9%), acute infection or rheumatologic disorder (58.3%), and heart or respiratory failure (32.3%) (Tables 1 & 2).
3.3 Appropriateness of thromboprophylaxis use
The use of thromboprophylaxis in 27.3% of patients was inappropriate.Of them, 85.2% were ineligible but received thromboprophylaxis anyway, whereas 12.0% were eligible but did not receive any thromboprophylaxis, and a small portion (2.8%) were eligible but received an inappropriate thromboprophylaxis dose (Table 3).
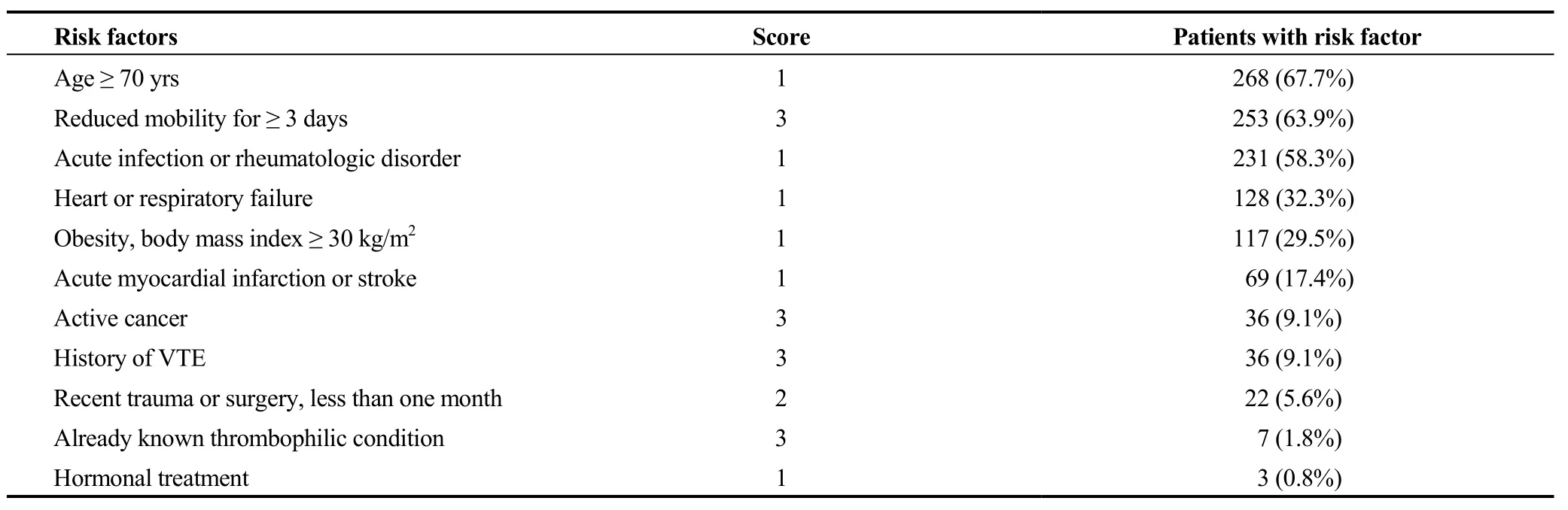
Table 2.Risk factors for VTE among the study subjects (n = 396).

Table 3.Appropriateness of thromboprophylaxis use in our patient cohort (n = 396).
3.4 Factors associated with inappropriate use of thromboprophylaxis
Patients’ clinical characteristics and risk factors for VTE were checked for their association with the inappropriate use of thromboprophylaxis using univariate followed by multivariate logistic regression.Patients with a lower risk of VTE (Padua score < 4) were much more likely to receive inappropriate thromboprophylaxis [crude odds ratio (COR)= 77.0, 95% CI: 38.3–154.9] than patients with a higher risk of VTE (Padua score ≥ 4).When comparing patients younger than 70 years old with older patients, those aged ≥ 70 years old were less likely to be managed inappropriately (COR =0.45, 95% CI: 0.29–0.72).Likewise, compared with patients without cancer or history of VTE, patients with cancer(COR = 0.22, 95% CI: 0.06–0.73) or history of VTE (COR= 0.22, 95% CI: 0.06–0.73) were less likely to receive inappropriate thromboprophylaxis.Furthermore, patients with reduced mobility for ≥ 3 days (COR = 0.04, 95% CI: 0.03–0.08) or acute infection (COR = 0.46, 95% CI: 0.29–0.72)were less likely to receive inappropriate thromboprophylaxis.
However, when assessing the effects of the significant univariate variables in the multivariate logistic regression model, they became insignificant except for two variables,namely, the Padua risk score classification [adjusted odds ratio (AOR) = 76.5, 95% CI: 16.1–363.2] and the acute infection criterion (AOR = 0.46, 95% CI: 0.22–0.96), which remained significant and in the same direction.The distribution of the appropriateness of thromboprophylaxis based on the patients’ clinical characteristics and risk factors for VTE,along with the results from the univariate and subsequent multivariate logistic regression, are summarized in Table 4.
