Validation of methods for effective orifice area measurement of prosthetic valves by two-dimensional and Doppler echocardiography following transcatheter self-expanding aortic valve implantation
Ming-Hu XIAO, Yong-Jian WU, Jing-Jin WANG, Guang-Yuan SONG, Jian-De WANG, Zhen-Hui ZHU,Xu WANG, Zhen-Yan ZHAO, Hao WANG,#
1Department of Echocardiography, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
2Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
3Department of Surgery, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Abstract Background The effective orifice area (EOA) is utilized to characterize the hemodynamic performance of the transcatheter heart valve (THV).However, there is no consensus on EOA measurement of self-expanding THV.We aimed to compare two echocardiographic methods for EOA measurement following transcatheter self-expanding aortic valve implantation.Methods EOA was calculated according to the continuity equation.Two methods were constructed.In Method 1 and Method 2, the left ventricular outflow tract diameter (LVOTd)was measured at the entry of the prosthesis (from trailing-to-leading edge) and proximal to the prosthetic valve leaflets (from trailing-toleading edge), respectively.The velocity-time integral (VTI) of the LVOT (VTILVOT) was recorded by pulsed-wave Doppler (PW) from apical windows.The region of the PW sampling should match that of the LVOTd measurement with precise localization.The mean transvalvular pressure gradient (MG) and VTI of THV was measured by Continuous wave Doppler.Results A total of 113 consecutive patients were recruited.The mean age was 77.2 ± 5.5 years, and 72 patients (63.7%) were male.EOA1 with the use of Method 1 was larger than EOA2(1.56 ± 0.39 cm2 vs. 1.48 ± 0.41 cm2, P = 0.001).MG correlated better with the indexed EOA1 (EOAI1) (r = -0.701, P < 0.001) than EOAI2(r = -0.645, P < 0.001).According to EOAI (EOAI ≤ 0.65 cm2/m2, respectively), the proportion of sever prosthesis-patient mismatch with the use of EOA1 was lower than EOA2 (12.4% vs. 21.2%, P < 0.05).Compared with EOA2, EOA1 had lower interobserver and intra-observer variability (intra: 0.5% ± 17% vs. 3.8% ± 22%, P < 0.001; inter: 1.0% ± 9% vs. 3.5% ± 11%, P < 0.001).Conclusions For transcatheter self-expanding valve EOA measurement, LVOTd should be measured in the entry of the prosthesis stent (from trailing-to-leading edge), and VTILVOT should match that of the LVOTd measurement with precise localization.
Keywords: Aortic valve stenosis; Echocardiography; Transcatheter aortic valve implantation
1 Introduction
Transcatheter aortic valve implantation (TAVI) has emerged as an alternative to standard surgical aortic valve replacement in high-risk patients with severe aortic stenosis.Five-year results in real-world, elderly, high-risk patients undergoing TAVI with a self-expanding bio-prosthesis provided evidence for continued valve durability with low rates of reinterventions and hemodynamic valve dysfunction.[1–4]
The effective orifice area (EOA) (estimated by the continuity equation), which provides complementary information, is one of the main echocardiographic indexes utilized to characterize the hemodynamic performance of prosthetic valves and identify the presence of prosthesis-patient mismatch (PPM).[2,5]Calculating EOA after TAVI relies on geometric measurement of the left ventricular outflow tract(LVOT) and the velocity-time integral (VTI) of the LVOT(VTILVOT) in addition to Continuous wave Doppler (CW)imaging of the transcatheter heart valve (THV).There islittle controversy regarding how to measure the VTI of the THV (VTITHV).However, the optimal site for placement of the sample volume to obtain VTILVOTafter TAVI is less well established.Moreover, for transcatheter self-expanding valves, there is no consensus about the optimal site for LVOT measurement.With regard for where to measure the LVOT diameter (LVOTd), initial studies of the selfexpanding valve suggested that the LVOTd should be measured just below the hinge points of the visible prosthetic leaflets.[6]However, recent trials have used the ventricular edge of THV;[1,7]in other words, in the entry of the stent.A comparison and validation of previously described methods for calculating the EOA for the self-expanding THV is lacking.
