Efficacy evaluation of acupuncture plus rehabilitation training for post-stroke deglutition disorders of qi-deficiency blood stasis pattern
Huang Yi-qing (黄逸清),Ma Wen (马文),Shen Wei-dong (沈卫东)
1Shuguang Hospital,Shanghai University of Traditional ChineseMedicine,Shanghai201203,China
2 Shanghai Yangpu Hospital of Traditional Chinese Medicine,Shanghai 200090,China
Abstract
Keywords:Acupuncture Therapy;Stroke Rehabilitation;Qi-deficiency Blood Stasis;Poststroke Syndrome;Pseudobulbar Palsy; Deglutition Disorders
With the aging of human society, the incidence of stroke has been rising. At the global scaleOn a global scale,China has the highest incidence of stroke and bears the most significant burden for it[1]. Deglutition disorder, one of the most common complications after stroke,has an incidence rate of 14%-71%[2-3].Post-stroke deglutition disorder may increase the death and disable disability rate since it can cause various complications such as aspiration pneumonia, nutritional disorders and dehydration[4].
Traditional Chinese medicine (TCM) has a long history in treating post-stroke deglutition disorder.Chinese medicationmedicine, acupuncture and bloodletting all can produce certain efficacy in treatment of this medical condition[5]. Qi-deficiency blood stasis has been considered a common cause of stroke[6-8]. TCM holds that when qi fails to circulate blood,blood becomes stagnant; and then the stagnant blood may enter the brain along the blood vessels to block the meridians and cause ischem ia and hypoxia, leading to stroke.
This study was to observe the clinical efficacy of acupuncture plus rehabilitation in treating post-stroke deglutition disorder of qi-deficiency blood stasis pattern.The report is given as follows.
1 Clinical Materials
1.1 Diagnostic and pattern-differentiation criteria
1.1.1 Diagnostic criteria for cerebral infarction in Westernmedicine
By referring the diagnostic criteria for cerebral infarction in theChina Guideline for Cerebrovascular Disease Prevention and Treatment(2005)[9].
1.1.2 Diagnostic criteria for cerebral hemorrhage in Westernmedicine
By referring the diagnostic criteria for cerebral hemorrhage in theChina Guideline for Cerebrovascular Disease Prevention and Treatment(2005)[10].
1.1.3 Diagnostic criteria for stroke of qi-deficiency blood stasispattern in TCM
Based on the pattern-differentiation criteria in theCriterion of Diagnosis and Therapeutic Effect of Apoplexy[11].
1.1.4 Diagnostic criteria for post-stroke deglutition disorder
By referring the diagnostic criteria in the
Management of Patients w ith Stroke Ⅲ:Identificationand Management of Dysphagia[12].
1.2 Inclusion criteria
Met the above diagnostic criteria and pattern- differentiation criteria; aged 40-85 years old; graded 3-5 by Kubota water swallow ing test (KWST) or scored 3-7 points by Fujishima Ichiro food intake level scale (FILS);w ith clear consciousness and good compliance,and able to follow the instructions during exam inations and treatments;informed consent form signed by the patient or his/her fam ily.
1.3 Exclusion criteria
Coupled w ith severe respiratory,circulatory or hemotologic diseases; other disorders affecting throat,such as thyroid diseases,topical infection or ulcers;serious mental or conscious disorders or dementia that can influence the patient's expression; receiving other treatments that may affect the outcome measure; w ith poor compliance and unable to cooperate the exam inations or treatments; women in pregnancy or lactation.
1.4 Statistical methods
1.5 General data
Patients who visited the Acupuncture-moxibustion Department,Neurology Department or Rehabilitation Department of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine,Shanghai Baoshan District Hospital of Integrated Chinese and Western Medicine and Shanghai Changning Tianshan Traditional Chinese Medicine Hospital between May 2018 and February 2019 and diagnosed w ith post-stroke deglutition disorder of qi-deficiency blood stasis pattern were recruited.A total of 66 participants were random ized into an observation group and a rehabilitation group by the random number table method, w ith 33 cases in each group. During the study,the two groups each had one dropout case due to not feeling significant improvement in the symptoms. In the end, 64 cases completed the intervention, w ith 32 cases in each group. There were no significant differences in the data of gender, age and disease duration between the two groups (allP>0.05), indicating the comparability (Table 1).
