Epidemiological profile and management of acute pyelonephritis in the emergency department of a tertiary hospital: A retrospective observational study
Eduardo Esteban-Zubero, Marta Jordán-Domingo, Alberto García-Noain, Francisco José Ruiz-Ruiz
1Emergency Department, Hospital San Pedro, Logroño, Spain
2Emergency Department, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain
ABSTRACT Objective: To assess the clinical and microbiological characteristics as well as the risk factors of early readmission(<72 h) in acute pyelonephritis (APN) patients discharged from emergency department (ED).Methods: The medical records of patients discharged with a diagnosis of APN between January 1, 2014 and December 31, 2015 were reviewed. Epidemiological, clinical, ultrasound results, and laboratory characteristics were collected, and the risk factors of prompt readmission and non-prompt readmission were assessed.Results: A total of 423 APN patients were included. The mean age was (44.3±19.0) years. The bulk of the patients were women(79.9%), and 20% of cases had episodes previously. Urine cultures were requested in 77.5% of cases, with Escherichia coli being the most frequently isolated bacterium (80.1%). Resistance to one or more antibiotics was found in 68.1% of the bacteria. The most widely used antibiotics were beta-lactam with beta-lactamases inhibitor (46%), and aminoglycosides in 24.4% of cases.Altogether, 73.5% of the patients received antibiotic treatment in the ED, and 46.8% of the patients were discharged. Furthermore,6.1% of the patients discharged from the ED had re-admission without associated risk factors.Conclusions: Given the high rate of resistance, it is important to know the profile of antibiotics in different areas. Likewise, the administration of antibiotics in the ED is useful in the prevention of early readmissions of APN (<72 h).
KEYWORDS: Acute pyelonephritis; Emergencies; Resistances;Antibiotics; Re-admission
1. Introduction
Urinary tract infections (UTIs) are one of the most common reasons for admissions in emergency departments (ED). In the United States, it is responsible for more than 2 million visits a year,which represents 2% of all visits[1]. UTIs, after upper and lower respiratory infections, are the most common infectious disease in the ED, accounting for 22% of all infections and 3% of all pathologies in the ED[2]. Acute pyelonephritis (APN) is a serious UTI. APN usually manifests with signs and symptoms of systemic inflammation (including fever, chills, and general malaise) and localized inflammation at the bladder level (for example, increased urinary frequency, urgency, and dysuria). However, there is a lack of consensus on the diagnostic criteria[3]. Clinical presentations and severity of the disease vary greatly, from mild flank pain with low or no fever to septic shock[4].
The aetiology of the UTI is influenced by many factors, including age, sex, gestation, the presence of comorbidities such as diabetes mellitus, use of the urinary catheter, and immunological status.Furthermore, previous exposure to antibiotics and a history of recent hospital admission may affect the etiological profile[5]. The main causal bacterium of APN isEscherichia coli(E. coli), followed by other Gram-negative bacteria such asKlebsiella spp. andProteus mirabilis. Among the Gram-positive bacteria, the most common isStaphylococcus saprophyticus, followed by enterococci andStreptococcus agalactiae[6,7]. Regarding the recurrences, infection withE. coliis of the highest rate[8].
To reduce symptoms and avoid possible complications, antibiotic treatment is usually empirically in the ED. It is because that the etiological spectrum, such as antibiotic sensitivity, is highly predictable. However, in recent years, more studies are concentrated on strains resistant to one or more of those frequently used antibiotics[9,10]. Thus, local microbiological epidemiology and resistance monitoring are important. This may differ due to age and associated risk factors. For example, the causative bacteria can vary between a young woman with no medical history and an elderly,immunosuppressed patient with a permanent bladder catheter[11].