The objective of this study was to compare the methods used in previous studies to measure the EOA of the selfexpanding THV following TAVI and validate an optimal method using transthoracic two-dimensional echocardiography and Doppler assessment.
2 Methods
The protocol of this study was approved by the Ethics Committee of Fuwai Hospital (No.2012-415), and all the patients gave informed consent in accordance with the Helsinki Declaration of 1975 and later revisions.Informed consent was obtained from all patients for being included in the study.
2.1 Study population
A total of 121 consecutive patients were included in this study.All patients were diagnosed with symptomatic severe aortic stenosis who underwent TAVI with Venusmedtech-VenusA valve (Figure 1) (Venusmedtech, Hangzhou, China)at Fuwai Hospital.All patients were in outpatient follow-up at our center.Transthoracic echocardiography (TTE) data were collected before the procedure and 12 months after the procedure.Exclusion criteria included valve-in-valve TAVI(n= 3), patients who could not complete 12 months followup for various reasons (n= 5): two patients died for all causes and three patients could not complete follow-up at our center.Finally, a total of 113 patients were included in this study.
The THV was implanted based on computer tomography measurements of the aortic valve annulus.Venusmedtech-VenusA valves with a diameter of 23 mm, 26 mm, 29 mm and 32 mm were used for annulus sizes ranging from 17 to 20 mm, 20 to 23 mm, 23 to 26 mm and 26 to 29 mm, respectively.All clinical, echocardiographic, preoperative and postoperative data were prospectively collected.

Figure 1.The VenusA transcatheter artery valve produced by VenusMedtech is a self-expanding valve device that has been approved by the China Food and Drug Administration(Registration Number: 20173460680) and officially listed in China.
2.2 Echocardiography
TTE was performed using a commercially available system (E9 ultrasound system, GE Healthcare, Horten, Norway).Standard two-dimensional and Doppler echocardiographic images were acquired using a phased-array transducer in the parasternal and apical views and stored digitally for offline analysis using EchoPAC software version BT 113 (GE Healthcare, Horten, Norway).Each echocardiographic measurement was averaged from three consecutive cardiac cycles for patients in sinus rhythm and from five consecutive cycles in patients with atrial fibrillation.All measurements were performed according to the recommendations of the American Society of Echocardiography.[8]
2.2.1 Continuity equation for aortic valve effective orifice
The EOA for THV was calculated according to the continuity equation as (LVOTd)2× 0.785 × (VTILVOT/VTITHV).[9]The indexed EOA (EOAI) was calculated as EOA/body surface area (BSA).
LVOTd was measured from a zoomed parasternal long-axis acquisition.Two methods were constructed (Figure 2).In Method 1, LVOTd1was measured at the entry of the prosthesis stent and from the trailing to the leading edge of the stent, whereas in Method 2, LVOTd2was measured proximal to the prosthetic valve leaflets (0.5 to 1.0 cm below the aortic valve annulus) and from the trailing-to-leading edge.
VTITHVwas mainly measured by CW from apical windows or occasionally from other acoustic windows (e.g., the right parasternal or suprasternal) to obtain the highest VTITHV,meanwhile, got the mean transvalvular pressure gradient(MG).VTILVOTwas recorded by pulsed-wave Doppler (PW)from apical windows.The region of the PW sampling should match that of the LVOTd measurement with precise localization.
