Corneal perforation and rare primary adenocarcinoma of the lacrimal gland: A case report
Sunny, Chi Lik Au, Edwin Chan, Simon, Tak Chuen Ko
Department of Ophthalmology, Tung Wah Eastern Hospital, Hong Kong, China
ABSTRACT Rationale: Primary adenocarcinoma of the lacrimal gland is rare, and its presentation as corneal perforation is even rarer.Corneal perforation is an ocular emergency that warrants urgent ophthalmic surgery, yet complete staging of lacrimal gland tumor pre-operatively is essential for optimal oncological management.Patient’s concerns: A 57-year-old man presented with left eye pain was found to have left eye proptosis and fleshy tissue mass around the eyeball. Uveal tissue was prolapsing over the perforated keratitis cornea, and the eye was full of discharge.Diagnosis: Bedside ultrasound B-scan confirmed vitreous haze,and emergency contrast computed tomography (CT) revealed soft tissue density mass (>40 mm) molding around the left globe and optic nerve without any rim enhancing abscess. Left exogenous endophthalmitis from exposure keratopathy secondary to proptosis caused by the bulky lacrimal tumor located in the confined orbital cone was diagnosed.Interventions: Emergency enucleation surgery of the left eyeball was done for this painful blind eye to control the infection from spreading. Orbital walls were biopsied intra-operatively, and tumor staging was completed by positron emission tomography-CT scan and magnetic resonance imaging. Without evidence of metastasis, left orbital exenteration was followed by adjuvant orbital chemoradiotherapy for the sake of close proximity of resection margin.Outcomes: Left exenterated orbit was fully epithelialized at around 2 months, and there was no recurrence of the disease up to present at the 1 year follow-up.Lessons: Thorough workup on the staging of the disease to minimize the number of operations for oncological patients is always a top priority, yet it may not always be possible as in our case presenting with corneal perforation.
KEYWORDS: Lacrimal apparatus; Adenocarcinoma; Orbital neoplasms; Corneal perforation; Keratitis; Eye enucleation
1. Introduction
Lacrimal gland tumor uncommonly can cause eye complications that present as an ophthalmological emergency[1], such as rupture globe or endophthalmitis, when a definite histological diagnosis of the radiological staging of the lacrimal gland tumor becomes impractical before the emergency eye operation. Here we present the challenges on managing a case of late presentation of nonmetastatic primary adenocarcinoma of the lacrimal gland.
2. Case report
Informed consent was obtained from the patient. A 57-yearold man presented to the hospital on 10th May 2019 for left eye pain. Visual acuity of the left eye was no light perception and Snellen decimal 0.7 for the right eye. Ophthalmological examinations showed left eye proptosis with ugly looking fleshy tissue mass around the eyeball (Figure 1). The cornea was not well identified, with lots of discharge and uveal tissue prolapsing over the disorganized cornea (Figure 1). Keratitis was prominent, and bedside ultrasound B-scan confirmed endophthalmitis. Emergency contrast computed tomography (CT) revealed soft tissue density mass (>40 mm) molding around the left globe and optic nerve(Figure 2). There was a loss of the entire anterior chamber of the eye, but the preservation of the natural lens (Figure 3). Rim enhancing abscess was absent.

Figure 1. Clinical photo of the left eye showing fleshy tissue mass covering up the normal sclera. The corneal is disorganised and coated with exudate,and the uveal tissue is prolapsed over the cornea.
Emergency enucleation surgery of the left eyeball was done for this painful blind eye to control the infection from spreading(Figure 4 and Figure 5). Orbital biopsy intra-operatively revealed moderately differentiated adenocarcinoma, positive for Cytokeratin 7,weakly positive for BRST-2 and GATA3, and negative for cytokeratin 20, prostate-specific antigen, and thyroid transcription factor-1. Immunohistochemical studies showed positivity for the mammaglobin androgen receptor, but negative for estrogen receptor and c-erbB2. Secondary orbital metastasis from breast or lung was unlikely, and there was no lymphovascular nor perineural invasion on the pathological examinations (Figure 4).
The patient’s private CT films two years ago from another hospital were only available after the first surgery. A smaller molding soft tissue mass over the left superotemporal orbit was presented already. It was not roundish in shape, and there was no capsule, nor indentation into the globe. The patient denied previous incisional biopsy of the lesion elsewhere; therefore, malignant transformation of pleomorphic adenoma, the commonest lacrimal gland epithelial origin tumor[2] was excluded.
