Parity and carotid atherosclerosis in elderly Chinese women
Xiao-Yan WANG, Fei YE, Li-Xiong ZENG, Shan TU, Wen-Zhi LUO, Xu DENG, Zhi-Hui ZHANG
Department of Cardiology, the Third Xiangya Hospital, Central South University, Changsha, China
Abstract Background The relationship between parity and atherosclerosis has been reported in some ethnic populations.However, results regarding Chinese women are still lacking.This study aimed to investigate the association of parity and carotid atherosclerosis, which has a predictive value of subsequent atherosclerotic events in elderly Chinese women.Methods A total of 2,052 participants from the medical examination center of the Third Xiangya Hospital were enrolled in the study.A standardized, structured questionnaire was administered to collect information on subjects’ demographic characteristics, socioeconomic status, and cardiovascular risk factors.High-resolution ultrasound was used to examine carotid plaques and carotid intima-media thickness (IMT).Results The mean age of participants was 66.1 ± 5.5 years.Women with more birth appeared to have a higher risk of carotid artery plaques.A multivariate-adjusted model yielded an odds ratio of 1.38 (95% CI: 12%–70%, P = 0.003) per birth.A positive association was observed between parity and common carotid IMT (β ± SE:0.029 ± 0.006, P < 0.001), and internal carotid IMT (β ± SE: 0.011 ± 0.005, P = 0.03) in a univariate model; however, these associations became non-significant in multivariate-adjusted models.When common carotid IMT was classified into an IMT ≥ 1 mm group and an IMT< 1 mm group, higher parity was associated with more obvious thickening both in the unadjusted model (OR = 1.61, 95% CI: 1.29–2.00, P <0.001) and in the fully adjusted model (OR = 1.43, 95% CI: 1.09–1.88, P = 0.01).Conclusions There is a positive association between parity and risk of carotid plaques, as well as between parity and risk of obvious thickening for common carotid IMT in elderly Chinese women, indicating multiparous women might experience more atherosclerotic challenges.
Keywords: Atherosclerosis; Elderly women; Parity
1 Introduction
The association between parity and atherosclerosis risk in women has been assessed in several studies.[1–7]Some studies have found that increased parity was associated with an increased atherosclerosis risk,[1–3,6,7]whereas other studies observed no association or even an increased risk of nulliparity.[4,5]Despite these conflicting evidences, the majority of previous studies have demonstrated a positive association.
Pregnancy is always accompanied by a series of important changes for women, including changes in sex hormone levels, hemodynamics, and insulin resistance.It is also associated with structural and functional changes in the cardiovascular system.[8]The relationships between parity and risk of cardiovascular diseases have been investigated in several prospective studies.[9,10]Because of a low incidence of clinical cardiovascular events in parous women, especially in young individuals,[11]it would be more meaningful to investigate the association between parity and cardiovascular diseases in older adults.Carotid atherosclerosis, including the presence of carotid plaques and the carotid intima-media thickness (IMT), used to be considered as a well-validated marker for atherosclerotic burden.[12,13]It has an important predictive value for subsequent cardiovascular events, such as myocardial infarction and stroke.Changes in carotid IMT have also been adopted as a surrogate endpoint to assess the effect of lipid-lowering agents.[14]The association between parity and carotid atherosclerosis has been reported in other ethnic populations,[1–7]but the results on elderly Chinese women are lacking.Herein, we performed a cohort study with women aged ≥ 60 years, aiming to assess the association between parity and carotid atherosclerosis in this cross-sectional analysis.
2 Methods
2.1 Study population
Participants were recruited from the medical examinationcenter of the Third Xiangya Hospital between January 2016 and December 2019.The inclusion criteria were defined as women aged ≥ 60 years with detailed information on parity and carotid artery plaques available.The exclusion criteria included female individuals aged < 60 years and those with missing data on parity and carotid plaque.Fifteen nulliparous women were also excluded from the current analysis due to small sample size.A total of 2,052 participants remained for statistical analysis.The study was conducted according to the guidelines of the Helsinki Declaration, approved by the Institutional Ethics Review Committee, and all participants provided written informed consent.
2.2 Assessment of baseline characteristics
A standardized, structured questionnaire was administered by well-trained interviewers to collect information on subjects’ demographic characteristics, socioeconomic status,marital history, cardiovascular risk factors, and medical history.Parity distribution in the present study is shown in Table 1.Parity was classified into four categories: one, two,three, and four or more pregnancies (Table 2).