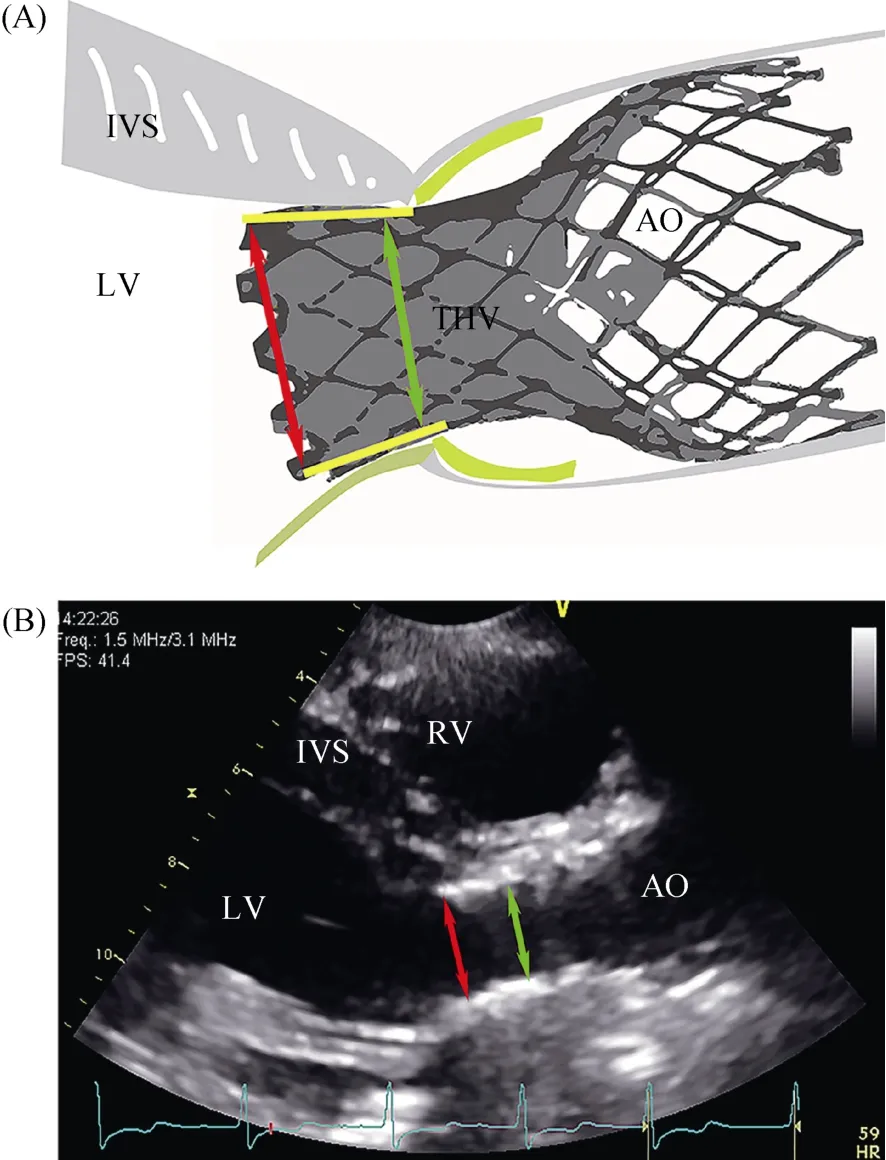
Figure 2.Measurement of the LVOTd.A zoomed LVOT in parasternal long-axis view.Schematic drawing of LVOTd measurements (A) and representative image of two-dimensional echocardiography (B).In Method 1, LVOTd was measured at the entry of the prosthesis stent from the trailing-to-leading edge of the stent (inner to inner edge, red arrow).In Method 2,measurements were obtained proximal to the prosthetic valve leaflets (0.5 to 1.0 cm below the aortic valve annulus) from the trailing-to-leading edge (inner to inner edge, green arrow).AO: ascending aorta; IVS: interventricular septum; LV: left ventricle;LVOT: left ventricular outflow tract; LVOTd: left ventricular outflow tract diameter; RV: right ventricle; THV: transcatheter heart valve.
Due to the LVOT’s elliptical geometry, the LVOTd was measured in the 5-chamber view again (the parasternal long axis view and 5-chamber view are two planes lying perpendicular to each other).The minimal diameter and maximal diameter were defined as the shorter LVOTd and the longer LVOTd, respectively.The circularity of the basal plane was expressed as the eccentricity index [EI = 1 – (minimal diameter/maximal diameter)].[8]
2.2.2 Relationships between EOAIs and MG
The relationships between the EOAIs and the MG were evaluated to validate the measurements of EOA obtained by Method 1 and Method 2.