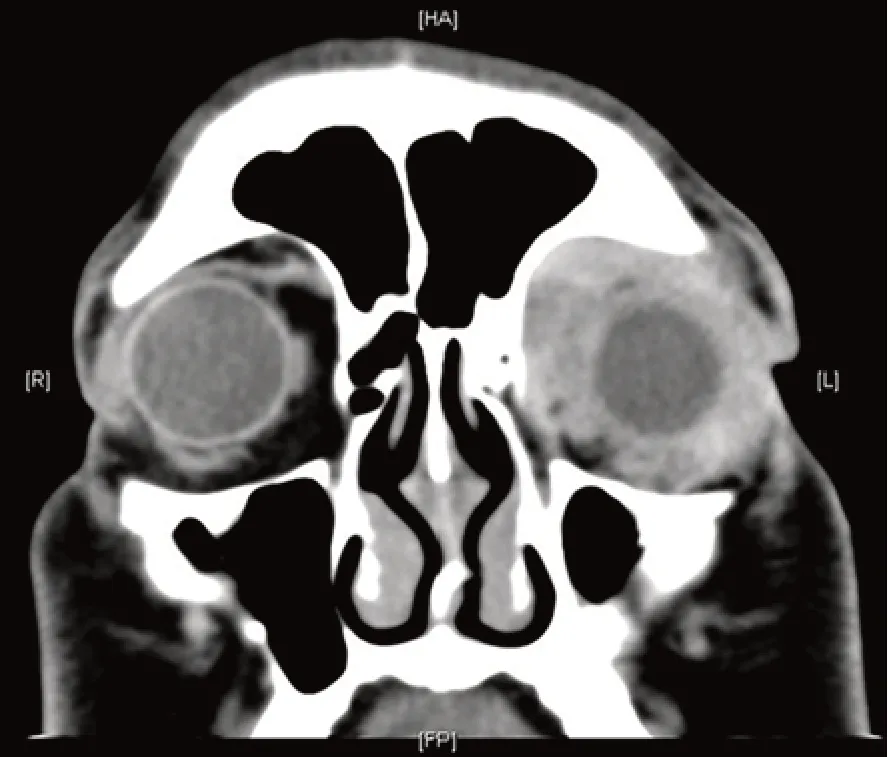
Figure 2. Coronal cut of computed tomography of the orbit showing diffuse soft tissue mass molding around the left globe and occupied the left orbital cone pushing the left globe forward to give proptosis.
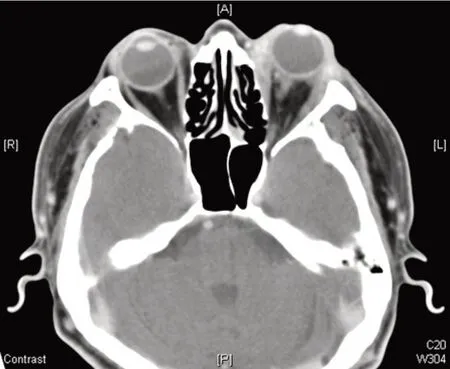
Figure 3. The transverse cut of computed tomography of the orbit showing left eye proptosis with loss of anterior chamber space. Right eye anterior chamber, i.e. the intraocular soft tissue density space anterior to the natural lens, is preserved as in normal eyes.
Post-operatively, a proper staging of disease was completed with imaging. Positron emission tomography-CT scan and magnetic resonance imaging (MRI) showed no lymph node or other organs involvement, nor metastasis out of the orbit into the cranial cavity,but large residual primary tumor (>40 mm) hindering success of radiotherapy (Figure 6). The patient underwent left orbital exenteration subsequently, excision was down to the orbital bone with a skin-sparing approach, and remained skin flap of ~1 cm in length was sutured to the orbital bone to promote granulation of the deep socket, for earliest possible radiotherapy subsequently(Figure 7). Pathological examinations of the exenteration specimen revealed a tumor edge of <1 mm, but clear, from excision margin.When the orbital exenteration wound was fully epithelialized at around 2 months post-operatively, the MRI showed no residual tumor (Figure 8). The patient then underwent adjuvant orbital chemoradiotherapy for the sake of close proximity of resection margin; 66 Gy in 30 fractions were delivered over 6 weeks with 3 cycles of cisplatin every 3 weeks. There was no recurrence of the disease up to present at the 1 year follow-up.
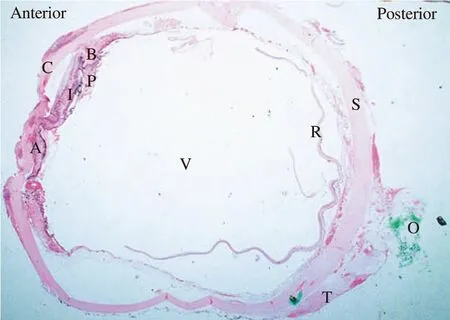
Figure 4. Histological slide of the enucleated eyeball in horizontal cut stained with haematoxylin and eosin (×5 magnification). A: Peripheral anterior synechiae; B: Ciliary body; C: Cornea; I: Iris; O: Optic nerve; P:Ciliary process; R: Retina; S: Sclera; T: Tumour; V: Vitreous.
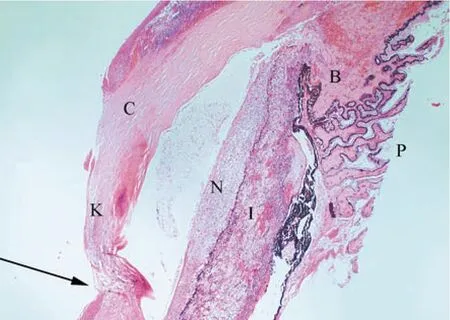
Figure 5. Enlarged view over the disorganised anterior chamber of the enucleated eye (×40 magnification). B: Ciliary body; C: Cornea; I: Iris;K: Keratitis (a cornea with inflammatory cells infiltrate); N: Collection of neutrophils in front of the iris; P: Ciliary process; Black arrow indicats the corneal melting down to perforation site.