Table 1.Parity distribution in the present study.
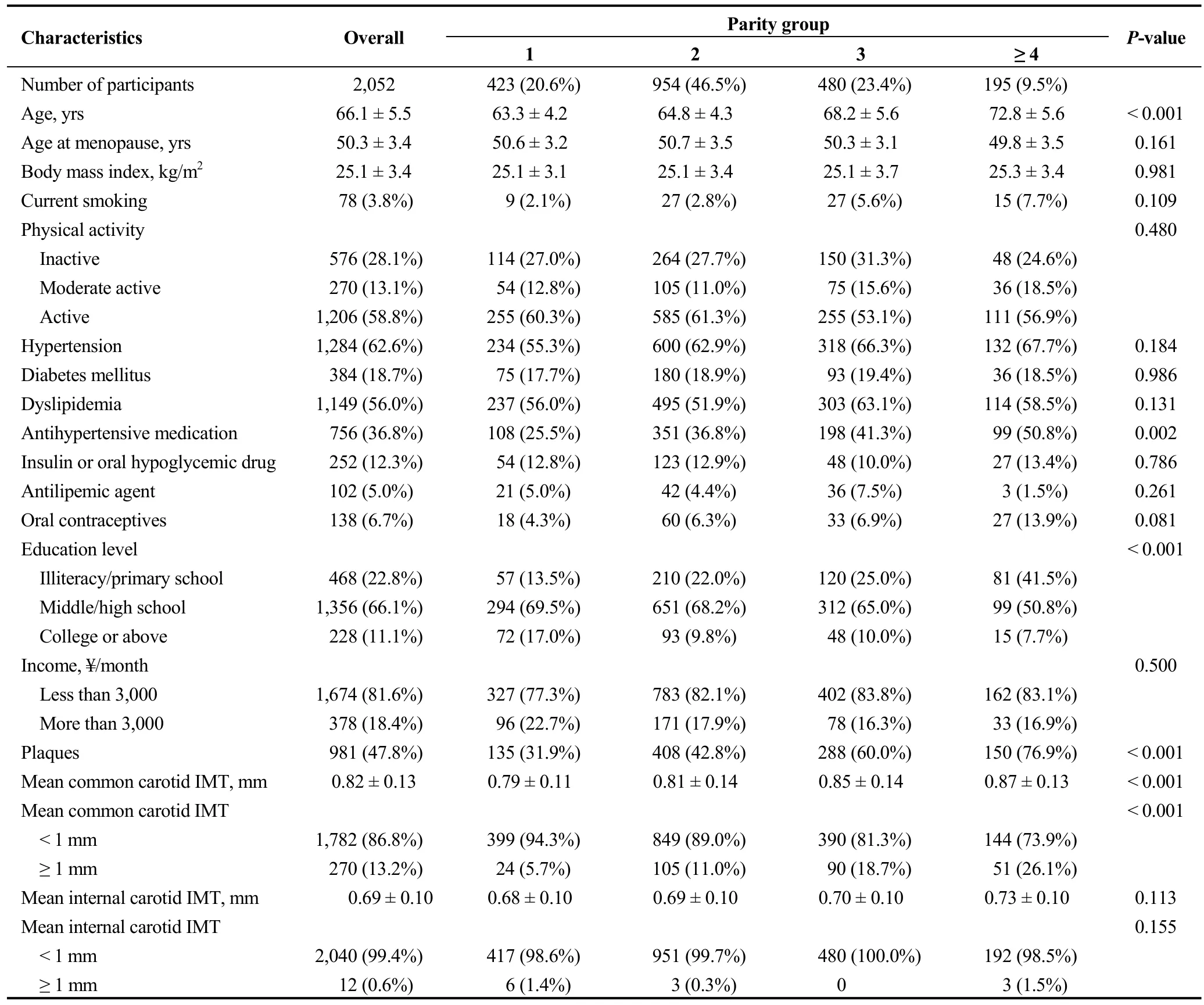
Table 2.Baseline characteristics of participants stratified by parity.