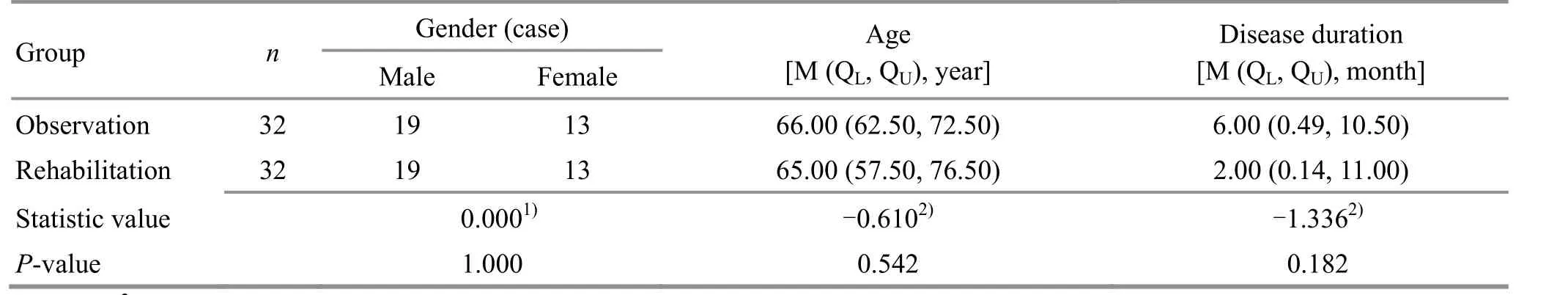
Table 1. Com parison of the baseline between the two groups
2 Treatment Methods
Same conventional medications and supportive treatment for stroke were given to the two groups.
2.1 Observation group
2.1.1 Acupuncture treatment
Acupoints: Baihui (GV 20), Fengchi (GB 20), Fengfu(GV 16),Yamen(GV 15),Yifeng (TE 17),Lianquan(CV 23), Jinjin (EX-HN 12), Yuye (EX-HN 13) and Zusanli(ST 36).
Method:ENERGY disposable sterile acupuncture needles of 0.25 mm in diameter and 40 mm in length were used for acupuncture treatment.After routine sterilization,Baihui(GV 20)was subcutaneously punctured for 0.5-1.0 cun with the needle tip backward;Fengchi (GB 20) was obliquely punctured for 0.8-1.2 cun w ith the needle tip towards the nose tip; Fengfu (GV 16)and Yamen (GV 15) were slow ly inserted for 0.5-1.0 cun w ith the needle tip towards the lower jaw; Yifeng (TE 17)was perpendicularly inserted for 0.5-0.8 cun; Lianquan(CV 23) was perpendicularly inserted with the needle tip towards the base of the tongue or the throat; Jinjin(EX-HN 12)and Yuye(EX-HN 13)were pricked for bloodletting;Zusanli(ST 36)was perpendicularly punctured for 1.0-1.5 cun. The needles were retained for 30 min except those at Jinjin (EX-HN 12) and Yuye(EX-HN 13). The acupuncture treatment was performed every other day, 3 times a week, for a total of 4 weeks.
2.1.2 Rehabilitation
Supraglottic swallow,Mendelsohn method,Shaker method, tongue exercise, and orofacial myofunctional exercises, cold stimulation to oral cavity and throat, and vocal cord closure exercise were adopted, 30 m in each session, once every other day, 3 times a week, for a total of 4 weeks,following the same treatment schedule as that of the acupuncture treatment.
其次,根据经济学理论,产权越明晰,对微观权益、绩效界定越清楚,越有利于提高整个经济系统的效率。对水资源而言,要改变吃国家“大锅水”的状况,明确水权的产权性质,把水的使用权明晰到基层用户,使水的利用效率与微观用户的经济利益紧密联系起来,以发挥整个社会爱惜水资源、节约水资源、保护水资源的积极性。
2.2 Rehabilitation group
The rehabilitation group received same rehabilitation measures, follow ing the same method and schedule as the observation group.