Figure 6. Post-enucleation magnetic resonance imaging for staging of left lacrimal gland tumour. This transverse cut T2 image over orbit demonstrated large residual tumour was located over the left orbit with the eyeball removed.

Figure 7. Clinical appearance of the left empty orbital socket after exenteration surgery. The skin flap is sutured onto the orbital bone raw area(red area) to promote healing.

Figure 8. Post-exenteration magnetic resonance imaging of the orbit. This transverse cut of short inversion time inversion recovery sequence over the orbit shows left empty orbital cavity, with no residual tumour.
3. Discussion
Malignant lacrimal gland tumor is rare[3], and randomized controlled trial on best treatment approaches and modalities is lacking in the literature. Most reported literature was retrospective case series only. With a predominance of lymphoid type of malignant tumors over lacrimal gland, carcinoma is even rarer[3].The commonest benign tumor of epithelial origin in lacrimal gland is pleomorphic adenoma[4], whereas malignant adenocarcinoma of lacrimal gland usually arises from malignant changes of benign pleomorphic adenoma, either spontaneously or from incomplete excision[4]. Secondary metastasis, such as from breast was reported.As biopsy tract seeding followed by malignant transformation is possible, incisional biopsy is contraindicated in suspected pleomorphic adenoma of the lacrimal gland[4], and complete excisional biopsy together with its pseudo-capsule is suggested[5].In our case, there was no clinical or radiological evidence to suggest a previous benign pleomorphic adenoma, and secondary lacrimal gland metastasis was excluded by histopathological tests. Therefore,the rare entity of primary adenocarcinoma of lacrimal gland was concluded.
Thorough workup on the staging of the disease to minimize the number of operations for oncological patients is always a top priority[2]; yet corneal perforation, no matter traumatic or inflammatory cause, is an ophthalmological emergency[6]. This patient unluckily suffered from exposure keratopathy secondary to proptosis caused by the bulky lacrimal tumor located in the confined orbital cone, and the exposure keratitis was so severe to cause exogenous endophthalmitis. Without visual potential, the eyeball was enucleated in emergency surgery setting to eliminate the septic source, and to protect the only useful right eye of the patient from sympathetic ophthalmia[7]. The nasty eye condition challenged the surgeons, and forced the patient inevitably to undergo a 2-staged operation, both requiring general anesthesia. Classic teaching on orbital exenteration surgery includes three approaches: partial thickness skin graft to the orbital raw area, free flap reconstruction to fill up the hollow orbit, or leaving bare area heals by granulation in months[8]. In our case with inadequate resection margin, orbital local recurrence was a major concern. The free flap would block the clinical view for detecting early tumor recurrence, and is relatively contraindicated in our case of dirty orbit started with infection; whereas healing by granulation would hinder early orbital radiotherapy. Skin graft remained the only option, yet the patient refused another surgical wound over the back or thigh area.
If there was no corneal perforation, this bulky orbital lacrimal gland tumor could have been worked upon metastasis with complete tumor staging, before proceeding to an elective singlestaged orbital exenteration surgery. Given the huge psychological impact of enucleation or exenteration surgery on one’s appearance,the fundamental question of eye-sparing surgery for the lacrimal gland tumor evolves. The literature on eye-sparing surgery for lacrimal gland tumor almost predominantly focused on adenoid cystic carcinoma[9], with only a handful of cases within different series on adenocarcinoma[9]. These adenocarcinoma cases were not separately analyzed for survival or recurrence benefit for eye-sparing surgery, thus a valid conclusion could not be drawn from the current literature. Besides, publication bias on this rare disease entity is significant. Despite all these, eye-sparing surgery was impossible in our case, as corneal perforation with endophthalmitis was of guarded visual potential[10].
In conclusion, we reported a rare case of lacrimal gland primary adenocarcinoma and its unusual rare presentation as an ophthalmic emergency with the perforated cornea. Challenges existed for diagnosing and managing such an extensive and complicated orbital tumor, which unavoidably required a 2-staged surgery.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
S.C.L.A.: Concept and design of the study, acquisition of data,drafting the article. E.C.: performing the surgery, acquisition of data, revising the article critically for important intellectual content.S.T.C.K.: Revising article critically for important intellectual content.
 Journal of Acute Disease2020年5期
Journal of Acute Disease2020年5期
- Journal of Acute Disease的其它文章
- Using point-of-care ultrasound in ocular emergencies: A mini review
- Coronavirus disease 2019 (COVID-19), MERS and SARS: Similarity and difference
- An epidemiological report on the burden and trend of injuries in the Philippines from 2011 to 2018
- Epidemiological profile and management of acute pyelonephritis in the emergency department of a tertiary hospital: A retrospective observational study
- Evaluation of the neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and monocyte lymphocyte ratio for diagnosis of testicular torsion
- Effect of proximal femur nail anti-rotation on unstable intertrochanteric fractures: A prospective observational study