4 Discussion
This study was conducted to determine the pattern and assess the appropriateness of using VTE prophylaxis based on the ACCP guidelines among elderly (≥ 60 years) medical patients who were admitted to a tertiary medical center in SA.Most of the patient cohort (71.7%) were classified as high risk (Padua score ≥ 4) for VTE development, and therefore required the administration of thromboprophylaxis.Since our study focused on elderly patients, the most common identified risk factors for VTE included patients aged ≥70 years old (67.7%), followed by reduced mobility for ≥ 3 days (63.9%) and acute infection or rheumatologic disorder(58.3%).Unfortunately, the use of thromboprophylaxis was inappropriate in more than one-quarter (27.3%) of patients,most of whom (85.2%) were exposed to unnecessary risk.This finding was emphasized in the multivariate logistic regression model, where we found that patients who were classified as low risk of VTE (Padua score < 4) were more likely to receive inappropriate thromboprophylaxis (AOR =76.5, 95% CI: 16.1–363.2).
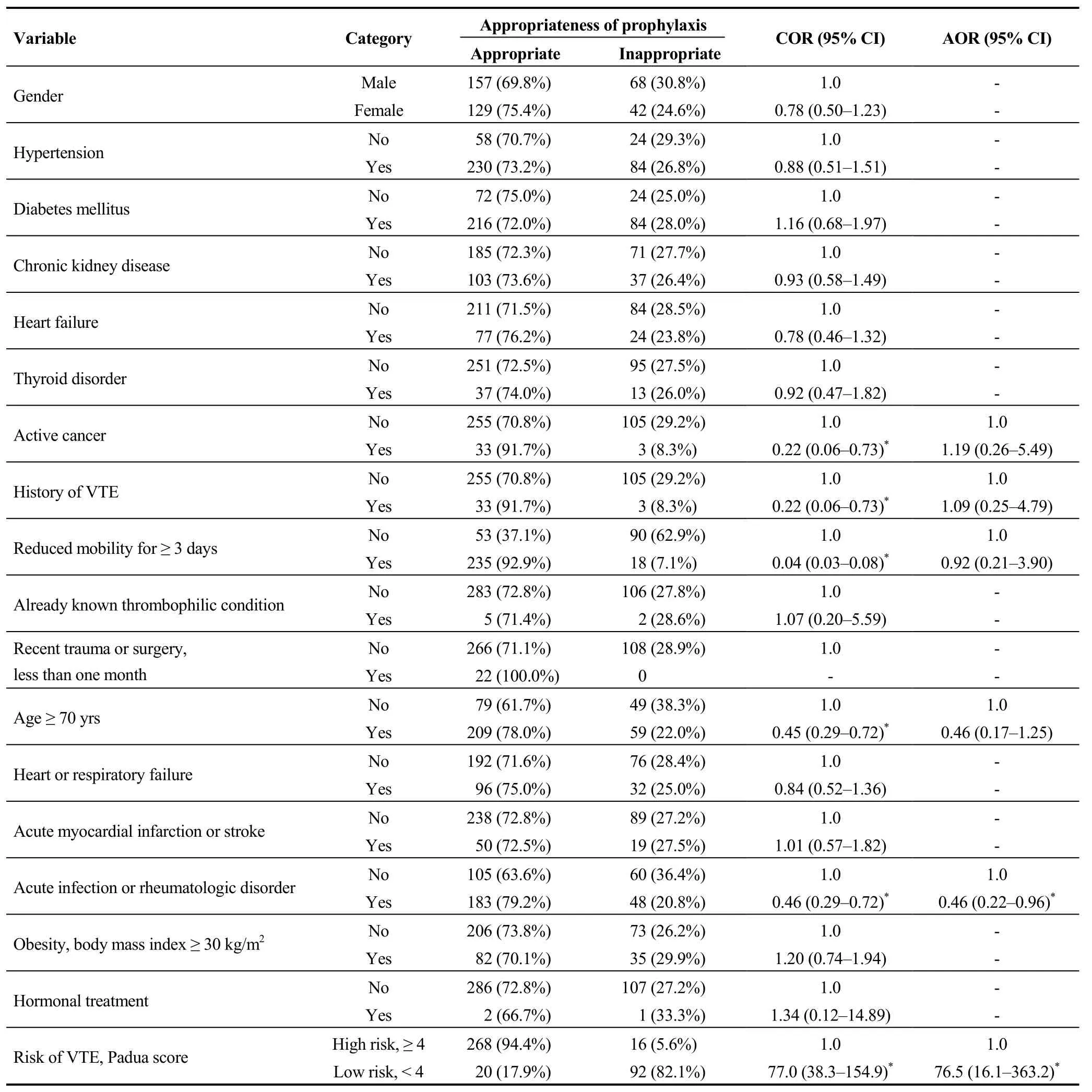
Table 4.Factors associated with inappropriate use of thromboprophylaxis.