3 Therapeutic Efficacy Observation
3.1 Observation items
The two groups of patients were evaluated by the follow ing items at recruitment (before treatment), after 4-week treatment and 1 month after treatment.
3.1.1 Major observation items
KWST: Estimated by a 5-grade scale from grade 1 to grade 5.A higher level indicates worse swallowing function.
FILS:Scored 1-10 points and 10 points stands for normal swallowing function.A lower score indicates more serious swallow ing dysfunction.
3.1.2 Secondary observation items
TCM symptoms score: The grading and quantification standard referred the grading and quantification table for stroke symptoms in theGuiding Principles for Clinical Study of New Chinese Medicines[13], mainly involving the major symptoms such as consciousness,body movements,articulation and swallow,secondary symptoms, complications, tongue and pulse inspection.The maximum score was 111 points and the lowest was 0. A higher score suggests severer symptoms.
3.2 Criteria for therapeutic efficacy evaluation
3.2.1 Efficacy criteria for swallow ing function
Recovered: Grade 1 by KWST or 10 points by FILS,and swallowing dysfunction symptoms were gone.
Markedly effective: Increased by 2 or more grades by KWST or increased by 3 or more points by FILS, and the swallowing dysfunction symptoms were significantly improved.
Effective:Increased by <2 grades by KWST or increased by <3 points by FILS,and the swallow ing dysfunction symptoms showed certain improvement.
Invalid: Evaluated >grade 3 by KWST or <3 points by FILS,and there was no notable improvement in the swallowing dysfunction symptoms.
3.2.2 Efficacy criteria for TCM symptoms
The evaluation criteria for TCM symptoms in theGuiding Principles for Clinical Study of New ChineseMedicineswere employed[13],and the efficacy was evaluated by the reduction rate of the TCM symptoms score.
Symptoms score reduction rate= (Pre-treatment score - Post-treatment score)÷ Pre-treatment score×100%.
Recovered: Symptoms score reduction rate ≥95%.
Markedly effective: Symptoms score reduction rate≥70% but <95%.
Effective: Symptoms score reduction rate ≥30% but <70%.
Invalid: Symptoms score reduction rate ≥0 but <30%.
Aggravated(including death):Symptoms score reduction rate <0.
3.3 Results
3.3.1 Comparison of the efficacy for swallow ing function
At 1 month after treatment, the total effective rate was 93.8% in the observation group versus 75.0% in the rehabilitation group, and the between-group difference in the general efficacy was statistically significant (P<0.05), (Table 2).
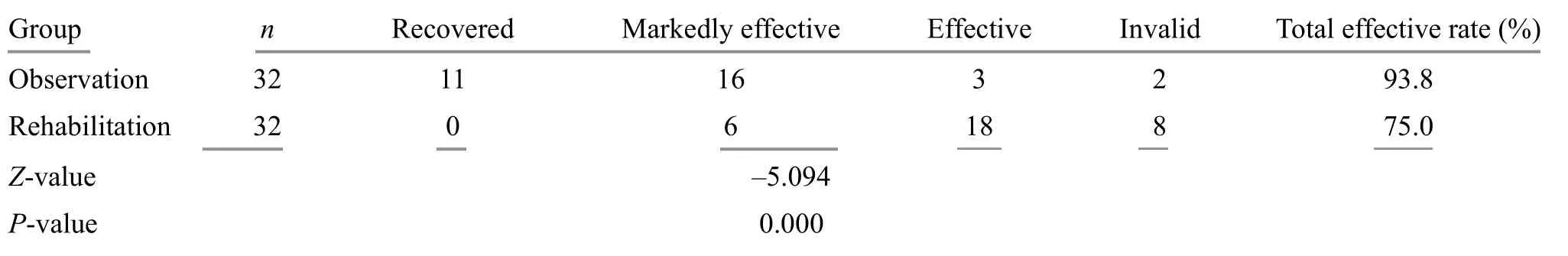
Table 2. Com parison of the efficacy for swallow ing function (case)
3.3.2Comparison of the KWST grading
There was no significant difference in the KWST grading between the two groups before treatment(P>0.05), (Table 3).