In low flow-state conditions, the MG may be pseudonormalized, and the EOA may be pseudo-severized, which may alter the relationship between the EOAI and the MG.[10]Taking into account of the stroke volume (SV) could be quantitated with either PW at the LVOT site or with a volumetric approach.In our study, for Method 1 and Method 2,the different LVOTd measurement got different SV.So, SV was measured with the volumetric approach: left ventricular end-diastolic volume minus end-systolic volume (evaluated via the biplane Simpson method).It was indexed for BSA[SV index (SVI)].We grouped patients by SVI as follows:Group 1 (n= 57): SVI ≥ 35 mL/m2and Group 2 (n= 56):SVI < 35 mL/m2, and we performed a sub-analysis of the Doppler echocardiographic data.
Depth of THV placement in LVOT was also studied.The depth of delivery was defined as the distance from the native aortic annular margin on the side of the noncoronary cusp (leftward on the described projection) to on the corresponding side the most proximal edge (deepest in the left ventricle) of the deployed stent-frame.This was measured using two-dimensional TTE.
2.3 Definition of PPM
Moderate and severe PPM were defined as EOAI ≤0.85 cm2/m2and ≤ 0.65 cm2/m2, respectively.[4]
2.4 Intra-observer and interobserver measurement variability
Twenty-six patients were randomly selected, and EOA measurements were repeated in these patients by two independent observers.Intra-observer and interobserver variability in the measurements were calculated.
2.5 Statistical analysis
Data are expressed as mean ± SD or number of patients(%).Changes in echocardiographic variables during postoperative follow-up were analyzed with the use of a one-way ANOVA for repeated measures followed by a Tukey Post Hoc test compared using the one-way analysis of variance (ANOVA).And Pearson’s chi-square test was used with two-tailedP-value to compare categorical variables.Relationships between EOAIs and MG were assessed with multiple nonlinear regression models, and the equation providing the best fit was retained.The results for intra-observer and interobserver variability between methods of measurement were assessed using the Bland-Altman methods.[11]All statistical analysis was performed with SPSS Statistics version 20.0 software for Windows (SPSS Inc., Chicago, IL,USA).A two-sidedP-value < 0.05 was considered statistically significant.
3 Results
3.1 Baseline characteristics
Finally, 113 patients were recruited in the study.The mean age was 77.2 ± 5.5 years, and 72 patients (63.7%)were male.The baseline characteristics are presented in Table 1.The mean follow-up days were 355 ± 13 days.A total of 33 patients (29.2%) received a 23-mm valve, 50 patients (44.2%) received a 26-mm valve, and 30 patients(26.6%) received a 29-mm valve.

Table 1.Baseline clinical characteristics.
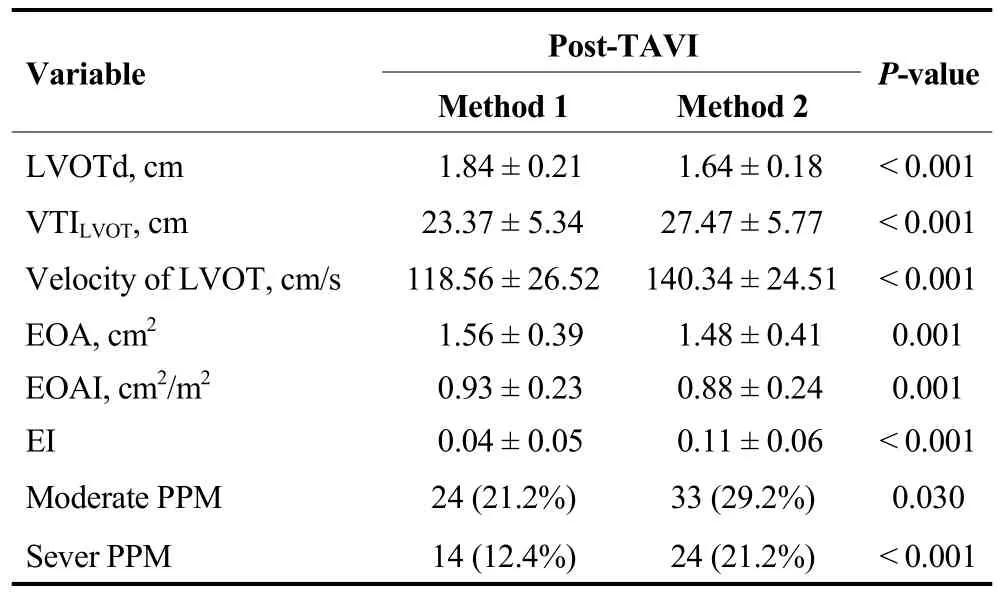
Table 2.Follow-up Doppler echocardiographic data in the whole cohort, grouped by different methods.