2.3 Assessment of carotid artery plaques and IMT
In brief, carotid artery was assessed by certified sonographers blinded to participants’ clinical characteristics.High-resolution B-mode ultrasound (Philips iU-22 ultrasound system by Philips Medical Systems, Bothell, WA,USA) with a 5–12 MHz linear array transducer was used to detect plaques bilaterally on three segments: the common carotid artery, the bifurcation, and the internal carotid artery.IMT was defined as the distance from the leading edge of the lumen-intima interface to the leading edge of the mediaadventitia interface on a longitudinal image of each carotid artery.Carotid plaque was defined as a focal structure encroaching into the arterial lumen of at least 0.5 mm or 50%of the surrounding IMT value, or a thickness > 1.5 mm, as measured from the media-adventitia interface to the intima-lumen interface.Carotid atherosclerosis was considered as the presence of plaques at one or more sites.No attempt was made to quantify the size or extent of the lesions.IMTs of the bilateral common carotid artery and the internal carotid artery were then averaged to get a mean IMT value for each subject.Mean carotid IMT ≥ 1 mm was considered an obvious thickening, while mean carotid IMT< 1 mm was normal.[15]IMTs were measured twice by the same technician for subsequent assessment of interpreter reproducibility.The results were reviewed by two independent sonographers.Discrepancies between their evaluations were resolved by consensus.
2.4 Statistical analysis
Comparisons between parity groups were tested using one-way ANOVA for continuous variables or using Pearson’s chi-square tests for categorical variables.Ordinal variables and continuous variables with skewed distributions were compared using nonparametric methods.The associations between parity and carotid artery plaques and between parity and common carotid IMT thickening were examined through logistic regression models.The association of parity with carotid artery IMT was analyzed using multivariate linear regression models.Results of logistic regression models were presented as an odds ratio (OR)with 95% confidence interval (CI), and results of linear regression models were presented as an unstandardized β-coefficient and standard estimate (SE).Potential confounders,including age, hypertension, diabetes mellitus, dyslipidemia,education level, income, current smoking, body mass index(BMI), physical activity, antihypertensive medication, insulin use, oral hypoglycemic drug intake, antilipemic agents,and use of oral contraceptives, were adjusted in these models.A parity of one was considered as the reference value in all models.A two-sidedP-value < 0.05 was considered statistically significant.All statistical analyses were performed with SAS 9.4 (SAS Institute Inc, Cary, NC, USA).
3 Results
3.1 Baseline characteristics
Parity in this study ranged from one to a maximum of six birth (Table 1).Table 2 shows the baseline characteristics of participants according to parity group.It seemed that age increased with higher parity (P< 0.001), while age at menopause showed no difference among parity groups (P=0.161).The presence of antihypertensive medication increased significantly with parity (P= 0.002); however, there was no difference in the prevalence of hypertension, diabetes mellitus, dyslipidemia, or use of hypoglycemic drugs, antilipemic agents, and oral contraceptives.Interestingly, education level showed a statistically significant difference among parity groups (P< 0.001).The proportion of elderly women with illiteracy or primary school education increased with parity, and those with middle school, high school, or college education and above decreased significantly with parity.
3.2 Association between parity and carotid artery plaques
The association between parity and carotid artery plaques is shown in Figure 1.Women with more birth seemed to have a higher risk of carotid artery plaques compared to those who had only one birth.Logistic regression analysis yielded an age-adjusted OR of 1.44 (95% CI: 1.18–1.75,P< 0.001) per birth.Additional adjustment for hypertension,diabetes mellitus, and dyslipidemia did not alter this association (OR = 1.43, 95% CI: 1.17–1.74,P< 0.001).In the multivariate-adjusted model, the risk of carotid artery plaques increased by 38% (95% CI: 12%–70%,P= 0.003)per birth after fully adjusting for age, hypertension, diabetes mellitus, dyslipidemia, education level, income, current smoking, BMI, physical activity, and use of antihypertensive medication, insulin or oral hypoglycemic drugs, antilipemic agents, and oral contraceptives.
3.3 Association between parity and carotid artery IMT
As shown in Table 3, it appears that there is a positive association between parity and mean carotid artery IMT in the unadjusted model, while linear regression analysis demonstrated a β of 0.029 (SE = 0.006,P< 0.001) for common carotid IMT, and a β of 0.011 (SE = 0.005,P= 0.03)for internal carotid IMT.In multivariate-adjusted models,these associations became statistically non-significant.