Thromboprophylaxis use in nearly three-quarters (72.7%)of our study subjects was appropriate.In contrast, other national studies have reported a much lower rate of appropriate thromboprophylaxis use.One study reported that although 91% of their patients were at high risk for VTE and candidates for thromboprophylaxis, only 38% of them received ACCP-recommended VTE prophylaxis.[20]In our study, 71.7% of patients were considered high risk, but only 94.4% of them received appropriate thromboprophylaxis.Another study in SA evaluated VTE patients and found that only 41% of them received appropriate thromboprophy-laxis.[18]However, better results were previously achieved in other hospitals in SA, such as a study evaluating the use of thromboprophylaxis at a tertiary hospital in the Aseer region in SA, where 80% of eligible patients received appropriate thromboprophylaxis.[21]In comparison with this, among the 295 patients who were eligible to receive thromboprophylaxis in our study, 279 (94.5%) received appropriate thromboprophylaxis, which is a much higher rate.Although the rate of appropriate thromboprophylaxis in our present study was not appalling, that might be because all patients were ≥60 years old, which is a known risk factor for VTE.Thus,they were more likely to receive thromboprophylaxis.
When comparing our results with other international findings, multiple studies have reported a much lower rate of appropriate VTE prophylaxis use.The multinational AVAIL ME study reported a low rate of compliance with VTE prophylaxis guidelines, and only 40% of medical patients received appropriate thromboprophylaxis.[17]Amin,et al.[22]assessed the appropriate utilization of thromboprophylaxis in USA medical centers and revealed appropriate use in approximately 34% of patients.Another similar multicenter study evaluating the use of thromboprophylaxis in acutely ill medical patients reported that although thromboprophylaxis was indicated in 90% of the study patients, only 16%received the treatment.[23]Moreover, another study reported that only 13% of at-risk patients received the appropriate type, dose, and duration of thromboprophylaxis recommended in the ACCP guidelines.[24]Therefore, the rate of appropriate thromboprophylaxis use in our study is better than the rate reported in others, but this does not negate the fact that better outcomes can be achieved by avoiding the exposure of these patients to unnecessary risk.
Another important finding of our study was that among patients classified as having received inappropriate thromboprophylaxis (27.3%), most of them received thromboprophylaxis (85.2%) when they were not supposed to.Similarly, another study found that low-risk patients were over-treated.[25]These findings indicate that clinicians are inadequately assessing patients’ risk of VTE, and low-risk patients are exposed to unnecessary risk.
Our findings highlight the need for healthcare providers to accurately assess patients’ risk before administering thromboprophylaxis so that the appropriate decision can be made to avoid the under- or overutilization of thromboprophylaxis.The appropriate use of thromboprophylaxis (mainly anticoagulant medications) in patients who are at high risk of VTE is a life-saving and cost-effective strategy,[26]but its use in low-risk patients adds extra cost and exposes them to unnecessary risks of bleeding.Therefore, the appropriate use of thromboprophylaxis should be a major consideration for hospitalized patients because of the increased risk.Poor adherence to guidelines significantly affects patient health and increases the incidence of VTE, bleeding, and other associated complications that, in turn, increase the overall cost of care for hospitalized patients.
4.1 Limitations
The cross-sectional nature of our study limits the cause and effect relationship between independent and dependent variables, and our findings should be interpreted taking this into consideration.Furthermore, this was a single-center study, and the results should not be generalized to other hospitals in SA.Therefore, multicenter, prospective studies with a larger sample size are necessary to confirm our findings.
4.2 Conclusions
The incidence of VTE among hospitalized patients is a major and preventable health condition that places an avoidable financial burden on any healthcare system.We found that the use of thromboprophylaxis among high-risk elderly patients was fairly adequate.However, there was a large proportion of patients who were exposed to unnecessary risk through the inappropriate overutilization of thromboprophylaxis in patients who were low risk of VTE.Therefore, healthcare providers need to be reminded of the importance of accurately assessing a patient’s risk before administering thromboprophylaxis so that the appropriate decision is made and under- or overutilization of thromboprophylaxis is avoided.
Acknowledgments
This study was supported by the Researcher Supporting Project (RSP-2020/77), King Saud University, Riyadh, Saudi Arabia.All authors had no conflicts of interest to disclose.The authors gratefully thank the Deanship of Scientific Research and RSSU at King Saud University for their technical support, and Enago® for English language editing of the manuscript.
 Journal of Geriatric Cardiology2020年12期
Journal of Geriatric Cardiology2020年12期
- Journal of Geriatric Cardiology的其它文章
- Advances in Journal of Geriatric Cardiology over the course of a decade
- Catheter ablation for atrial fibrillation is associated with reduced risk of mortality in the elderly: a prospective cohort study and propensity score analysis
- Effects of angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker on one-year outcomes of patients with atrial fibrillation: insights from a multicenter registry study in China
- Parity and carotid atherosclerosis in elderly Chinese women
- Validation of methods for effective orifice area measurement of prosthetic valves by two-dimensional and Doppler echocardiography following transcatheter self-expanding aortic valve implantation
- Can sacubitril/valsartan become the promising drug to delay the progression of chronic kidney disease?