3.2 Follow-up Doppler echocardiographic data
The results of follow-up echocardiography assessments after TAVI are presented in Table 2.EOA1was significantly larger than EOA2(1.56 ± 0.39 cm2vs.1.48 ± 0.41 cm2,P=0.001).LVOTd1was larger than LVOTd2.The peak velocity at level 2 was significantly higher than the peak velocity at level 1.The LVOT was less elliptical in the entry of the THV stent than proximal to the prosthetic valve leaflets.According to EOAIs, the proportion of moderate and sever PPM with the use of EOA1was lower than EOA2(21.2%and 12.4%vs.29.2% and 21.2%, eachP< 0.05).Mean depth of THV in LVOT in the whole cohort was 11.62 ±3.78 mm.63 patients (55.7%) had the ‘optimal’ placement of the THV (5–10 mm below the native non-coronary cusp).50 patients (44.3%) had the ‘suboptimal’ placement [48 patients (42.5%) > 10 mm, and 2 patients (1.8%) < 5 mm].
3.3 Normal flow-state condition and low flow-state condition
In the subgroups, LVOTd1, LVOTd2, VTILVOT, VTITHV,EOA1, EOAI1, MG and left ventricular end-diastolic diameter were larger in Group 1 than in Group 2 (Table 3).
3.4 Relationships between EOAIs and MG
MG correlated better with EOAI1than with EOAI2in the whole cohort (Figure 3A & 3B:r= -0.645 andr= -0.602,P< 0.001), in Group 1 (SVI ≥ 35 mL/m2) (Figure 3C & 3D:r= -0.701 andr= -0.645,P< 0.001) and in Group 2 (SVI< 35 mL/m2) (Figure 3E & 3F:r= -0.696 andr= -0.515,P< 0.001).

Table 3.Follow-up Doppler echocardiographic data in the subgroups (Group 1 with SVI ≥ 35 mL/m2 and Group 2 with SVI <35 mL/m2).
3.5 Intra-observer and interobserver variability
A Bland-Altman plot comparing the values of EOA1versus EOA2is shown in Figure 4.Compared with EOA2,EOA1had lower interobserver and intra-observer variability(intra: 0.5% ± 17%vs.3.8% ± 22%,P< 0.001; inter: 1.0%± 9%vs.3.5% ± 11%,P< 0.001).
4 Discussion
To the best of our knowledge, this study is the first to validate the methods used for calculating the EOA of the self-expanding THV by two-dimensional and Doppler echocardiography.Our results confirm that Method 1 was better than Method 2; in other words, it is preferable to measure LVOTd in the entry of the stent and from the trailing-to-leading edge, while the optimal site for placement of the sample volume to obtain VTILVOTwas in the entry of the stent.