It is reported that the use of antimicrobials needs improvement in many hospitals (30%-60% of cases)[12-14]. And the resistance varies in different geographic areas[15]. The inappropriate use of antibiotics causes problems in patients in two ways: causing novel toxicity(adverse reactions) and modifying their microbiota, which favors the multi-resistant strains[16,17]. They cause an increase in medical costs.Some observational studies have reported that adverse effects related to antibiotics have attracted more attention in the ED[18,19].
To date, the loss of sensitivity to antibiotics has been mitigated with the development of new antibiotics. But it is believed that this longterm model is not sustainable since the time required to discover new treatments is longer than the evolution time of new resistant strains[20]. This study aims to assess the epidemiological situation of APN as well as the antibiotic resistance pattern in our hospital.
2. Patients and methods
2.1. Study design
The study was carried out at the University Hospital Lozano Blesa in Zaragoza. It is a public general hospital and is the reference health center for an area of 275 000 inhabitants. A retrospective observational study was designed. The included patients were over 14 years of age with a diagnosis of APN on discharge from ED between 2014 and 2015 (590.1, 590.11, 590.8 as a primary or secondary diagnosis were included in ICD-9, 9th revision).
2.2. Ethical approval
The study was authorized by the Internal Ethical Committee of Clinical Research of the Emergency Department of University Hospital Lozano Blesa (N. HCU-20160201p).
2.3. Inclusion and exclusion criteria
Patients over 14 years old and diagnosed as APN were included in this study. The presence of the two following symptoms and/or signs was defined as APN: (1) Axillary temperature ≥38 ℃; (2) Renal/ureteral flank pain; (3) Pyuria, defined as ≥10 leukocytes/mL in urine without centrifugation. Otherwise, Patients with cystitis, urethritis,or prostatitis were excluded.
2.4. Data collection
Data were obtained from the electronic medical history of patients. The data included: (1) Sex and age; (2) Recent urological manipulation (<7 d); (3) Predisposing factors such as a history of APN, diabetes mellitus, immunosuppression, chronic renal failure;(4) Previous antibiotic treatment; (5) Physical examination in the ED; (6) Other comorbidities including dementia, permanent urinary catheter, neoplasias,etc.; (7) Ultrasonography results;(8) Microbiological tests, including urine culture and blood culture.If the results of the uroculture and blood cultures were discordant,the aetiology of was determined based on the microorganism isolated in the blood culture; (9) Antibiotic resistance of isolated bacteria or urine cultures as well as blood cultures; (10) Antibiotic administered in the ED (if it was performed) as well as the antibiotic prescription; (11) Readmissions in the ED, which was defined as prompt readmissions (<72 h) and non-prompt readmissions (<7 d).
The following indicators were also studied: (1) Percentage of hospitalizations; (2) Microbiological tests obtained during the episode (urocultures and blood cultures); (3) Pattern of antibiotic use during APN episodes in the ED; (4) Adequacy of antibiotic empirical treatment; (5) Risk factors associated with ED readmissions.
The following outcome indicators were evaluated: (1) Percentage of patients discharged from the ED; (2) Percentage of readmissions;(3) Result of the microbiological tests as a positive percentage in cultures and blood cultures.
2.5. Statistical analysis
Statistical analysis was performed using the statistical software IBM®SPSS version 22. Qualitative variables were expressed as absolute and relative frequencies. The association was analyzed using theChi-square test and the Fisher exact test. The significant level of the test was set at α<0.05.
3. Results
The study included 423 APN patients, among which 338 were women (79.9%) and 85 were men (20.1%). The mean age was(44.3±19.0) years. Besides, 31.4% of the patients had taken antibiotics before admission to the ED (n=133).
Table 1 shows the epidemiological, clinical, ultrasound results, and laboratory characteristics of the patients. Regarding comorbidities, diabetes mellitus was the most frequently observed(20.1%,n=28). The most observed alteration in the ultrasound image was lithiasis (15.9%,n=52). The most isolated bacterium in urine cultures as well as blood cultures wasE. coli. The prevalence was 80.1% (n=173) and 74.1% (n=20), respectively. Antibiotic resistance was tested in 68.1% of positive urine cultures, with quinolones the most observed (30.6%,n=45).