Intra-group comparison:Pairwise comparison was applied in comparing the KWST grading in the observation group at the three time points, i.e. before treatment,after treatment and at the follow-up.In comparing the KWST grading between before and after treatment,Z=-4.456,P<0.001;in comparing that between before treatment and at the follow-up,Z=-4.544,P<0.001;in comparing that between after treatment and at the follow-up,Z=-0.234,P=0.810. The pairwise comparison of the KWST grading in the rehabilitation group at the three time points showed that between before treatment and after treatment,Z=-2.599,P=0.009; between before treatment and at the follow-up,Z=-2.931,P=0.003;between after treatment and at the follow-up,Z=-0.322,P=0.747.
The between-group comparison showed that there were significant differences in the KWST grading between the two groups after treatment and at the follow-up (bothP<0.05), (Table 4-Table 5).
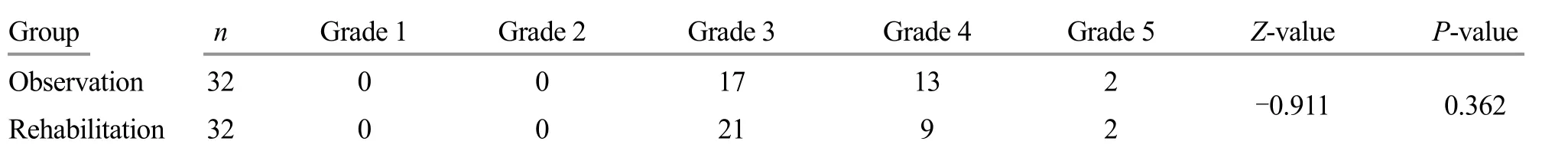
Table 3. Com parison of the KWST grading between the two groups before treatment (case)
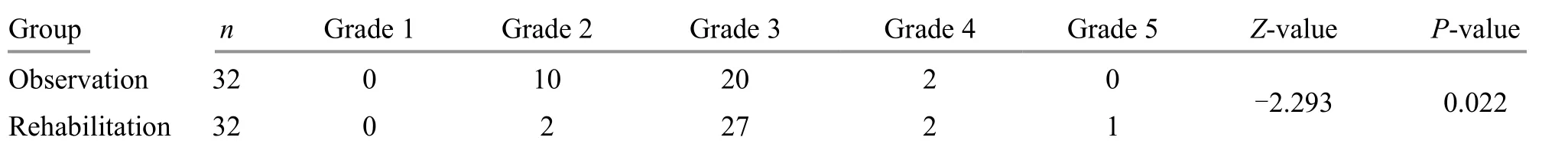
Table 4.Comparison of the KWST grading after 4-week treatment (case)

Table 5.Comparison of the KWST grading at the 1-month follow-up (case)
3.3.3 Comparison of the FILS score
There was no significant difference in the FILS score between the two groups before treatment (P>0.05),(Table 6).
Intra-group comparison: The pairw ise comparison of the FILS score in the observation group before treatment,after treatment and at the follow-up demonstrated that between before treatment and after treatment,Z=-5.785,P<0.001;between before treatment and at the follow-up,Z=-6.068,P<0.001;between after treatment and at the follow-up,Z=-0.762,P=0.446. The pairwise comparison of the FILS score in the rehabilitation group at the three time points showed that between before treatment and after treatment,Z=-3.994,P<0.001;between before treatment and at the follow-up,Z=-4.262,P<0.001;between after treatment and at the follow-up,Z=-0.616,P=0.538.
The between-group comparison showed that there were significant differences in the FILS score between the two groups after treatment and at the follow-up(bothP<0.05), (Table 7-Table 8).