As a functional determination of prosthesis size,in vivoEOA can vary widely, depending on a number of factors related to the measurement technique used and the patient state.Variability can be introduced during the measurement of LVOTd or VTILVOT.[12,13]
For a self-expanding valve, there is no consensus regarding the optimal site for measuring LVOTd on TTE.[14]In the 2009 American Society of Echocardiography guidelines for echocardiographic assessment of prosthetic valve function,it is recommended that LVOTd should be measured just beneath the prosthesis sewing ring.[15]However, this method can serve as a general rule for all types of prosthetic aortic values.In the 2019 American Society of Echocardiographyguidelines for the evaluation of valvular regurgitation after percutaneous valve replacement, it is recommended that LVOTd should be measured using different method in different situations: (1) when a self-expanding valve is placed low in the left ventricular, particularly if the lower end of the stent is not in close proximity to the anterior mitral leaflet and interventricular septum, LVOTd is to measure the inner edge-to-inner edge diameter of the valve stent immediately proximal to the cusps; and (2) when a self-expanding valve is placed just beneath the aortic annulus, and thelower end of the stent is close proximity to the anterior mitral leaflet and interventricular septum, it is recommended that LVOTd should be measured using the outer edge-to-outer edge diameter at the lower (ventricular) end of the valve stent for a self-expanding valve.[16]In Jilaihawi’s study,[6]the average depth of implantation was 10.5 ± 3.4 mm,which was similar with our data.In our study, for most patients (111, 98%), the depth of THV placement in LVOT were more than 5 mm and the lower end of the stent is not in close proximity to the anterior mitral leaflet and interventricular septum.Hence, in our study, LVOTd was measured from the trailing-to-leading edge (inner edge-to-inner edge diameter of the valve stent).

Figure 3.Correlation between MG and EOAI.MG correlated better with EOAI1 than with EOAI2 in the whole cohort (A & B), in Group 1 (SVI ≥ 35 mL/m2) (C & D) and in Group 2 (SVI < 35 mL/m2) (E & F).EOAI: indexed effective orifice area; MG: mean transvalvular pressure gradient; SVI: stroke volume index.

Figure 4.Bland-Altman plots comparing the interobserver and intra-observer variability in measurements of the prosthetic self-expanding valve EOA when using different methods.EOA1 (blue dots) versus EOA2 (green dots): interobserver (A) and intra-observer (B) variability.EOA: effective orifice area.
For transcatheter balloon expandable valves, Clavel,et al.[17]recommended measuring LVOTd immediately proximal to the stent.Compared Clavel’s Method 2 with our Method 1,the first difference is that a self-expanding valve was employed; and the second difference is that in Clavel’s Method 2, LVOTd was measured outside the stent and from outerto-outer.[17]For balloon expandable valves, the depth of THV placement in LVOT was less than the self-expanding valve,and the lower end of the stent is close proximity to the anterior mitral leaflet and interventricular septum.Previous studies of the self-expanding valve suggested that LVOTd should be taken just below the hinge points of the visible prosthetic leaflets, measuring the inner-to-inner stent,[6]which was similar to our Method 2.
In our study, two methods were constructed: Method 1:LVOTd and VTILVOTwere measured in the entry of the prosthesis stent, and Method 2: LVOTd and VTILVOTwere measured proximal to the visible prosthetic leaflets.For the methods in which we calculated the LVOTd of the selfexpanding THV using the outer edge to outer edge diameter,the confused borders of the stent may have contributed to the variance observed in the measurement of LVOTd,which represents an external dimension of the prosthesis and not its internal orifice.Especially for patients with poor image quality.Therefore, we did not validate the methods used to calculate the LVOTd using the outer-to-outer edge.The correlation between EOAI and MG has been previously reported to be highly predictive of adverse outcomes.[12]Our study shows that MG correlated better with EOAI1than EOAI2in the whole cohort and in the both subgroups (with SVI ≥ 35 mL/m2and SVI < 35 mL/m2).Intra-observer and interobserver variability were lower for Method 1 than Method 2.These results suggest that Method 1 provides a more accurate and reliable estimate of EOA for transcatheter self-expanding valves.Possible reasons for the higher variability observed when using Method 2 include the following:(1) it was difficult to precisely identify the base of the prosthetic cusps due to acoustic shadowing created by the prosthesis stent and the calcification of the native aortic valve and annulus; (2) the shape of the LVOT is more elliptical at this level; and (3) there is significant flow acceleration within the stent proximal to the prosthetic leaflets.