Figure 1.Association between parity and carotid artery plaques.Model 1: unadjusted.Model 2: adjusted for age.Model 3: adjusted for age, hypertension, diabetes mellitus and dyslipidemia.Model 4: adjusted for age, hypertension, diabetes mellitus, dyslipidemia, education level, income, current smoking, body mass index, physical activity, antihypertensive medication, insulin or oral hypoglycemic drug, antilipemic agent and oral contraceptives.
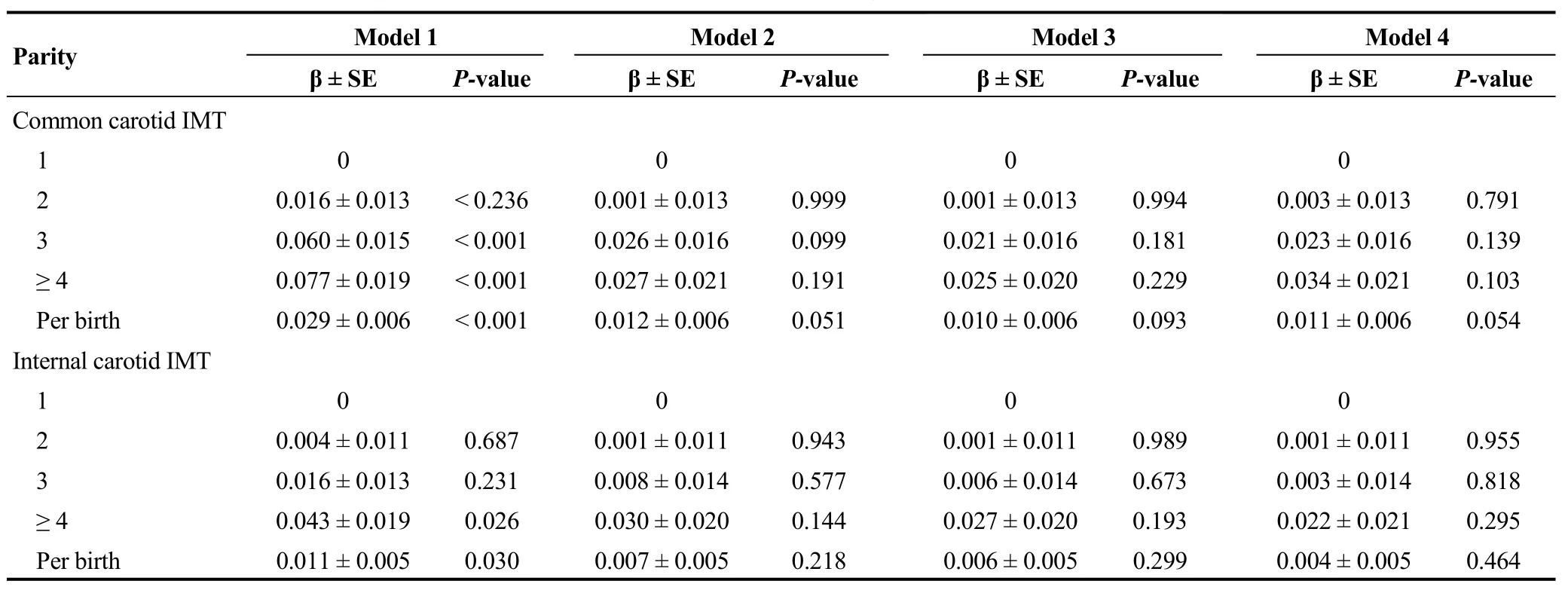
Table 3.Association between parity and carotid artery IMT in linear regression models.