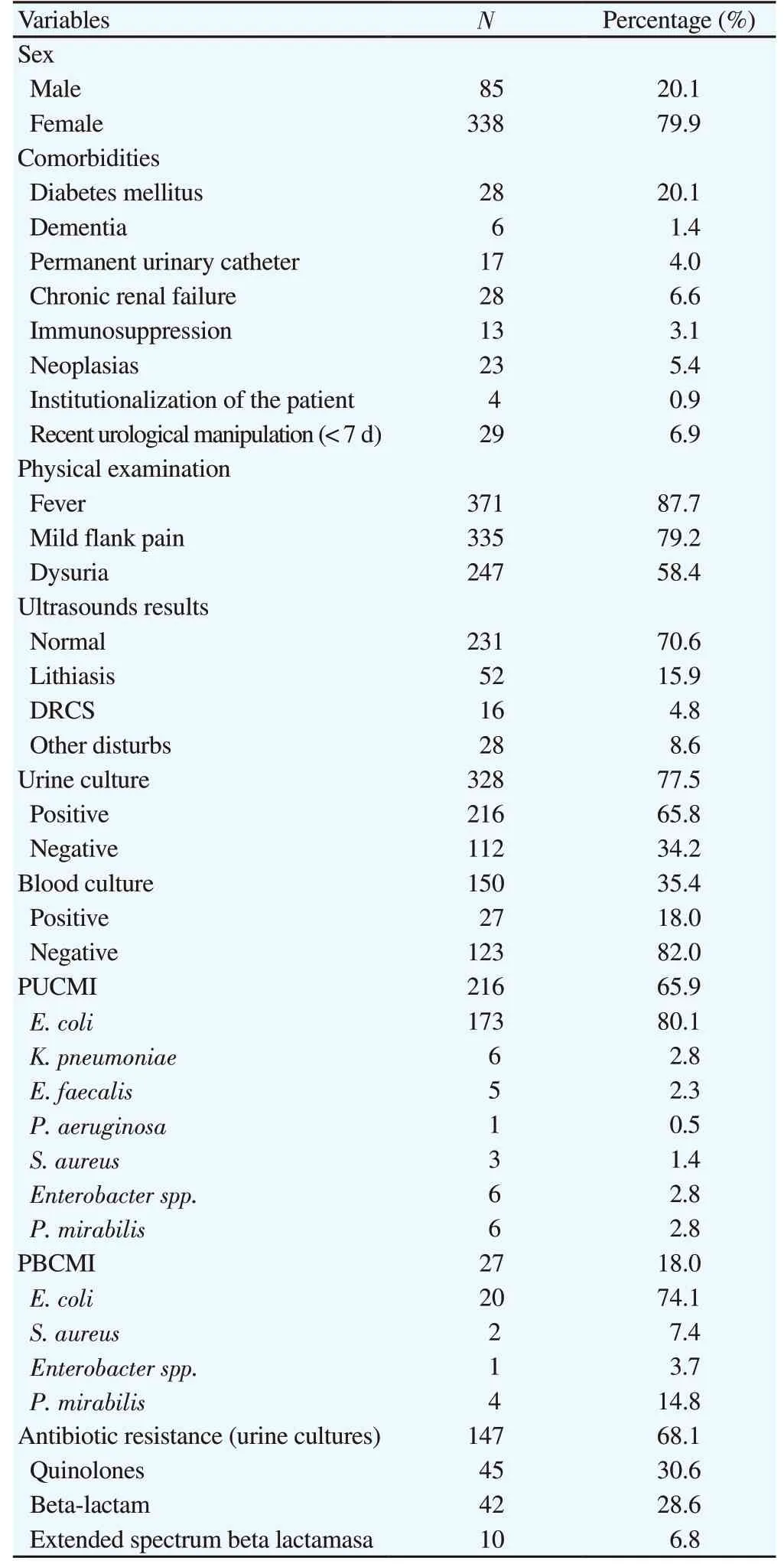
Table 1. Baseline information and laboratory characteristics of the patients.