In view of the special structure of transcatheter selfexpanding valves, they have a longer left-ventricular stent.Although the THV is designed for circular deployment, the THV device landing zone often has a non-circular shape,and the LVOT’s geometry is more circular at the entry ofthe prosthesis stent than at the level proximal to the prosthetic valve leaflets.[18]In our study, the EI of the LVOT was smaller in the entry of the prosthesis stent than at the level proximal to the prosthetic valve leaflets.The more elliptical shape of the LVOT may result in significant underestimations of true cross-sectional areas.Then, there was significant flow acceleration at the level within the stent that was proximal to the prosthetic leaflets (left ventricular side).[19]In our study, the peak velocity of the LVOT when calculated proximal to the leaflets was significantly higher than the velocity measured in the entry of the stent, resulting in an overestimated EOA.The flow acceleration proximal to the leaflets is mostly related to the elliptical shape of the LVOT and the turbulent flow at this level.[20]In both Clavel’s Method 2 and our Method 1, the flow acceleration within the stent proximal to the prosthetic leaflets was avoided.[17]However, in some studies, flow acceleration is ignored, resulting in a larger EOA (1.7 ± 0.5 cm2; e.g., in Jilaihawi’s study).[6]When we compared our Method 1 and Method 2, although VTILVOTwas higher when using Method 2 (because of the geometry of the LVOT was more elliptical at this level and the flow acceleration proximal to the cusps), but LVOTd2was much smaller than LVOTd1,resulting in a smaller EOA2.
In the present study, patients with self-expandable prosthesis provided an excellent hemodynamic performance and the incidence of severe PPM was low.Incidence of moderate and severe PPM estimated with the use of indexed EOAI1was similar with the previous studies, reported by Jilaihawi,et al.[6](moderate: 32%, severe: 2%), Tzikas,et al.[21](moderate: 23%, severe: 16%) and Muñoz-García,et al.[22](moderate: 34.9%, severe: 9%) for the CoreValve prosthesis.Our LVOTd of severe PPM group was smaller than Muñoz-García’s LVOTd.[22]These differences can be partially explained by the design, size of different prostheses and different methods for EOA measurement.Jilaihawi,et al.[6]reported a low incidence of severe PPM.Firstly, different prosthesis was employed in our study.Secondly, Jilaihawi’s EOA (1.7 ±0.5 cm2) was larger than our EOA1, flow acceleration at the level (just below hinge points of visible prosthetic leaflets)may exist.
4.1 Limitations
The most obvious limitation of our study was the absence of an accepted gold standard for EOA measurement.Because a transcatheter self-expanding valve was employed in this study, the results of this study may not be applicable to transcatheter balloon expandable valves.With regard for the EI, the LVOTd was measured in a 5-chamber view or parasternal long axis view, and the minimal diameter and maximal diameter may therefore not be accurate.No threedimensional imaging was used.Our study was a singlecentre study that included a relatively small number of patients.Further studies that include a larger number of patients and longer follow-up are needed to establish the normal reference values of the valve hemodynamic parameters of transcatheter valves and determine whether their hemodynamic performance is maintained in the long term.
4.2 Conclusions
In conclusions, for transcatheter self-expanding valves,measuring LVOTd at the entry and from the trailing-toleading edge of the stent is likely more appropriate than other methods for the estimation of EOA by transthoracic Doppler echocardiography.Moreover, the PW sample should be located in the entry of the stent and on the same horizontal line used to measure the LVOTd.
Acknowledgments
All authors had no conflicts of interest to disclose.The authors gratefully acknowledge Xin YUAN for revising the manuscript for language and statistical analysis.
 Journal of Geriatric Cardiology2020年12期
Journal of Geriatric Cardiology2020年12期
- Journal of Geriatric Cardiology的其它文章
- Advances in Journal of Geriatric Cardiology over the course of a decade
- Catheter ablation for atrial fibrillation is associated with reduced risk of mortality in the elderly: a prospective cohort study and propensity score analysis
- Effects of angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker on one-year outcomes of patients with atrial fibrillation: insights from a multicenter registry study in China
- Parity and carotid atherosclerosis in elderly Chinese women
- Venous thromboembolism prophylaxis-prescribing patterns among elderly medical patients in a Saudi tertiary care center: success or failure?
- Can sacubitril/valsartan become the promising drug to delay the progression of chronic kidney disease?