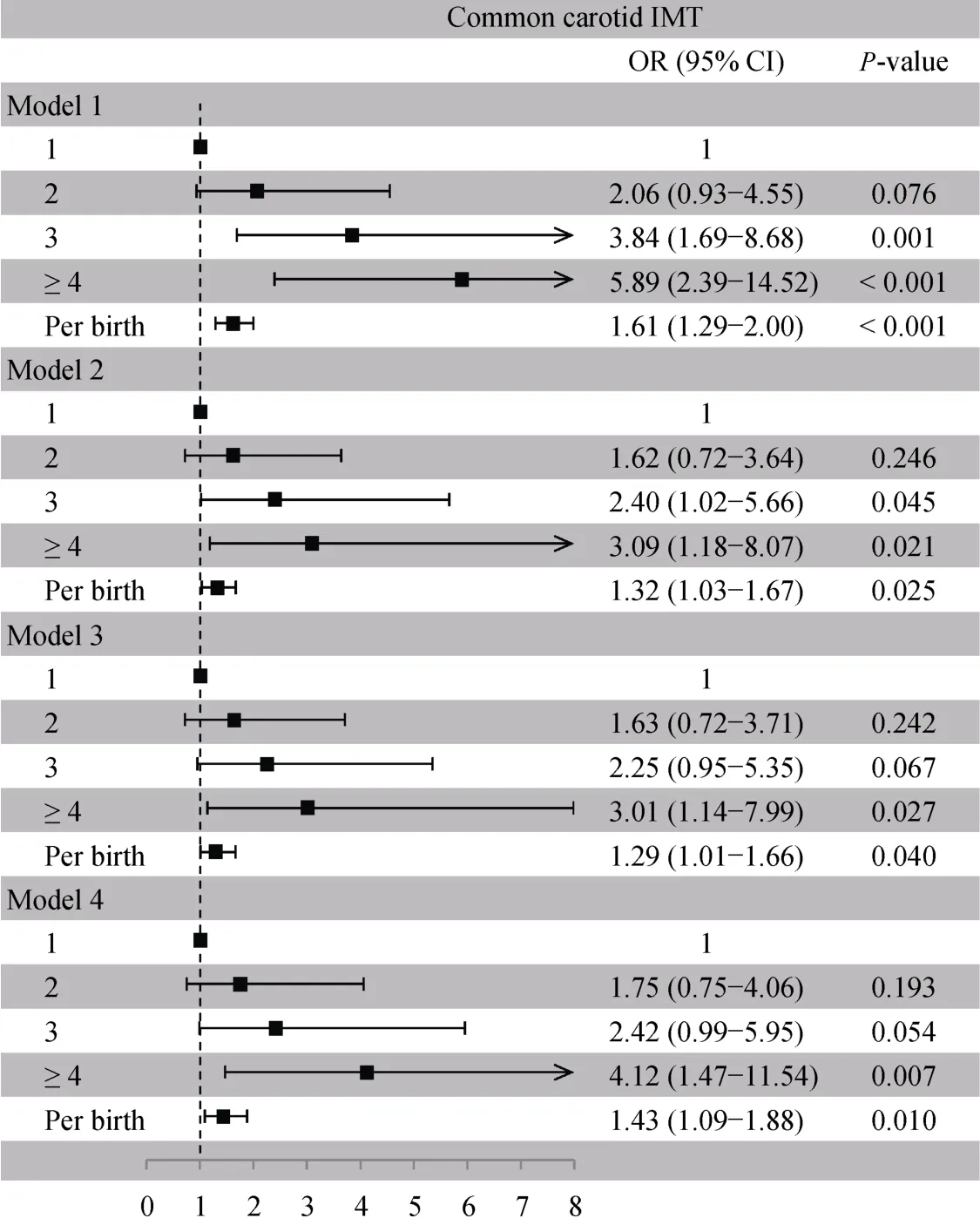
Figure 2.Association between parity and common carotid IMT obvious thickening.Model 1: unadjusted.Model 2: adjusted for age.Model 3: adjusted for age, hypertension, diabetes mellitus and dyslipidemia.Model 4: adjusted for age, hypertension, diabetes mellitus,dyslipidemia, education level, income, current smoking, body mass index, physical activity, antihypertensive medication, insulin or oral hypoglycemic drug, antilipemic agent and oral contraceptives.IMT: intima-media thickness.
Interestingly, when common carotid IMT was classified into two subgroups, including IMT ≥ 1 mm as an obvious thickening and IMT < 1 mm as normal (Figure 2), it seemed that higher parity was associated with more obvious thickening in the unadjusted model (OR = 1.61, 95% CI: 1.29–2.00,P< 0.001).In the fully adjusted model, this association remained statistically significant (OR = 1.43, 95% CI:1.09–1.88,P= 0.01).
4 Discussion
We first assessed the association between parity and carotid atherosclerosis in elderly Chinese women.We found that women with more birth had an increased risk of carotid plaques.In addition, there was a positive association between parity and risk of obvious thickening for common carotid IMT.However, no significant associations were observed between parity and common carotid IMT or between parity and internal carotid IMT.