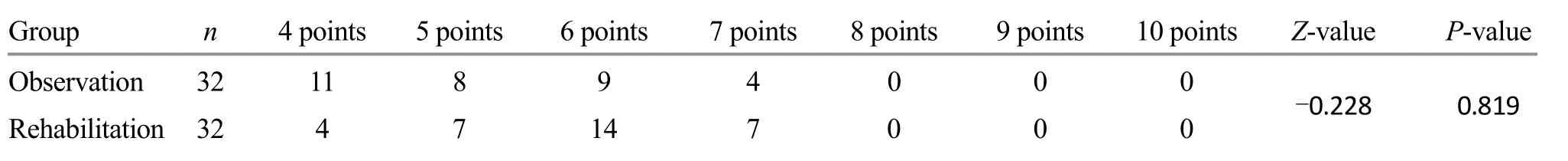
Table 6. Com parison of the FILS score before treatment (case)

Table 7.Comparison of the FILS score after 4-week treatment (case)
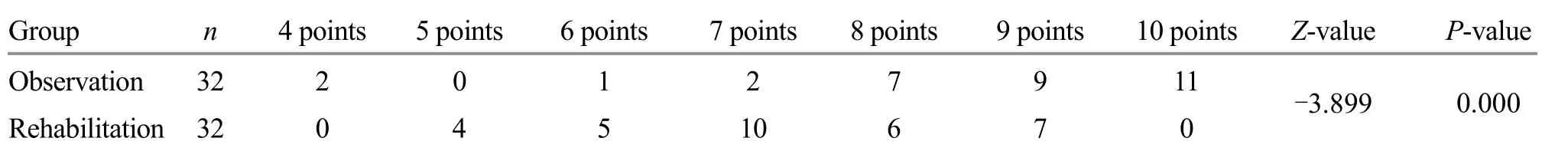
Table 8. Com parison of the FILS score at the 1-month follow-up (case)
3.3.4 Comparison of the TCM symptoms score
There was no significant difference in the TCM symptoms score between the two groups before treatment(P>0.05). The pairwise comparison of the TCM symptoms score in the observation group before treatment, after treatment and at the follow-up showed that between before and after treatment,Z=-4.942,P<0.001;between before treatment and at the follow-up,Z=-4.941,P<0.001; between after treatment and at the follow-up,Z=-4.714,P<0.001. The pairwise comparison of the TCM symptoms score in the rehabilitation group at the three time points demonstrated that between before and after treatment,Z=-4.969,P<0.001; between before treatment and at the follow-up,Z=-4.870,P<0.001;between after treatment and at the follow-up,Z=-3.911,P<0.001.There were no significant differences in the TCM symptoms score between the two groups after treatment and at the follow-up (bothP>0.05), (Table 9).
The efficacy for TCM symptoms score was compared between the two groups after treatment and at the follow-up. The intra-group comparison of the efficacy in the observation group between after treatment and the follow-up showedZ=-2.611,P=0.009. The intra-group comparison of the efficacy in the rehabilitation group between after treatment and at the follow-up showedZ=-0.320,P=0.749.The between-group comparison showed that there were significant differences in the efficacy for TCM symptoms score after treatment and at the follow-up (bothP<0.05), (Table 10-Table 11).

Table 9. Com parison of the TCM sym ptom s score [M (QL, QU), point]

Table 10.Com parison of the efficacy for TCM sym ptom s score after 4-week treatment (case)

Table 11. Com parison of the efficacy for TCM sym ptoms score at the 1-month follow-up(case)
4 Discussion
Post-stroke deglutition disorder can be classified into Hou Bi (throat Bi-impediment) or Yin Fei (aphasia and paralysis). This study targeted at the patients diagnosed w ith post-stroke deglutition disorder of qi-deficiency blood stasis pattern. The observation group was treated w ith acupuncture, at the acupoints on the nape, Baihui(GV 20) and Zusanli (ST 36), combined w ith bloodletting at Jinjin (EX-HN 12) and Yuye (EX-HN 13). Acupoints on the nape are close to the throat. Hence, acupuncture at the nape acupoints can stimulate the motor and sensory fibers in the throat region. When these stimuli are transmitted to the brain,it is beneficial to the reconstruction of the swallowing reflex and the recovery of the swallow ing function[14-16]. Bloodletting at Jinjin(EX-HN 12)and Yuye(EX-HN 13)has been commonly used for deglutition disorder[17-18]. It can not only activate the blood flow to unblock the stasis and accelerate the blood circulation in the glossopharyngeal region, but also open orifices to awaken the brain and boost the recovery of stroke, thus exerting therapeutic effects on both the root cause and superficial manifestations.Baihui(GV 20)is the joint of yang energy. Stimulating this acupoint can boost qi,blood and essence to go up to nourish the brain and glossopharyngeal region. Zusanli (ST 36) was selected as a distant acupoint,for arousing all meridians and collaterals to tonify qi and activate blood flow. These acupoints were used together to supplement qi and accelerate blood flow,and m itigate the qi-deficiency blood stasis state, so as to fundamentally improve the swallow ing function.