Table 2. Process indicators of acute pyelonephritis.
In our study, 73.5% of the patients received antibiotic treatment in the ED. Table 2 shows the process indicators and the percentage of admissions was 20.3% (n=86). Beta-lactams with beta-lactamase inhibitors were the most administered antibiotic (46%,n=143)and the initial empiric treatment used aminoglycoside mostly in 24.4% (n=76), which was similar to the antibiotic prescription on discharge (Table 2).
The total percentage of prompt readmissions (<72 h) was 6.1%(n=26), whereas non-prompt readmissions was 4% (n=17). Of both groups, 48.8% of the patients (n=21) were discharged from the ED.And antibiotic administration in the ED provided protective effect against recurrence (P<0.05) (Table 3 and Table 4).
4. Discussion
The present study highlighted the high frequency ofE. colias a causative agent of APN as well as the high resistance to one or more antibiotics. Sampling for microbiological tests should be improved since urine culture was not performed in more than 20%of cases. It showed that cephalosporins third generation and betalactam antibiotics are used more frequently for the treatment of APNs. This study does not show any differences in comorbidity or type of bacteria involved, which is mainly because APN itself is a high risk of complications. For patients without risks of severe APN, the administration of intravenous antibiotics was useful in preventing prompt readmissions (<72 h).

Table 3. Risk factors for prompt readmission in the ED (< 72 h).
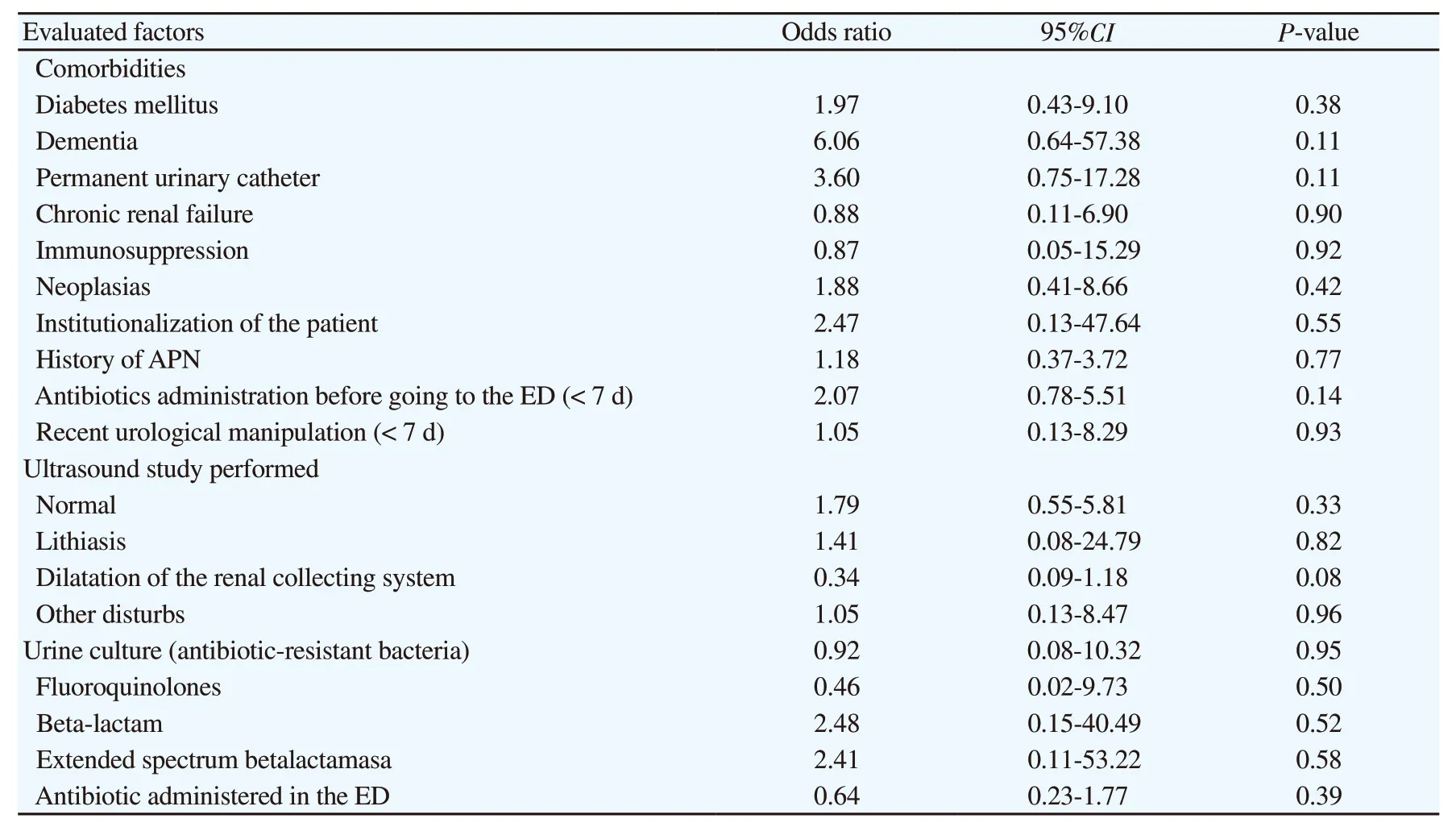
Table 4. Risk factors for non-prompt readmission in the ED (< 7 d).
One of the limitations of this study is failed to assess the association between the administration time of antibiotics and the possibility of readmission. Many studies have shown that delayed antibiotic treatment led to worse results in cases of sepsis or bacteremia[21,22]. However, rare literature studied