Previous studies reported inconsistent relationships between parity and carotid atherosclerosis.The Rotterdam Study first found a progressive increase between parity and risk of carotid artery plaques in Dutch women aged ≥ 55 years.[1]In French women aged > 45 years, a linear association was observed between women with more birth and the prevalence of carotid plaques.[6]In women aged 45–79 years in the northeast Germany, there was a U-shaped association between parity and mean, as well as maximum,common carotid IMT.[2]Sanghavi,et al.[7]also reported a U-shaped relationship between parity and the risk of subclinical coronary and aortic atherosclerosis in U.S.women aged 30–65 years.In British women aged 60–79 years, a J-shaped association was prospectively found between parity and the risk of coronary heart disease.[3]However, both in Finnish women aged 45–74 years and in southern German women aged 50–81 years, parity was not significantlyassociated with carotid plaques or IMT.[4,5]In our study, we found a positive association between parity and carotid artery plaques.Women with more birth tended to have a higher risk of carotid artery plaques compared to those who had only one birth.Besides, higher parity was associated with more obvious thickening in common carotid IMT.Our results were similar to the findings in Dutch women aged ≥55 years.
Several reasons should be considered in explaining the discrepancies between these findings.Firstly, women of different age groups were included.Some studies only included elderly women,[3]while others included both middle-aged and older women,[1,2,4–6]and yet other studies enrolled individuals younger than 30 years.[7]In our study, we only included those over 60 years old.The differences in age might cause an unavoidable bias in the results.Secondly, the study populations were from different countries with different races and sociodemographic characteristics, which might cause heterogeneity in the associations.[16]Last but not least, among the Dutch participants, 21.5% were nulliparous;[1]whereas the proportion was 8.5% and 18% in the cohorts from Germany and France,[2,6]respectively.In our population, we excluded the nulliparous women due to small sample size.
Previous studies proposed possible biological mechanisms behind the association between parity and atherosclerosis.Firstly, sex hormones are modified during pregnancy, resulting in relatively lower protection by estrogen.[17]Reduced exposure to estrogen may promote the development of maternal atherosclerosis.[18]Secondly, repeated pregnancies may lead to chronic metabolic alterations, such as increases in lipid profile, insulin resistance, dysglycemia,obesity, folate deficiency,etc.[19]All of these changes might contribute to the pathophysiological processes of atherosclerotic diseases.Last but not least, pregnancy is associated with changes in endothelial function, the coagulation system,oxidative stress, and inflammation response, which cause direct harmful effects on the cardiovascular system.[20]
4.1 Limitations
Several limitations of our study should also be considered.First of all, the study population consisted of elderly women from China, who have specific sociodemographic characteristics.Thus, the results might be restricted in their generalizability to other countries.Moreover, reproductive factors, including miscarriage, abortions, stillbirths, and breastfeeding, were not assessed in the present study.In addition, the questionnaire did not include information on pre-eclampsia, gestational hypertension, or gestational diabetes mellitus.The exclusion of these pregnancy complications could potentially lead to an overestimation of the observed association.
4.2 Conclusions
In conclusion, we found a positive association between parity and risk of carotid plaques, as well as parity and risk of obvious thickening for common carotid IMT in elderly Chinese women, suggesting multiparous women might be exposed to a greater atherosclerotic burden.Particular attention should be paid to parous women, especially multiparous individuals.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (No.81870303).All authors had no conflicts of interest to disclose.The authors gratefully acknowledge the all enrolled participants and their family members.
 Journal of Geriatric Cardiology2020年12期
Journal of Geriatric Cardiology2020年12期
- Journal of Geriatric Cardiology的其它文章
- Wild type transthyretin amyloidosis, a reason not to be forgotten for heart failure of preserved ejection fraction in the elderly
- Guiding extension catheter facilitated percutaneous coronary intervention for a dextrocardia patient with acute left anterior descending artery occlusion: a case report
- A nonagenarian patient with rhabdomyolysis and multiple organ dysfunction:a case report
- Can sacubitril/valsartan become the promising drug to delay the progression of chronic kidney disease?
- Venous thromboembolism prophylaxis-prescribing patterns among elderly medical patients in a Saudi tertiary care center: success or failure?
- Validation of methods for effective orifice area measurement of prosthetic valves by two-dimensional and Doppler echocardiography following transcatheter self-expanding aortic valve implantation