Currently, video fluoroscopic swallowing study (VFSS)is considered as the gold standard in evaluating the post-stroke swallow ing dysfunction[19-21].VFSS can determine the stage of the swallow ing dysfunction, if there is pulmonary aspiration and estimate its severity.Besides, fiberoptic endoscopic evaluation of swallowing (FEES) can be another option. However, high price and significant lim its have discouraged their application in clinic, and it is the questionnaires or scales that have been w idely adopted for clinical evaluation of deglutition disorder. KWST is a commonly used method since it can well reflect the patient's capability of swallowing fluid, but it is not reliable to use KWST in evaluating patients'capability of swallow ing other forms of food[22]. Therefore, this study adopted KWST,FILS and TCM symptoms score to conduct a comprehensive evaluation, to wholly study the patient's function when swallow ing different types of food.
In this trial, all the treatments were performed by professionals,the patients were peaceful when receiving treatments,and there were no adverse reactions such as passing out during acupuncture,hematoma and arrhythm ia, or complications such as aspiration pneumonia and malnutrition.
The KWST and FILS score changed significantly after treatment compared w ith the baseline figures in the two groups (allP<0.05), suggesting that acupuncture plus rehabilitation and sole use of rehabilitation both can improve the swallow ing function in the patients w ith post-stroke deglutition disorder of qi-deficiency blood stasis pattern.There were no significant differences in the KWST and FILS score between after treatment and at the follow-up in the two groups (allP>0.05), indicating that the improvement of swallow ing function managed to maintain for 1 month after the term ination of treatment.Meanwhile, we conducted pairw ise comparisons of the TCM symptoms score at the three different time points in the two groups and found that the TCM symptoms score showed significant improvement in the observation group (P<0.05), while the improvement in the rehabilitation group was insignificant (P>0.05). There were significant differences in the KWST, FILS and TCM symptoms score between the two groups after treatment and at the follow-up (allP<0.05),demonstrating that acupuncture plus rehabilitation won out the sole use of acupuncture in improving the swallow ing function and TCM symptoms,together w ith more significant long-term efficacy.
This clinical trial was conducted in multiple centers.However, lim ited by the study duration, this study was designed w ith a rather small sample size and short efficacy observation time. These shortcom ings should be overcome in the future studies.

Conflict of Interest The authors declare that there is no potential conflict of interest in this article.Acknow ledgments This work was supported by Research Projects of Shanghai Science and Technology Committee (上海市科学技术委员会科研计划项目,No.16401970402,No.18401970601),Shanghai Municipal Health and Fam ily Planning Comm ission Research Project [上海市卫生和计划生育委员会项目,No.ZY(2018-2020)-CCCX-1005];Shanghai Municipal Health Commission Research Project (上海市卫生健康委员会科研课题计划项目,No.20204Y0470).Statement of Informed Consent Informed consent was obtained from all individual participants.
Received:22 January 2020/Accepted:19March 2020
 Journal of Acupuncture and Tuina Science2020年5期
Journal of Acupuncture and Tuina Science2020年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation on electroacupuncture plus Yi Jin Jing (Sinew-transform ing Qigong Exercises) for knee osteoarthritis
- Clinical efficacy comparison of moxibustion w ith different doses for knee osteoarthritis
- Clinical observation of acupuncture and traction plus Ba Duan Jin (Eight-brocade Exercise) for improving discogenic low back pain
- Clinical observation on acupoint injection for back pain in patients w ith primary osteoporosis
- Clinical observation on Yi Jin Jing(Sinew-transform ing Qigong Exercises) plus tuina on the neck for stiff neck
- Clinical observation of acupuncture plus Frenkel exercises for ataxia after cerebral stroke