the relationship in the cases of APN. Naucléret al.observed that the severity of the symptoms and comorbidities are the only factors related to the prognosis of APN, while other scholars found different factors such as delayed initiation or empirical use of antibiotic-therapy in an erroneous way[23].
With respect to the risk factors of APN, though the result is not significant (P=0.85), the medical history of APN is a valuable factor (20.6%). This is in line with previous studies[5,24]. Moreover,it has been suggested that cystitis (caused by sexual activity,new sexual partner, exposure to spermicide,etc.) is a potential risk of APN. However, less than 3% of asymptomatic cystitis or bacteriuria cases were found to progress to APN[3,25]. Other relative factors are pregnancy, mechanical obstructions, genetic predisposition, a high microbiological load, the virulence of the pathogen, vesicoureteral reflux, and diabetes mellitus possibly[2,26].
Microbiological studies are vital for the effective diagnosis and treatment of APN[4]. Urine cultures were only requested in 77.5%of patients in our study. As a confirmatory test, urine culture is helpful for effective antibiotic therapys[2,27]. However, the application of urine culture is not enough in our study, far from the optimal usage rate (greater than 90%)[5,24,28]. One of the reasons is 31.4% of patients received antibiotics application 7 d before the test, which could influence the results of tests[5].
In our study, the most frequently isolated bacterium by urine culture wasE. coli(80.1%). This bacterium is most related to the development of APN and urinary tract infection[4,5-7,24,27,28].E. coliusually present in the anal flora and can be transmitted through direct contact[29]. Blood cultures were performed in 35.4% of the patients, which is similar to previous studies[2,27]. AndE. coliis also the most frequently isolated bacterium as previously reported[5,24,27,28].
A total of 68.1% (n=147) of urine cultures showed at least one antimicrobial resistance. Quinolone resistance was the most frequent (30.6%,n=45), which is higher than some previous studies[6,7,30,31]. However, in Spain, the rate of quinolone resistance is increased[5], due to the abuse use of drugs in the treatment of UTI. There are different methods to assess the risk of resistance to antibiotics[32]. Association is observed between resistance and the comorbidities[33], which may be also observed in other antibiotics such as penicillin[33]. The high rate of resistance to quinolones (and other antibiotics) is due to empirical antibiotic therapy, inefficient control of infections in the hospital setting, low adherence to treatment, and poor hygiene.
The specific resistance to ciprofloxacin is also related to chromosomal mutations that alter DNA gyrase and topoisomeraseⅣ, overexpress efflux pumps, alter the number of porin types,and transfer the resistance through the genes of the plasmids[6,34].Some risk factors lead to the delevopment of ESBL-producing germs an APN[35]. It is important to note that despite the apparent complexity of these illnesses due to the antibiotic resistance,no worse prognosis has been observed[36]. Likewise, common antibiotic therapy rather than a selective one in the suspected ESBL cases is most likely to have poor effectiveness and worse prognosis.Therefore, some authors suggested avoiding broad-spectrum drugs in the first line but choosing a specific antibody based on the urine culture to avoid resistance[37].
Only a few pieces of literature focused on the timely application of antibiotics therapy of APN or UTI, especially in patients with sepsis and other significant comorbidities[23]. The most prescribed antibiotic was beta-lactam with beta-lactamases inhibitor (46%) followed by cephalosporins 3rd generation(34.4%). Aminoglycoside was used in 24.4% of the cases. In some studies, cephalosporins were the most prescribed treatment[2,27].In recent years, there is a new tendency to administer betalactam with beta-lactamases inhibitor as the first choice in cases of APN[31]. It should be noted that the use of aminoglycoside was more prevalent in our center than in other places[2,27]. This may be because first-line treatments have high resistance, and aminoglycoside can increase efficacy[38]. Recent studies also show that the administration of aminoglycoside can improve symptoms or shorten in-hospital stay in patients with sepsis of urinary origin or APN[39].
Finally, our results showed that 46.8% of patients were discharged, higher than other studies[2]. Our data may be biased since the comorbidities or the severity of each condition are different. Moreover, The results showed that 6.1% of the cases had early readmission into the ED (<72 h) and 4.2% cases <7 d,which is similar to previous studies[40-43]. Of all these factors, only the administration of antibiotics in the ED showed a significant preventive effect. Poor response to symptomatic treatment and the inadequacy of the antibiotic therapy are influencing factors of early readmission[28,42]. Fully response and effective antibiotic therapy can not only achieve a better prognosis but also be economically efficient[40]. Antibiotics were prescribed to discharged patients in our study, which is similar to other studies[31] and 3rd generation cephalosporin was prescribed before discharge in another study[44].
In conclusion,E. coliis the most frequent causal bacterium of APN in our ED. A total of 68.1% of the cases showed resistance to one or more antibiotics. Finally, the administration of antibiotics in the ED before discharge has a significant protective effect from early readmissions (<72 h).
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
A.G.N., F.J.R.R.: Concepts, design, definition of intelectual content and data analysis. E.E.Z., M.J.D.: Literature search, experimental studies and data acquistion. F.J.R.R.: Statistical analysis. E.E.Z.:Manuscript preapration and editing. All the authors: Clinical studies and manuscript review.
 Journal of Acute Disease2020年5期
Journal of Acute Disease2020年5期
- Journal of Acute Disease的其它文章
- Using point-of-care ultrasound in ocular emergencies: A mini review
- Coronavirus disease 2019 (COVID-19), MERS and SARS: Similarity and difference
- An epidemiological report on the burden and trend of injuries in the Philippines from 2011 to 2018
- Evaluation of the neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and monocyte lymphocyte ratio for diagnosis of testicular torsion
- Effect of proximal femur nail anti-rotation on unstable intertrochanteric fractures: A prospective observational study
- Antibacterial activity of plant extracts in different solvents against pathogenic bacteria: An in vitro experiment
